Abstract
Chemokines are key regulators of both innate and adaptive immune responses. CCL4 (macrophage inflammatory protein-1β, MIP-1β) is a CC chemokine that has a broad spectrum of target cells including immature dendritic cells, which express the cognate receptor CCR5. We asked whether a plasmid encoding CCL4 is able to improve tumor protection and immune responses in a Her2/neu+ mouse tumor model. Balb/c mice were immunized twice intramuscularly with plasmid DNA on days 1 and 15. On day 25, a tumor challenge was performed with 2 × 105 syngeneic Her2/neu+ D2F2/E2 tumor cells. Different groups of mice were vaccinated with pDNA(Her2/neu) plus pDNA(CCL4), pDNA(Her2/neu), pDNA(CCL4) or mock vector alone. Our results show that CCL4 is able to (i) improve tumor protection and (ii) augment a TH1-polarized immune response against Her2/neu. Although Her2/neu-specific humoral and T-cell immune responses were comparable with that induced in previous studies using CCL19 or CCL21 as adjuvants, tumor protection conferred by CCL4 was inferior. Whether this is due to a different spectrum of (innate) immune cells, remains to be clarified. However, combination of CCL19/21 with CCL4 might be a reasonable approach in the future, particularly for DNA vaccination in Her2/neu+ breast cancer in the situation of minimal residual disease.
Similar content being viewed by others
Introduction
DNA vaccination using plasmid DNA encoding a particular antigen is a vaccination strategy which is used both in infectious disease and in cancer.1, 2, 3, 4, 5, 6 Despite strong immunogenicity in mice, the efficacy of DNA vaccines in large animals and humans has been disappointing so far.7 Therefore, during the past decades, different strategies have been pursued to improve efficacy of DNA vaccines, including the coadministration of immunomodulatory molecules as genetic adjuvants.8, 9
Chemokines are key regulators of immune responses and may orchestrate the interactions and the migration of different immune cells during innate and adaptive immune responses. Therefore, chemokines are among these different immunomodulatory molecules that have been studied as adjuvants for different vaccination strategies both in infectious disease and in cancer.10, 11, 12, 13, 14, 15 As CCR7 agonists, such as CCL19 and CCL21, have a central role for interactions between dendritic cells (DC) and naive T cells in the immunological synapse, these chemokines have been in the focus of animal models by several groups including ours. Meanwhile, there is a large body of evidence showing that the use of CCL19 or CCL21 as adjuvant for vaccines is able to enhance TH1-polarized immune responses and to protect mice from tumor growth or viral infection.16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
CCL4 (macrophage inflammatory protein-1β, MIP-1β) is a CC chemokine that belongs to the group of inflammatory chemokines and acts as a chemoattractant for different immune effector cells such as immature DC, TH1 T cells, NK cells and monocytes. In contrast to CCR7 that is expressed on mature DC and naive T-cell subsets, the CCL4 receptor CCR5 is expressed on immature DC and TH1-polarized T cells.10, 29 Consequently, it has to be assumed that—when applied as an adjuvant during DNA vaccination—the spectrum of immune cells recruited by CCL4 and CCL19/21 will be clearly distinct from each other and thus may induce different immunological effector mechanisms. In this study, we asked whether CCL4 is able to enhance the efficacy of a Her2/neu DNA vaccine in a mouse tumor model, in which syngeneic Her2/neu tumor cells are used for tumor challenge experiments.
Materials and methods
Animals
Female 6–8-week-old BALB/c mice (H-2kd) mice were purchased from Charles River (Sulzfeld, Germany) and housed in our animal facility (Max Delbrück Center for Molecular Medicine (MDC), Berlin, Germany) under standard pathogen-free conditions. Experiments were approved by local authorities (LAGeSo, Berlin, Germany) and were performed in accordance with German animal protection law.
Cell line
Mouse mammary tumor cell line D2F2 is derived from a spontaneous mouse mammary tumor, which arose in a BALB/c background from the hyperplastic alveolar nodule cell line D2. The cells were kindly provided by Dr S Preise and Dr T Kammertoens (MDC). The cell line and culture conditions have previously been described.22, 23, 30, 31
Plasmids
pVax was purchased from Invitrogen (Carlsbad, CA, USA). pDNA(Her2/neu) encoding human Her2/neu was kindly provided by Dr S Preise and Dr T Kammertoens (MDC). The Her2/neu plasmid pVax/E2A contains the E2A gene from pCMV/E2A, which was cloned into the expression vector pVax. E2A contains a lysine to alanine mutation in nucleotide sequence position 2257-2258, which corresponds to position 753 of the amino acid sequence. This alteration leads to the elimination of tyrosine signaling in the Her2/neu proto-oncogene, which is an important issue under safety aspects for a potential clinical vaccine development. The plasmids were amplified in E. coli X1-blue strain (Agilent Technologies, Waldbronn, Germany) and purified using the EndoFree Giga-Prep-Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions.
Murine CCL4 (MIP-1β) was synthesized and optimized for expression in mammalian cells by GeneArt (Regensburg, Germany) with NotI and XbaI as indicators and cloned into the cloning sites KpaI and SacI of the vector pGA4. The CCL4 gene was then subcloned into the cloning site NotI and XbaI of pVax (Invitrogen) (Figure 1a). The plasmid was amplified and purified as described above. Appropriate insertion of the CCL4 gene into pVax was confirmed by restriction enzyme analysis with NotI and XbaI (Figure 1b).
CCL4 expression in murine NIH 3T3 cells
Murine NIH 3T3 cells were transfected with pVax (CCL4) by electroporation. CCL4- transfected NIH 3T3 cells were cultured for 24–48 h in Dulbecco's modified Eagle's medium (Life Technologies, Karlsruhe, Germany). Cell culture supernatant and the adherent cells were collected separately to analyze the expression of CCL4 protein by ELISA (supernatant) and western blot (cell lysate). CCL4-transfected NIH 3T3 cells were lysed and used for western blot analysis. Biotinylated anti-murine CCL4 antibody (BFA 451, R&D, Abingdon Science Park, UK) were used together with Streptavidin-HRP and an ELC plus detection kit (Amersham Pharmacia Biotech, Piscataway, NJ, USA). CCL4 in the cell culture supernatant was quantified by an ELISA Kit (R&D) according to the manufacturer’s instructions. The lower detection limit of the assay was 3 pg ml−1.
Immunization and tumor challenge protocol
Mice were injected twice intramuscularly with 100 μg of plasmid DNA on days 1 and 15. Each experimental group consisted of 8–10 mice. Mice were injected with pDNA(Her2/neu) plus pDNA(CCL4), pDNA(Her2/neu), pDNA(CCL4) or mock vector alone. On day 25, the immunized mice were challenged subcutaneously with 2 × 105 Her2/neu+ syngeneic D2F2/E2 tumor cells. Tumor growth was subsequently observed. Progressively growing masses >1 mm in mean diameter were defined as tumors. Tumor diameters were measured one to two times weekly by calipers. Tumor volumes were calculated according to the formula tumor volume=1/6 π d3 (d=diameter). On day 30, sera and splenocytes were collected for the different immunological assays.23
ELISpot
Enzyme-linked immunospot (ELISpot) assays were performed with splenocytes from vaccinated mice as previously described.22, 23, 30 Briefly, spleens were aseptically removed and a single cell suspension was generated in complete medium. Splenocytes were seeded in triplicates (2 × 105 splenocytes per well) on an γ-interferon- or IL-4-precoated ELISpot plate (ELISpot Kit, Pharmingen, Heidelberg, Germany) and restimulated by the following Her2/neu peptides: (i) peptides derived from the extracellular domain (Her2/neu-ECD): a/ Her2p63-71: TYLPTNASL, b/ Her2p342-350: CYGLGMEHL, c/ Her2p369-377: KIFGSLAFL, d/ Her2p440-448: AYSLTLQGL; (ii) peptides derived from the intracellular domain (Her2/neu-ICD): a/ Her2p773-782: VMAGVGSPYV, b/ Her2p780-788:PYVSRLLG, c/ Her2-2p883-899 KVPIKWMALESILRRRF, d/ Her2p907-915: SYGVTVWEL. Kd restriction and potential immunogenicity in mice has previously been shown for most of these peptides.32, 33, 34 Using the BIMAS epitope prediction algorithm (www.bimas.cet.nih.gov), most peptides are high affinity binders for Kd. Only peptides 1c, 2a and 2c are predicted to have a low affinity for Kd. All peptides were purchased from Wita GmbH (Berlin, Germany) and had a purity of >95%. Peptides were added at a concentration of 100 ng per well. Incubation was performed overnight and ELISpot plates were developed according to the manufacturer’s instructions. Evaluation was performed by means of an ImmunoSpot reader system (ImmunoSpot, Cellular Technology Ltd., Bonn, Germany). Antigen-specific responses were defined as having (i) a ratio of specific peptide: control⩾2 and (ii) an absolute number of spots >20. Results were expressed as 'spots per 106 splenocytes'.
Humoral anti-Her2/neu immune responses
Flow cytometric assays were performed as previously described.22, 23, 31 Briefly, frozen sera were thawed and subsequently diluted in phosphate-buffered saline (PBS; 1:30, 1:60 and 1:120). Sera were then incubated with 3–5 × 105 SK-BR-3 cells for 30–60 min at 4 °C. After that time, cells were washed twice with PBS. Pellets were resuspended in PBS containing 50 μl of biotinylated anti-mouse IgG1, IgG2a, IgG2b, IgG3 (dilution 1:50) (BD Pharmingen, San Diego, CA, USA). Cells were incubated for 30–60 min at 4 °C, washed twice with fluorescence-activated cell sorting buffer and resuspended in PBS containing 50 μl of streptavidin-APC (BD Pharmingen) (dilution 1:200). Cells were incubated for 15–30 min at 4 °C, washed with fluorescence-activated cell sorting buffer and resuspended in 200 μl fluorescence-activated cell sorting buffer (1 × PBS containing 0.5% bovine serum albumin, 2 mM EDTA, 0.05% NaN3) for flow cytometric analysis. Relative quantification of anti-Her2/neu serum IgG1, IgG2a, IgG2b and IgG3 was performed by comparing the mean channel fluorescence in the different samples. Mean channel fluorescence reflects the binding of anti-Her2/neu antibodies to SK-BR3 cells and is therefore a suitable parameter for the quantification of humoral anti-Her2/neu immune responses.22, 23, 30
Statistical methods
For comparison of the means of three or more groups, analysis of variance was used together with PRISM software. Student’s t-test was used to compare the means between two groups. A P-value<0.05 was considered statistically significant.
Results
Transfected CCL4 is expressed in NIH 3T3 cells and secreted into the supernatant
To confirm the expression of CCL4 on a protein level, murine NIH 3T3 cells were transfected with pDNA(CCL4) by electroporation. Cell lysates of the transfected cells as well as supernatant from the cell culture were used for western blot and ELISA to detect CCL4 protein. Our results show that CCL4 protein is not only expressed on a cellular level, moreover, substantial secretion into the supernatant could be detected. Slightly increasing amounts of CCL4 protein were observed over the first 48 h after transfection (Figures 2a and b).
CCL4 expression in murine NIH 3T3 cells. Murine NIH 3T3 cells were transfected with pDNA(CCL4) by electroporation. (a) Expression of CCL4 protein was detected by western blot in cell lysates 24 and 48 h after transfection. (b) Secretion of CCL4 into the cell culture supernatant was detected 24 and 48 h after transfection. Results are representative for three independent experiments.
CCL4 as an adjuvant is able to improve the protective immunity of a DNA vaccine against Her2/neu+ tumors
To study CCL4 as an adjuvant for Her2/neu DNA vaccination, mice (n=8–10 per group) were immunized intramuscularly with plasmid DNA on days 1 and 15, and tumor challenge with syngeneic Her2/neu+ D2F2/E2 tumor cells was performed on day 25. Vaccination with pDNA(Her2/neu) plus pDNA(CCL4) was compared with pDNA(Her2/neu), control groups were injected with pDNA(CCL4) or mock vector (pVax) alone.
The percentages of tumor-free mice as well as tumor growth were monitored thereafter. Coexpression of CCL4 as an adjuvant together with the Her2/neu DNA vaccine was able to increase the percentage of tumor-free mice as compared with pDNA(Her2/neu) alone.
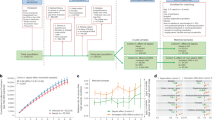
On day 38 after tumor challenge, 26% of the mice immunized with pDNA(Her2/neu) plus pDNA(CCL4) remained tumor-free as compared with 13% of mice in the group that had been vaccinated with pDNA(Her2/neu) alone (P<0.05). In contrast, all of the mice immunized with pDNA(CCL4) or mock vector developed a tumor (P<0.05). Results are depicted in Figure 3a. Improved tumor protection by the adjuvant use of CCL4 was not only reflected by the percentage of tumor-free animals, but also by the tumor growth slope in immunized animals: there was a substantial retardation of tumor growth in the group of animals that had been vaccinated with pDNA(Her2/neu) plus pDNA(CCL4) as compared with all control groups (P<0.05). Results are shown in Figure 3b.
Improved tumor protection after coadministration of CCL4 as an adjuvant for Her2/neu DNA vaccination. Mice were immunized with pDNA(Her2/neu) plus pDNA(CCL4), pDNA(Her2/neu), pDNA(CCL4) or mock vector on days 1 and 15. On day 25, tumor challenge was performed with 2 × 105 Her2/neu+ syngeneic D2F2/E2 tumor cells. Tumor growth was monitored thereafter. Data are representative for two independent experiments. (a) Coexpression of CCL4 was able to improve tumor protection of the immunized animals (n=8–10 for each group of mice). (b) In the same experimental setting, the tumor growth slope was observed over 30 days after DNA vaccination. Coexpression of CCL4 led to a significant retardation of tumor growth as compared with all control groups (P<0.05). *P<0.05 as compared with all other groups. **P<0.05 as compared with pDNA(CCL4) and mock vector.
CCL4 induces a TH1-polarized anti-Her2/neu T-cell response
Induction of an anti-Her2/neu T-cell response was evaluated in the same experimental setting. Mice that had been vaccinated with pDNA(Her2/neu) plus pDNA(CCL4) were compared with pDNA(Her2/neu), pDNA(CCL4) and mock vector alone.
Splenocytes from the vaccinated mice were prepared on day 5 after the tumor challenge and were analyzed by IFN-γ and IL-4 ELISpot assays using peptides from the intracellular and/or extracellular domain of Her2/neu for restimulation. Our results show that two vaccinations with pDNA(Her2/neu) are not sufficient to induce a significant anti-Her2/neu T-cell response, which is in line with our previous studies in this mouse model.21, 22, 23 In contrast, coadministration of CCL4 led to a strong TH1-polarized anti-Her2/neu immune response. As previously shown,21, 22, 23 the T-cell response was directed against peptides from the extracellular domain of Her2/neu. T cells showed a predominant TH1 cytokine profile with peptide-specific γ-IFN-release (Figure 4a), whereas IL-4-ELISpots were always negative (Figure 4b).
Anti-Her2/neu T-cell immune response after vaccination. Splenocytes from vaccinated mice were stimulated with different peptides from the extracellular or the intracellular domain of Her2/neu. Her2/neu-specific T-cell responses were analyzed by γ-IFN- (a) and IL-4-ELISpot (b). The mice had been immunized with DNA on days 1 and 15 and challenged on day 25 with the 2 × 105 D2F2/E2 Her2/neu+ tumor cells. ELISpot assays were performed 5 days after the tumor challenge. For ELISpot assays, splenocytes in the different groups of mice were pooled. Data are representative for two independent experiments. *P<0.05 as compared with all control groups.
Induction of a humoral anti-Her2/neu immune responses by CCL4 as an adjuvant
In the same groups of mice that had been immunized with pDNA(Her2/neu) plus pDNA(CCL4), pDNA(Her2/neu), pDNA(CCL4) or mock vector (pVax) alone, anti-Her2/neu antibodies (IgG1, IgG2a, IgG2b and IgG2b isotypes) were quantified in the serum of the animals as described in materials and methods. There was a strong induction of anti-Her2/neu antibodies with an IgG2a isotype and—to a lesser extent—an IgG3 isotype, whereas anti-Her2/neu antibodies of the subclasses IgG1 and IgG2b were not elevated over background levels (Figure 5). These results are consistent with a TH1-polarized immune response and therefore fit very well with the data obtained from the ELISpot assays.
Induction of a humoral anti-Her2/neu immune response after vaccination. Mice were immunized with pDNA(Her2/neu) plus pDNA(CCL4), pDNA(Her2/neu), pDNA(CCL4) or mock vector on days 1 and 15. On day 25, tumor challenge was performed with 2 × 105 Her2/neu+ syngeneic D2F2/E2 tumor cells. Antibody responses against Her2/neu (IgG1 (a); IgG2a (b); IgG2b (c) and IgG3 (d)) were analyzed on day 5 after the tumor challenge. The different colors of the bars indicate different dilutions: white bar: 1:30, gray bar: 1:60, black bar: 1:120. Data are representative for two independent experiments. *P<0.05 as compared with all control groups.
Discussion
During the past decade, it has become increasingly evident that chemokines may serve as adjuvant for both innate and adaptive immune responses.8, 9, 10, 11, 12, 13, 30, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46 As tumor vaccination is mainly focused on the induction of T-cell responses, chemokines such as CCL19 and CCL21(refs. 14, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28) are of particular interest because of their chemoattractant capacity with regard to mature DC and naive T cells within the immunological synapse.14, 15
In this study, we were able to demonstrate that CCL4, a CC chemokine with a completely different spectrum of target cells (immature DC, TH1-polarized T cells, NK cells and monocytes, which all express the cognate receptor CCR5) is also able to amplify antigen-specific T-cell responses. Moreover, the adjuvant effect of CCL4 led to an inhibition of tumor growth in our syngeneic Her2/neu mouse tumor model. After successful transfection, the chemokine is secreted into the environment, which is assumed to be a prerequisite for the attraction of immune effector cells. CCL4 is able to enhance (i) a Her2/neu-specific T-cell and antibody response, and (ii) the protection from tumor growth in tumor challenge experiments. In our mouse tumor model, the amplification of both the anti-Her2/neu-directed T-cell response and the antibody response induced by CCL4 was in the same order of magnitude or even higher than it had been observed using CCL19 or CCL21 as adjuvants.22, 23 As we have previously described,22, 23 the anti-Her2/neu T-cell response was again directed against peptides from the extracellular domain of Her2/neu, whereas peptides from the intracellular Her2/neu domain were not recognized (Figure 4). Although the application of CCL4 led to comparable anti-Her2/neu immune responses, protection from tumor growth after a tumor challenge with syngeneic Her2/neu+ tumor cells (26% tumor-free mice) was lower than that observed in the same mouse tumor model with CCL19 (58% tumor-free mice) or CCL21 (38% tumor-free mice).22, 23 It is very difficult—if possible at all—to dissect the underlying immunological mechanisms, which are responsible for these differences. This is because of the fact that the chemokines act on many different immune cells and that the effects are partly interdependent. This interdependency becomes clear considering the interactions of DC and T cells. Therefore, even experiments in knockout mice or after depletion of particular subsets of immune cells (which are far beyond the scope of this study) will presumably not be able to give clear-cut answers with regard to the observed differences in chemokine-induced anti-tumor responses. However, it is tempting to speculate that the observed differences might basically be explained in two different ways: (i) although the analysis of Her2/neu-specific immune responses suggests largely comparable efficacy of CCL4, CCL19 and CCL21, there might be differences with regard to epitope specificity and/or functional activity of the T cells/antibodies that are induced. These differences might result in different anti-tumor activity and, moreover, the T-cell specificities detected in vitro might not completely reflect the true rejection epitopes in vivo. Therefore, the in vitro assays can only be considered as 'surrogate parameter' for the emerging anti-Her2/neu immune response in vivo; (ii) despite comparable Her2/neu-specific immune responses (T-cell and humoral responses) with CCL4, CCL19 and CCL21, the observed differences in tumor protection may be attributed to a different spectrum of innate effector cells such as NK cells, neutrophils and monocytes/macrophages, which are attracted by these three chemokines. Curcio et al.47 have previously demonstrated in a Her2/neu-transgenic mouse model that the extent of vaccine-induced protection from tumor growth is largely the sum of different antigen-specific and non-specific mechanisms, involving T cells, B cells, neutrophils and macrophages. In line with these results, the different expression pattern of the chemokine receptors CCR5 (ligand: CCL4) and CCR7 (ligand: CCL19 and CCL21) might very well explain a varying contribution of these different innate and adaptive effector mechanisms during Her2/neu DNA vaccination with chemokines as adjuvants. Finally, CCL19 and CCL21 affect T-cell immunity primarily by creating a chemokine gradient towards lymphatic tissues leading to an interaction of CCR7+ mature, antigen-loaded DC and CCR7+ naive T cells within the immunological synapse.48, 49 In contrast, the effect of CCL4 on T-cell immune responses might rather rely on a recruitment of CCR5+ immature DC at the injection site. This may result in an enhancement of antigen uptake because the antigen (in our study Her2/neu) is locally overexpressed in the muscle tissue. Subsequently, and after maturation, which is supported by vaccine-derived CpG sequences, these Her2/neu-loaded DC migrate into the draining lymph nodes and elicit Her2/neu-specific immune responses.
In conclusion and somewhat unexpectedly, our present study shows that—in comparison with CCL19 and CCL21—the use of CCL4 (targeting mainly immature DC) does not impair Her2/neu-specific immune responses in as far as they are detectable in vitro.
In the literature, data on the effect of CCL4 in the context of vaccination are very scarce. Lillard et al.29 reported on the differential effects of CCL3 and CCL4 on humoral and T-cell immune responses against ovalbumin in a mouse model for mucosal immunization. They were able to show that the administration of CCL4 leads to an enhancement of both humoral and (CD4) T-cell responses against ovalbumin. However, to the best of our knowledge, this is the first study using plasmid-encoded CCL4 as an adjuvant for a DNA vaccine in a mouse tumor model. Although tumor protection by CCL4 is inferior to CCL19 and CCL21 in our Her2/neu mouse tumor model, our study shows the ability of CCL4 to amplify a TH1-polarized anti-Her2/neu immune response. Therefore, CCL4 as an adjuvant is an interesting combination partner for CCL19 or CCL21. The most appropriate clinical perspective for such a genetic Her2/neu vaccine with chemokines as adjuvant might be Her2/neu-positive breast cancer in the situation of minimal residual disease after surgery or successful systemic therapy. Combination with immune checkpoint inhibitors such as anti-PD1 antibodies might further increase immunogenicity of the DNA vaccine.
References
Gurunathan S, Klinman DM, Seder RA . DNA vaccines: immunology, application and optimization. Annu Rev Immunol 2000; 18: 927–974.
Choo AY, Choo DK, Kim JJ, Weiner DB . DNA vaccination in immunotherapy of cancer. Cancer Res 2005; 123: 137–156.
Kutzler MA, Weiner DB . Developing DNA vaccines that call to dendritic cells. J Clin Invest 2004; 114: 1241–1244.
Rice J, Ottensmeier CH, Stevenson F . DNA vaccines: precision tools for activating Effective immunity against cancer. Nat Rev Immunol 2008; 8: 108–120.
Prud’homme G . DNA vaccination against tumors. J Gene Med 2005; 7: 3–17.
Iezzi M, Quaglino E, Amici A, Lollini P, Forni G, Cavallo F . DNA vaccination against oncoantigens.A promise. OncoImmunology 2012; 1: 316–325.
Babiuk LA, Pontarollo R, Babiuk S, Loehr B, van Drunen Littel-van den Hurk S . Induction of immune responses by DNA vaccines in large animals. Vaccine 2003; 21: 649–658.
Scheerlinck JP . Genetic adjuvants for DNA vaccines. Vaccine 2001; 19: 2647–2656.
Greenland JR, Letvin NL . Chemical adjuvants for plasmid DNA vaccines. Vaccine 2007; 25: 3731–3741.
Stewart TJ, Smyth MJ . Chemokine-chemokine receptors in cancer immunotherapy. Immunother 2009; 1: 109–127.
Bobanga ID, Petrosiute, Huang AY . Chemokines as cancer vaccine adjuvants. Vaccines 2013; 1: 444–462.
Allen SJ, Crown SE, Handel TM . Chemokine: receptor structure, interactions, and antagonism. Annu Rev Immunol 2007; 25: 787–920.
Homey B, Müller A, Zlotnik A . Chemokines: agents for the immunotherapy of cancer? Nat Rev immunol 2002; 2: 175–184.
Bromley SK, Mempel TR, Luster AD . Orchestrating the orchestrators: chemokines in control of T cell traffic. Nat Immunol 2008; 9: 970–980.
Viola A, Contento RL, Molon B . T cells and their partners: the chemokine dating agency. Trends Immunol 2006; 27: 421–427.
Eo SK, Lee S, Kumaraguru U, Rouse BT . Immunopotentiation of DNA vaccine against herpes simplex virus via co-delivery of plasmid DNA expressing CCR7 ligands. Vaccine 2001; 19: 4685–4693.
Toka FN, Gierynska M, Rouse BT . Codelivery of CCR7 ligands as molecular adjuvants enhances the protective immune response against herpes simplex virus type 1. J Virol 2003; 77: 12742–12752.
Braun SE, Chen K, Foster RG, Kim CH, Hromas R, Kaplan MH et al. The CC chemokine CK beta-11/MIP-3 beta/ELC/Exodus 3 mediates tumor rejection of murine breast cancer cells through NK cells. J Immunol 2000; 164: 4025–4031.
Hillinger S, Yang SC, Zhu L, Huang M, Duckett R, Atianzar K et al. EBV-induced molecule 1 ligand chemokine (ELC/CCL19) promotes IFN-gamma-dependent antitumor responses in a lung cancer model. J Immunol 2003; 171: 6457–6465.
Hillinger S, Yang SC, Batra RK, Striete RM, Weder W, Dubinett SM et al. CCL19 reduces tumour burden in a model of advanced lung cancer. Br J Cancer 2006; 94: 1029–1034.
Westermann J, Nguyen-Hoai T, Baldenhofer G, Höpken UE, Lipp M, Dörken B et al. CCL19 (ELC) as an adjuvant for DNA vaccination: induction of a TH1-type T-cell response and enhancement of antitumor immunity. Cancer Gene Ther 2007; 14: 523–532.
Nguyen-Hoai T, Baldenhofer G, Ahmed MS, Pham-Duc M, Gries M, Lipp M et al. CCL19 (ELC) improves TH1-polarized immune responses and protective immunity in a murine Her2/neu DNA vaccination model. J Gene Med 2012; 14: 128–137.
Nguyen-Hoai T, Baldenhofer G, Sayed Ahmed MS, Pham-Duc M, Lipp M, Dörken B et al. CCL21 (SLC) improves tumor by a DNA vaccine in a Her2/neu mouse tumor model. Cancer Gene Ther 2012; 19: 69–76.
Sharma S, Stolin M, Luo J, Strieter RM, Burdick M, Zhu LX et al. Secondary Lymphoid tissue chemokine mediates T cell-dependent antitumor responses in vivo. J Immunol 2000; 164: 4558–4563.
Sharma S, Stolina M, Zhu L, Lin Y, Batra R, Huang M et al. Secondary lymphoid organ chemokine reduces pulmonary tumor burden in spontaneous murine bronchoalveolar cell carcinoma. Cancer Res 2001; 61: 6406–6412.
Yang SC, Hillinger S, Riedl K, Zhang L, Zhu L, Huang M et al. Intratumoral administration of dendritic cells overexpressing CCL21 generates systemic antitumor responses and confers tumor immunity. Cancer Res 2004; 10: 2891–2901.
Yang SC, Batra RK, Hillinger S, Reckamp KL, Strieter RM, Dubinett SM et al. Intrapulmonary administration of CCL21 gene-modified dendritic cells reduces tumor burden in spontaneous murine bronchoalveolar cell carcinoma. Cancer Res 2006; 66: 3205–3213.
Qin H, Zhou C, Wang D, Ma W, Liang X, Lin C et al. Enhancement of antitumour immunity by a novel chemotactic antigen DNA vaccine encoding chemokines and multiepitopes of prostate-tumour-associated antigens. Immunology 2006; 117: 419–430.
Lillard JW, Singh UP, Boyaka PN, Singh S, Taub DD, McGhee JR . MIP-1a and MIP-1b differentially mediate mucosal and systemic adaptive immunity. Blood 2003; 101: 807–814.
Nguyen-Hoai T, Hohn O, Vu MD, Baldenhofer G, Sayed Ahmed MS, Dörken B et al. CCL19 as an adjuvant for intradermal gene gun immunization in a Her2/neu mouse tumor model: improved vaccine efficacy and a role for B cells as APC. Cancer Gene Ther 2012; 19: 880–887.
Lindencrona JA, Preiss S, Kammertoens T, Schuler T, Piechocki M, Wie WZ et al. CD4+T cell-mediated HER-2/neu-specific tumor rejection in the absence of B cells. Int J Cancer 2004; 109: 259–264.
Nagata Y, Furugen R, Hiasa A . Peptides derived from a wild-type murine proto-oncogene c-erbB-2/HER2/neu can induce CTL and tumor suppression in syngeneic hosts. J Immunol 1997; 159: 1336–1343.
Correa I, Plunkett T . Update on HER-2 as a target for cancer therapy: HER2/neu peptides as tumour vaccines for T cell recognition. Breast Cancer Res 2001; 3: 399–403.
Vertuani S, Sette A, Sidney J . Improved immunogenicity of an immunodominant epitope of the HER-2/neu protooncogene by alterations of MHC contact residues. J Immunol 2004; 172: 3501–3508.
Chen D, Murphy B, Sung R, Bromberg JS . Adaptive and innate immune responses to gene transfer vectors: role of cytokines and chemokines in vector function. Gene Ther 2003; 10: 991–998.
Novak L, Igoucheva O, Cho S, Alexeev V . Characterization of the CCL21-mediated melanoma-specific immune responses and in situ melanoma eradication. Mol Cancer Ther 2007; 6: 1755–1764.
Thanarajasingam U, Sanz L, Diaz R, Qiao J, Sanchez-Perez L, Kottke T et al. Delivery of CCL21 to metastatic disease improves the efficacy of adoptive T-cell therapy. Cancer Res 2007; 67: 300–308.
Song R, Liu S, Leong KW . Effects of MIP-1 alpha, MIP-3 alpha, and MIP-3 beta on the induction of HIV Gag-specific immune response with DNA vaccines. Mol Ther 2007; 15: 1007–1015.
Song JH, Kim JI, Kwon HJ, Shim DH, Parajuli N, Cuburu N et al. CCR7- CCL19/CCL21-regulated dendritic cells are responsible for effectiveness of sublingual vaccination. J Immunol 2009; 182: 6851–6860.
Song S, Liu C, Wang J, Zhang Y, You H, Wang Y et al. Vaccination with combination of Flt3L and RANTES in a DNA prime-protein boost regimen elicits strong cell mediated immunity and antitumor effect. Vaccine 2009; 27: 1111–1118.
Rainone V, Dubois G, Temchura V, Uberla K, Clivio A, Nebuloni M et al. CCL28 Induces Mucosal Homing of HIV-1-Specific IgA-Secreting Plasma Cells in Mice Immunized with HIV-1 Virus-Like Particles. PLoS One 2011; 6: e26979.
Kar UK, Srivastava MK, Andersson A, Baratelli F, Huang M, Kickhoefer V et al. A Novel CCL21-vault nanocapsule intratumoral delivery inhibits lung cancer growth. PLoS One 2011; 6: e18758.
Franciszkiewicz K, Boissonnas A, Boutet M, Combadiere C, Mami-Chouai F . Role of chemokines and chemokine receptors in shaping the effector phase of the antitumor immune response. Cancer Res 2012; 72: 6325–6332.
Igoucheva O, Jonas R, Alexeev V . Chemokine-enhanced DNA vaccination in cancer immunotherapy. Oncoimmunology 2013; 2: e26092.
Yan YH, Qi SC, Su LK, Xu QA, Fan MW . Co-delivery of ccl19 gene enhances anti-caries DNA vaccine pCIA-P immunogenicity in mice by increasing dendritic cell migration to secondary lymphoid tissues. Acta Pharmacol Sin 2013; 34: 432–440.
Hartoonian C, Sepehrizadeh Z, Tabatabai Yazdi M, Jang YS, Langroudi L, Amir Kalvanagh P et al. Enhancement of immune responses by co-delivery of CCL19/MIP-3beta chemokine plasmid with HCV core DNA/protein immunization. Hepat Mon 2014; 14: e14611.
Curcio C, Di Carlo E, Clynes R, Smyth MJ, Boggio K, Quaglino E et al. Nonredundant roles of antibody, cytokines, and perforin in the eradication of established Her-2/neu carcinomas. J Clin Invest 2003; 111: 1161–1170.
Bachmann MF, Kopf M, Marsland BJ . Chemokines: more than just road signs. Nat Rev Immunol 2006; 6: 159–164.
Wuest TR, Carr DJ . The role of chemokines during herpes simplex virus-1 infection. Front Biosci 2008; 13: 4862–4872.
Acknowledgements
This study was partially supported by a generous grant by 'Music against Cancer e.V.'
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nguyen-Hoai, T., Pham-Duc, M., Gries, M. et al. CCL4 as an adjuvant for DNA vaccination in a Her2/neu mouse tumor model. Cancer Gene Ther 23, 162–167 (2016). https://doi.org/10.1038/cgt.2016.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2016.9
This article is cited by
-
The future of cancer immunotherapy: DNA vaccines leading the way
Medical Oncology (2023)
-
Cancer DNA vaccines: current preclinical and clinical developments and future perspectives
Journal of Experimental & Clinical Cancer Research (2019)
-
Recent developments in targeted imaging of CXCR4-chemokine receptor
Journal of Radioanalytical and Nuclear Chemistry (2018)
-
Synergistic effect of programmed cell death protein 1 blockade and secondary lymphoid tissue chemokine in the induction of anti-tumor immunity by a therapeutic cancer vaccine
Archives of Virology (2017)