Abstract
Nowadays, allogeneic haematopoietic stem cell transplantation (allo-HSCT) is a well-established treatment procedure and often the only cure for many patients with malignant and non-malignant diseases. Decrease in short-term complications has substantially contributed to increased survival. Therefore long-term sequelae are reaching the focus of patient care. One of the most important risks of stem cell transplant survivors is infertility. As well as in the field of allo-HSCT also the field of reproductive medicine has achieved substantial advances to offer potential options for fertility preservation in both boys and girls. Access to these procedures as well as their financing differs significantly throughout Europe. As all European children and adolescents should have the same possibility, the Paediatric Diseases Working Party of the European Society for Blood and Marrow Transplantation organised an expert meeting in September 2015. This manuscript describes the recommendations for the diagnosis and pre-emptive procedures that should be offered to all children and adolescents in Europe who have to undergo an allo-HSCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
European Society for Blood and Marrow Transplantation. Annual Report, 2014. EBMT: Leiden, The Netherlands, 2014. https://www.ebmt.org/Contents/Resources/Library/Annualreport/Documents/EBMT_AnnualReport_2014.pdf.
Borgmann-Staudt A, Rendtorff R, Reinmuth S, Hohmann C, Keil T, Schuster FR et al. Fertility after allogeneic haematopoietic stem cell transplantation in childhood and adolescence. Bone Marrow Transplant 2012; 47: 271–276.
Lambertini M, Del Mastro L, Pescio MC, Andersen CY, Azim HA Jr, Peccatori FA et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med 2016; 14: 1.
Assouline E, Crocchiolo R, Prebet T, Broussais F, Coso D, Gamerre M et al. Impact of reduced-intensity conditioning allogeneic stem cell transplantation on women's fertility. Clin Lymphoma Myeloma Leuk 2013; 13: 704–710.
Panasiuk A, Nussey S, Veys P, Amrolia P, Rao K, Krawczuk-Rybak M et al. Gonadal function and fertility after stem cell transplantation in childhood: comparison of a reduced intensity conditioning regimen containing melphalan with a myeloablative regimen containing busulfan. Br J Haematol 2015; 170: 719–726.
Lawrenz B, Jauckus J, Kupka MS, Strowitzki T, von Wolff M . Fertility preservation in >1,000 patients: patient's characteristics, spectrum, efficacy and risks of applied preservation techniques. Arch Gynecol Obstet 2011; 283: 651–656.
Picton HM, Wyns C, Anderson RA, Goossens E, Jahnukainen K, Kliesch S et al. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys. Hum Reprod 2015; 30: 2463–2475.
Demeestere I, Simon P, Dedeken L, Moffa F, Tsepelidis S, Brachet C et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. Hum Reprod 2015; 30: 2107–2109.
Schmidt KT, Larsen EC, Andersen CY, Andersen AN . Risk of ovarian failure and fertility preserving methods in girls and adolescents with a malignant disease. BJOG 2010; 117: 163–174.
Donnez J, Dolmans MM . Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J Assist Reprod Genet 2015; 32: 1167–1170.
Jadoul P, Dolmans MM, Donnez J . Fertility preservation in girls during childhood: is it feasible, efficient and safe and to whom should it be proposed? Hum Reprod Update 2010; 16: 617–630.
Poirot CJ, Martelli H, Genestie C, Golmard JL, Valteau-Couanet D, Helardot P et al. Feasibility of ovarian tissue cryopreservation for prepubertal females with cancer. Pediatr Blood Cancer 2007; 49: 74–78.
Rosendahl M, Schmidt KT, Ernst E, Rasmussen PE, Loft A, Byskov AG et al. Cryopreservation of ovarian tissue for a decade in Denmark: a view of the technique. Reprod Biomed Online 2011; 22: 162–171.
Liebenthron J, Dittrich R, Toth B, Korell M, Krüssel J, Van der Ven K et al. Orthotopic ovarian tissue transplantation - results in relation to experience of the transplanting centers, overnight tissue transportation and transplantation into the peritoneum. Hum Reprod 2015; 30 (Suppl 1): i97–i98.
Jensen AK, Kristensen SG, Macklon KT, Jeppesen JV, Fedder J, Ernst E et al. Outcomes of transplantations of cryopreserved ovarian tissue to 41 women in Denmark. Hum Reprod 2015; 30: 2838–2845.
Dittrich R, Lotz L, Fehm T, Krussel J, von Wolff M, Toth B et al. Xenotransplantation of cryopreserved human ovarian tissue—a systematic review of MII oocyte maturation and discussion of it as a realistic option for restoring fertility after cancer treatment. Fertil Steril 2015; 103: 1557–1565.
Luyckx V, Scalercio S, Jadoul P, Amorim CA, Soares M, Donnez J et al. Evaluation of cryopreserved ovarian tissue from prepubertal patients after long-term xenografting and exogenous stimulation. Fertil Steril 2013; 100: 1350–1357.
Telfer EE, Zelinski MB . Ovarian follicle culture: advances and challenges for human and nonhuman primates. Fertil Steril 2013; 99: 1523–1533.
Ernst E, Kjaersgaard M, Birkebaek NH, Clausen N, Andersen CY . Case report: stimulation of puberty in a girl with chemo- and radiation therapy induced ovarian failure by transplantation of a small part of her frozen/thawed ovarian tissue. Eur J Cancer 2013; 49: 911–914.
Poirot C, Abirached F, Prades M, Coussieu C, Bernaudin F, Piver P . Induction of puberty by autograft of cryopreserved ovarian tissue. Lancet 2012; 379: 588.
Nakagawa K, Kanda Y, Yamashita H, Nakagawa S, Sasano N, Ohtomo K et al. Ovarian shielding allows ovarian recovery and normal birth in female hematopoietic SCT recipients undergoing TBI. Bone Marrow Transplant 2008; 42: 697–699.
von Wolff M, Dittrich R, Liebenthron J, Nawroth F, Schuring AN, Bruckner T et al. Fertility-preservation counselling and treatment for medical reasons: data from a multinational network of over 5000 women. Reprod Biomed Online 2015; 31: 605–612.
Knight S, Lorenzo A, Maloney AM, Srikanthan A, Donen R, Greenblatt E et al. An approach to fertility preservation in prepubertal and postpubertal females: a critical review of current literature. Pediatr Blood Cancer 2015; 62: 935–939.
Oktay K, Bedoschi G . Oocyte cryopreservation for fertility preservation in postpubertal female children at risk for premature ovarian failure due to accelerated follicle loss in Turner syndrome or cancer treatments. J Pediatr Adolesc Gynecol 2014; 27: 342–346.
Huober-Zeeb C, Lawrenz B, Popovici RM, Strowitzki T, Germeyer A, Stute P et al. Improving fertility preservation in cancer: ovarian tissue cryobanking followed by ovarian stimulation can be efficiently combined. Fertil Steril 2011; 95: 342–344.
Turan V, Bedoschi G, Moy F, Oktay K . Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril 2013; 100: 1681–5 e1.
Adank MC, van Dorp W, Smit M, van Casteren NJ, Laven JS, Pieters R et al. Electroejaculation as a method of fertility preservation in boys diagnosed with cancer: a single-center experience and review of the literature. Fertil Steril 2014; 102: 199–205 e1.
Meistrich ML, Shetty G . Hormonal suppression for fertility preservation in males and females. Reproduction 2008; 136: 691–701.
Jahnukainen K, Mitchell RT, Stukenborg JB . Testicular function and fertility preservation after treatment for haematological cancer. Curr Opin Endocrinol Diabetes Obes 2015; 22: 217–223.
Sato T, Katagiri K, Gohbara A, Inoue K, Ogonuki N, Ogura A et al. In vitro production of functional sperm in cultured neonatal mouse testes. Nature 2011; 471: 504–507.
Article 32. Journal Officiel de la République Française 2011; L. 2141-11. http://www.ccne-ethique.fr/sites/default/files/joe_20110708_0157_0001.pdf.
Muller J, Sonksen J, Sommer P, Schmiegelow M, Petersen PM, Heilman C et al. Cryopreservation of semen from pubertal boys with cancer. Med Pediatr Oncol 2000; 34: 191–194.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dalle, JH., Lucchini, G., Balduzzi, A. et al. State-of-the-art fertility preservation in children and adolescents undergoing haematopoietic stem cell transplantation: a report on the expert meeting of the Paediatric Diseases Working Party (PDWP) of the European Society for Blood and Marrow Transplantation (EBMT) in Baden, Austria, 29–30 September 2015. Bone Marrow Transplant 52, 1029–1035 (2017). https://doi.org/10.1038/bmt.2017.21
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.21
This article is cited by
-
Fertilitätserhalt – State of the Art in Österreich
Journal für Gynäkologische Endokrinologie/Österreich (2023)
-
Recommendations on hematopoietic stem cell transplantation for patients with Diamond–Blackfan anemia. On behalf of the Pediatric Diseases and Severe Aplastic Anemia Working Parties of the EBMT
Bone Marrow Transplantation (2021)
-
Gene therapy using haematopoietic stem and progenitor cells
Nature Reviews Genetics (2021)
-
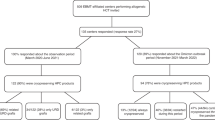
How can fertility counseling be implemented for every newly diagnosed pediatric patient facing gonadotoxic treatment?-A single-center experience
Annals of Hematology (2021)
-
Urogenital Abnormalities in Adenosine Deaminase Deficiency
Journal of Clinical Immunology (2020)