Abstract
Despite remarkable progress in survival with the availability of novel agents, an overwhelming majority of patients with multiple myeloma (MM) relapse and the curability of MM remains limited. Genetically defined high-risk MM represents a subgroup with an aggressive disease course despite novel agents. Allogeneic hematopoietic cell transplantation (allo-SCT) is a potentially curative option in MM that has several advantages including a tumor-free graft, and the potential for sustained immune-mediated disease control. However, historically high treatment-related mortality (TRM) and conflicting reports from prospective studies in the United States and European Union have limited the utilization of this modality. Meanwhile, newer preparative regimens, planned maintenance strategies and improvements in supportive care have led to a decline in TRM and better survival in recent years. The allo-SCT platform also provides additional options of immunotherapy at relapse including donor lymphocyte infusions, immunomodulatory drug maintenance and withdrawal of immune suppression. In this article, we provide an in-depth review of literature for allo-SCT and other immunotherapy options, as well as the authors’ approach to using allo-SCT in MM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Kyle RA, Rajkumar SV . Multiple myeloma. N Engl J Med 2004; 351: 1860–1873.
Jakubowiak AJ, Dytfeld D, Griffith KA, Lebovic D, Vesole DH, Jagannath S et al. A phase 1/2 study of carfilzomib in combination with lenalidomide and low-dose dexamethasone as a frontline treatment for multiple myeloma. Blood 2012; 120: 1801–1809.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med 2005; 352: 2487–2498.
Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010; 11: 29–37.
Wang M, Martin T, Bensinger W, Alsina M, Siegel DS, Kavalerchik E et al. Phase 2 dose-expansion study (PX-171-006) of carfilzomib, lenalidomide, and low-dose dexamethasone in relapsed or progressive multiple myeloma. Blood 2013; 122: 3122–3128.
Lonial S, Dimopoulos M, Palumbo A, White D, Grosicki S, Spicka I et al. Elotuzumab therapy for relapsed or refractory multiple myeloma. N Engl J Med 2015; 373: 621–631.
Masters GA, Krilov L, Bailey HH, Brose MS, Burstein H, Diller LR et al. Clinical cancer advances 2015: Annual report on progress against cancer from the American Society of Clinical Oncology. J Clin Oncol 2015; 33: 786–809.
Libura J, Hoffmann T, Passweg J, Gregor M, Favre G, Tichelli A et al. Graft-versus-myeloma after withdrawal of immunosuppression following allogeneic peripheral stem cell transplantation. Bone Marrow Transplant 1999; 24: 925–927.
Lokhorst H, Einsele H, Vesole D, Bruno B, San Miguel J, Perez-Simon JA et al. International Myeloma Working Group consensus statement regarding the current status of allogeneic stem-cell transplantation for multiple myeloma. J Clin Oncol 2010; 28: 4521–4530.
Barlogie B, Shaughnessy J, Tricot G, Jacobson J, Zangari M, Anaissie E et al. Treatment of multiple myeloma. Blood 2004; 103: 20–32.
Hunter HM, Peggs K, Powles R, Rahemtulla A, Mahendra P, Cavenagh J et al. Analysis of outcome following allogeneic haemopoietic stem cell transplantation for myeloma using myeloablative conditioning—evidence for a superior outcome using melphalan combined with total body irradiation. Br J Haematol 2005; 128: 496–502.
Bensinger WI, Buckner CD, Anasetti C, Clift R, Storb R, Barnett T et al. Allogeneic marrow transplantation for multiple myeloma: an analysis of risk factors on outcome. Blood 1996; 88: 2787–2793.
Gahrton G, Tura S, Ljungman P, Blade J, Brandt L, Cavo M et al. Prognostic factors in allogeneic bone marrow transplantation for multiple myeloma. J Clin Oncol 1995; 13: 1312–1322.
Gahrton G, Tura S, Ljungman P, Belanger C, Brandt L, Cavo M et al. Allogeneic bone marrow transplantation in multiple myeloma. European Group for Bone Marrow Transplantation. N Engl J Med 1991; 325: 1267–1273.
Gahrton G, Svensson H, Cavo M, Apperly J, Bacigalupo A, Bjorkstrand B et al. Progress in allogenic bone marrow and peripheral blood stem cell transplantation for multiple myeloma: a comparison between transplants performed 1983–93 and 1994–8 at European Group for Blood and Marrow Transplantation centres. Br J Haematol 2001; 113: 209–216.
Durie BG, Gale JP, Klein JP et al. Allogeneic transplants for multiple myeloma: an IBMTR analysis. Proc Am Soc Clin Oncol 1995; 15: 405.
Bjorkstrand BB, Ljungman P, Svensson H, Hermans J, Alegre A, Apperley J et al. Allogeneic bone marrow transplantation versus autologous stem cell transplantation in multiple myeloma: a retrospective case-matched study from the European Group for Blood and Marrow Transplantation. Blood 1996; 88: 4711–4718.
Barlogie B, Kyle RA, Anderson KC, Greipp PR, Lazarus HM, Hurd DD et al. Standard chemotherapy compared with high-dose chemoradiotherapy for multiple myeloma: final results of phase III US Intergroup Trial S9321. J Clin Oncol 2006; 24: 929–936.
Lokhorst HM, Segeren CM, Verdonck LF, van der Holt B, Raymakers R, van Oers MH et al. Partially T-cell-depleted allogeneic stem-cell transplantation for first-line treatment of multiple myeloma: a prospective evaluation of patients treated in the phase III study HOVON 24 MM. J Clin Oncol 2003; 21: 1728–1733.
Kroger N, Schwerdtfeger R, Kiehl M, Sayer HG, Renges H, Zabelina T et al. Autologous stem cell transplantation followed by a dose-reduced allograft induces high complete remission rate in multiple myeloma. Blood 2002; 100: 755–760.
Giralt S, Aleman A, Anagnostopoulos A, Weber D, Khouri I, Anderlini P et al. Fludarabine/melphalan conditioning for allogeneic transplantation in patients with multiple myeloma. Bone Marrow Transplant 2002; 30: 367–373.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009; 15: 1628–1633.
Kumar S, Zhang MJ, Li P, Dispenzieri A, Milone GA, Lonial S et al. Trends in allogeneic stem cell transplantation for multiple myeloma: a CIBMTR analysis. Blood 2011; 118: 1979–1988.
Kroger N, Shimoni A, Schilling G, Schwerdtfeger R, Bornhauser M, Nagler A et al. Unrelated stem cell transplantation after reduced intensity conditioning for patients with multiple myeloma relapsing after autologous transplantation. Br J Haematol 2010; 148: 323–331.
Maloney DG, Molina AJ, Sahebi F, Stockerl-Goldstein KE, Sandmaier BM, Bensinger W et al. Allografting with nonmyeloablative conditioning following cytoreductive autografts for the treatment of patients with multiple myeloma. Blood 2003; 102: 3447–3454.
Rotta M, Storer BE, Sahebi F, Shizuru JA, Bruno B, Lange T et al. Long-term outcome of patients with multiple myeloma after autologous hematopoietic cell transplantation and nonmyeloablative allografting. Blood 2009; 113: 3383–3391.
Bruno B, Rotta M, Patriarca F, Mattei D, Allione B, Carnevale-Schianca F et al. Nonmyeloablative allografting for newly diagnosed multiple myeloma: the experience of the Gruppo Italiano Trapianti di Midollo. Blood 2009; 113: 3375–3382.
Lokhorst HM, van der Holt B, Cornelissen JJ, Kersten MJ, van Oers M, Raymakers R et al. Donor versus no-donor comparison of newly diagnosed myeloma patients included in the HOVON-50 multiple myeloma study. Blood 2012; 119: 6219–6225; quiz 6399.
Rosinol L, Perez-Simon JA, Sureda A, de la Rubia J, de Arriba F, Lahuerta JJ et al. A prospective PETHEMA study of tandem autologous transplantation versus autograft followed by reduced-intensity conditioning allogeneic transplantation in newly diagnosed multiple myeloma. Blood 2008; 112: 3591–3593.
Bruno B, Rotta M, Patriarca F, Mordini N, Allione B, Carnevale-Schianca F et al. A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med 2007; 356: 1110–1120.
Giaccone L, Storer B, Patriarca F, Rotta M, Sorasio R, Allione B et al. Long-term follow-up of a comparison of nonmyeloablative allografting with autografting for newly diagnosed myeloma. Blood 2011; 117: 6721–6727.
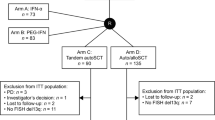
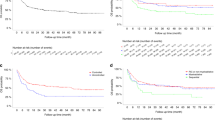
Krishnan A, Pasquini MC, Logan B, Stadtmauer EA, Vesole DH, Alyea E III et al. Autologous haemopoietic stem-cell transplantation followed by allogeneic or autologous haemopoietic stem-cell transplantation in patients with multiple myeloma (BMT CTN 0102): a phase 3 biological assignment trial. Lancet Oncol 2011; 12: 1195–1203.
Bjorkstrand B, Iacobelli S, Hegenbart U, Gruber A, Greinix H, Volin L et al. Tandem autologous/reduced-intensity conditioning allogeneic stem-cell transplantation versus autologous transplantation in myeloma: long-term follow-up. J Clin Oncol 2011; 29: 3016–3022.
Gahrton G, Iacobelli S, Bjorkstrand B, Hegenbart U, Gruber A, Greinix H et al. Autologous/reduced-intensity allogeneic stem cell transplantation vs autologous transplantation in multiple myeloma: long-term results of the EBMT-NMAM2000 study. Blood 2013; 121: 5055–5063.
Passera R, Pollichieni S, Brunello L, Patriarca F, Bonifazi F, Montefusco V et al. Allogeneic hematopoietic cell transplantation from unrelated donors in multiple myeloma: study from the Italian Bone Marrow Donor Registry. Biol Blood Marrow Transplant 2013; 19: 940–948.
Donato ML, Siegel DS, Vesole DH, McKiernan P, Nyirenda T, Pecora AL et al. The graft-versus-myeloma effect: chronic graft-versus-host disease but not acute graft-versus-host disease prolongs survival in patients with multiple myeloma receiving allogeneic transplantation. Biol Blood Marrow Transplant 2014; 20: 1211–1216.
Freytes CO, Vesole DH, LeRademacher J, Zhong X, Gale RP, Kyle RA et al. Second transplants for multiple myeloma relapsing after a previous autotransplant-reduced-intensity allogeneic vs autologous transplantation. Bone Marrow Transplant 2014; 49: 416–421.
Patriarca F, Einsele H, Spina F, Bruno B, Isola M, Nozzoli C et al. Allogeneic stem cell transplantation in multiple myeloma relapsed after autograft: a multicenter retrospective study based on donor availability. Biol Blood Marrow Transplant 2012; 18: 617–626.
de Lavallade H, El-Cheikh J, Faucher C, Furst S, Stoppa AM, Coso D et al. Reduced-intensity conditioning allogeneic SCT as salvage treatment for relapsed multiple myeloma. Bone Marrow Transplant 2008; 41: 953–960.
Michallet M, Sobh M, El-Cheikh J, Morisset S, Sirvent A, Reman O et al. Evolving strategies with immunomodulating drugs and tandem autologous/allogeneic hematopoietic stem cell transplantation in first line high risk multiple myeloma patients. Exp Hematol 2013; 41: 1008–1015.
Wirk B, Byrne M, Dai Y, Moreb JS . Outcomes of salvage autologous versus allogeneic hematopoietic cell transplantation for relapsed multiple myeloma after initial autologous hematopoietic cell transplantation. J Clin Med Res 2013; 5: 174–184.
Qazilbash MH, Saliba R, De Lima M, Hosing C, Couriel D, Aleman A et al. Second autologous or allogeneic transplantation after the failure of first autograft in patients with multiple myeloma. Cancer 2006; 106: 1084–1089.
Mehta J, Tricot G, Jagannath S, Ayers D, Singhal S, Siegel D et al. Salvage autologous or allogeneic transplantation for multiple myeloma refractory to or relapsing after a first-line autograft? Bone Marrow Transplant 1998; 21: 887–892.
Kroger N, Sayer HG, Schwerdtfeger R, Kiehl M, Nagler A, Renges H et al. Unrelated stem cell transplantation in multiple myeloma after a reduced-intensity conditioning with pretransplantation antithymocyte globulin is highly effective with low transplantation-related mortality. Blood 2002; 100: 3919–3924.
Weiden PL, Sullivan KM, Flournoy N, Storb R, Thomas ED . Antileukemic effect of chronic graft-versus-host disease: contribution to improved survival after allogeneic marrow transplantation. N Engl J Med 1981; 304: 1529–1533.
Ringden O, Shrestha S, da Silva GT, Zhang MJ, Dispenzieri A, Remberger M et al. Effect of acute and chronic GVHD on relapse and survival after reduced-intensity conditioning allogeneic transplantation for myeloma. Bone Marrow Transplant 2012; 47: 831–837.
Mir MA, Kapoor P, Kumar S, Pandey S, Dispenzieri A, Lacy MQ et al. Trends and outcomes in allogeneic hematopoietic stem cell transplant for multiple myeloma at mayo clinic. Clin Lymphoma Myeloma Leuk 2015; 15: 349–357 e2.
Garban F, Attal M, Michallet M, Hulin C, Bourhis JH, Yakoub-Agha I et al. Prospective comparison of autologous stem cell transplantation followed by dose-reduced allograft (IFM99-03 trial) with tandem autologous stem cell transplantation (IFM99-04 trial) in high-risk de novo multiple myeloma. Blood 2006; 107: 3474–3480.
Alyea E, Weller E, Schlossman R, Canning C, Webb I, Doss D et al. T-cell—depleted allogeneic bone marrow transplantation followed by donor lymphocyte infusion in patients with multiple myeloma: induction of graft-versus-myeloma effect. Blood 2001; 98: 934–939.
Stern M, de Wreede LC, Brand R, van Biezen A, Dreger P, Mohty M et al. Sensitivity of hematological malignancies to graft-versus-host effects: an EBMT megafile analysis. Leukemia 2014; 28: 2235–2240.
Smith E, Devlin SM, Kosuri S, Orlando E, Landau H, Lesokhin AM et al. CD34-selected allogeneic hematopoietic stem cell transplantation for patients with relapsed, high-risk multiple myeloma. Biol Blood Marrow Transplant 2015; pii: S1083-8791(15)00573-X (e-pub ahead of print).
Gorgun G, Samur MK, Cowens KB, Paula S, Bianchi G, Anderson JE et al. Lenalidomide enhances immune checkpoint blockade-induced immune response in multiple myeloma. Clin Cancer Res 2015; 21: 4607–4618.
DiCapua Siegel DS, Moreau P, Avigan D, Anderson KC, Reece DE, Migue JS et al. A phase 1 (Ph1) trial of MK-3475 combined with lenalidomide (Len) and low-dose dexamethasone (Dex) in patients (pts) with relapsed/refractory multiple myeloma (RRMM). J Clin Oncol 2014; 32: 5s. (suppl; abstract no. TPS3117).
Lokhorst HM, Plesner T, Laubach JP, Nahi H, Gimsing P, Hansson M et al. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med 2015; 373: 1207–1219.
Maus MV, June CH . Zoom Zoom: racing CARs for multiple myeloma. Clin Cancer Res 2013; 19: 1917–1919.
Mateos MV, Oriol A, Martinez-Lopez J, Gutierrez N, Teruel AI, de Paz R et al. Bortezomib, melphalan, and prednisone versus bortezomib, thalidomide, and prednisone as induction therapy followed by maintenance treatment with bortezomib and thalidomide versus bortezomib and prednisone in elderly patients with untreated multiple myeloma: a randomised trial. Lancet Oncol 2010; 11: 934–941.
Tricot G, Vesole DH, Jagannath S, Hilton J, Munshi N, Barlogie B . Graft-versus-myeloma effect: proof of principle. Blood 1996; 87: 1196–1198.
Kroger N, Kruger W, Renges H, Zabelina T, Stute N, Jung R et al. Donor lymphocyte infusion enhances remission status in patients with persistent disease after allografting for multiple myeloma. Br J Haematol 2001; 112: 421–423.
Lokhorst HM, Wu K, Verdonck LF, Laterveer LL, van de Donk NW, van Oers MH et al. The occurrence of graft-versus-host disease is the major predictive factor for response to donor lymphocyte infusions in multiple myeloma. Blood 2004; 103: 4362–4364.
Bellucci R, Alyea EP, Weller E, Chillemi A, Hochberg E, Wu CJ et al. Immunologic effects of prophylactic donor lymphocyte infusion after allogeneic marrow transplantation for multiple myeloma. Blood 2002; 99: 4610–4617.
de Carvalho F, Alves VL, Braga WM, Xavier CV Jr, Colleoni GW . MAGE-C1/CT7 and MAGE-C2/CT10 are frequently expressed in multiple myeloma and can be explored in combined immunotherapy for this malignancy. Cancer Immunol Immunother 2013; 62: 191–195.
Tyler EM, Jungbluth AA, O'Reilly RJ, Koehne G . WT1-specific T-cell responses in high-risk multiple myeloma patients undergoing allogeneic T cell-depleted hematopoietic stem cell transplantation and donor lymphocyte infusions. Blood 2013; 121: 308–317.
Kroger N, Badbaran A, Lioznov M, Schwarz S, Zeschke S, Hildebrand Y et al. Post-transplant immunotherapy with donor-lymphocyte infusion and novel agents to upgrade partial into complete and molecular remission in allografted patients with multiple myeloma. Exp Hematol 2009; 37: 791–798.
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1770–1781.
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1782–1791.
Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med 2014; 371: 895–905.
Wolschke C, Stubig T, Hegenbart U, Schonland S, Heinzelmann M, Hildebrandt Y et al. Postallograft lenalidomide induces strong NK cell-mediated antimyeloma activity and risk for T cell-mediated GvHD: Results from a phase I/II dose-finding study. Exp Hematol 2013; 41: 134–142 e3.
Luptakova K, Rosenblatt J, Glotzbecker B, Mills H, Stroopinsky D, Kufe T et al. Lenalidomide enhances anti-myeloma cellular immunity. Cancer Immunol Immunother 2013; 62: 39–49.
Rosenblatt J, Vasir B, Uhl L, Blotta S, Macnamara C, Somaiya P et al. Vaccination with dendritic cell/tumor fusion cells results in cellular and humoral antitumor immune responses in patients with multiple myeloma. Blood 2011; 117: 393–402.
Coman T, Bachy E, Michallet M, Socie G, Uzunov M, Bourhis JH et al. Lenalidomide as salvage treatment for multiple myeloma relapsing after allogeneic hematopoietic stem cell transplantation: a report from the French Society of Bone Marrow and Cellular Therapy. Haematologica 2013; 98: 776–783.
Kneppers E, van der Holt B, Kersten MJ, Zweegman S, Meijer E, Huls G et al. Lenalidomide maintenance after nonmyeloablative allogeneic stem cell transplantation in multiple myeloma is not feasible: results of the HOVON 76 Trial. Blood 2011; 118: 2413–2419.
Alsina M, Becker PS, Zhong X, Adams A, Hari P, Rowley S et al. Lenalidomide maintenance for high-risk multiple myeloma after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2014; 20: 1183–1189.
Kroger N, Zabelina T, Klyuchnikov E, Kropff M, Pfluger KH, Burchert A et al. Toxicity-reduced, myeloablative allograft followed by lenalidomide maintenance as salvage therapy for refractory/relapsed myeloma patients. Bone Marrow Transplant 2013; 48: 403–407.
Koreth J, Stevenson KE, Kim HT, McDonough SM, Bindra B, Armand P et al. Bortezomib-based graft-versus-host disease prophylaxis in HLA-mismatched unrelated donor transplantation. J Clin Oncol 2012; 30: 3202–3208.
Vodanovic-Jankovic S, Hari P, Jacobs P, Komorowski R, Drobyski WR . NF-kappaB as a target for the prevention of graft-versus-host disease: comparative efficacy of bortezomib and PS-1145. Blood 2006; 107: 827–834.
Kroger N, Zabelina T, Ayuk F, Atanackovic D, Schieder H, Renges H et al. Bortezomib after dose-reduced allogeneic stem cell transplantation for multiple myeloma to enhance or maintain remission status. Exp Hematol 2006; 34: 770–775.
Caballero-Velazquez T, Lopez-Corral L, Encinas C, Castilla-Llorente C, Martino R, Rosinol L et al. Phase II clinical trial for the evaluation of bortezomib within the reduced intensity conditioning regimen (RIC) and post-allogeneic transplantation for high-risk myeloma patients. Br J Haematol 2013; 162: 474–482.
Nishihori T, Ochoa-Bayona JL, Kim J, Pidala J, Shain K, Baz R et al. Allogeneic hematopoietic cell transplantation for consolidation of VGPR or CR for newly diagnosed multiple myeloma. Bone Marrow Transplant 2013; 48: 1179–1184.
Giebel S, Locatelli F, Lamparelli T, Velardi A, Davies S, Frumento G et al. Survival advantage with KIR ligand incompatibility in hematopoietic stem cell transplantation from unrelated donors. Blood 2003; 102: 814–819.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Benson DM Jr, Hofmeister CC, Padmanabhan S, Suvannasankha A, Jagannath S, Abonour R et al. A phase 1 trial of the anti-KIR antibody IPH2101 in patients with relapsed/refractory multiple myeloma. Blood 2012; 120: 4324–4333.
Hallett WH, Jing W, Drobyski WR, Johnson BD . Immunosuppressive effects of multiple myeloma are overcome by PD-L1 blockade. Biol Blood Marrow Transplant 2011; 17: 1133–1145.
Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood 2012; 119: 940–948.
Avet-Loiseau H, Daviet A, Brigaudeau C, Callet-Bauchu E, Terre C, Lafage-Pochitaloff M et al. Cytogenetic, interphase, and multicolor fluorescence in situ hybridization analyses in primary plasma cell leukemia: a study of 40 patients at diagnosis, on behalf of the Intergroupe Francophone du Myelome and the Groupe Francais de Cytogenetique Hematologique. Blood 2001; 97: 822–825.
Mikhael JR, Dingli D, Roy V, Reeder CB, Buadi FK, Hayman SR et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013. Mayo Clin Proc 2013; 88: 360–376.
Bahlis NJ . Darwinian evolution and tiding clones in multiple myeloma. Blood 2012; 120: 927–928.
Egan JB, Shi CX, Tembe W, Christoforides A, Kurdoglu A, Sinari S et al. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood 2012; 120: 1060–1066.
Chng WJ, Dispenzieri A, Chim CS, Fonseca R, Goldschmidt H, Lentzsch S et al. IMWG consensus on risk stratification in multiple myeloma. Leukemia 2014; 28: 269–277.
Moreau P, Cavo M, Sonneveld P, Rosinol L, Attal M, Pezzi A et al. Combination of international scoring system 3, high lactate dehydrogenase, and t(4;14) and/or del(17p) identifies patients with multiple myeloma (MM) treated with front-line autologous stem-cell transplantation at high risk of early MM progression-related death. J Clin Oncol 2014; 32: 2173–2180.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L et al. Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. J Clin Oncol 2015; 33: 2863–2869.
Barlogie B, Pineda-Roman M, van Rhee F, Haessler J, Anaissie E, Hollmig K et al. Thalidomide arm of Total Therapy 2 improves complete remission duration and survival in myeloma patients with metaphase cytogenetic abnormalities. Blood 2008; 112: 3115–3121.
Pineda-Roman M, Zangari M, Haessler J, Anaissie E, Tricot G, van Rhee F et al. Sustained complete remissions in multiple myeloma linked to bortezomib in total therapy 3: comparison with total therapy 2. Br J Haematol 2008; 140: 625–634.
Avet-Loiseau H . Ultra high-risk myeloma. Hematology Am Soc Hematol Educ Program 2010; 2010: 489–493.
Kroger N, Badbaran A, Zabelina T, Ayuk F, Wolschke C, Alchalby H et al. Impact of high-risk cytogenetics and achievement of molecular remission on long-term freedom from disease after autologous-allogeneic tandem transplantation in patients with multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 398–404.
Knop S, Liebisch P, Hebart H et al. Autologous followed by allogeneic versus tandem-autologous stem cell transplant in newly diagnosed FISH-del13q myeloma. ASH Annu Meet Abstr 2014; 124: 43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dhakal, B., Vesole, D. & Hari, P. Allogeneic stem cell transplantation for multiple myeloma: is there a future?. Bone Marrow Transplant 51, 492–500 (2016). https://doi.org/10.1038/bmt.2015.325
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.325
This article is cited by
-
Long-term outcomes of allogeneic stem cell transplant in multiple myeloma
Blood Cancer Journal (2023)
-
Quadruple gene-engineered natural killer cells enable multi-antigen targeting for durable antitumor activity against multiple myeloma
Nature Communications (2022)
-
Any closer to successful therapy of multiple myeloma? CAR-T cell is a good reason for optimism
Stem Cell Research & Therapy (2021)
-
Chimeric antigen receptor T cell therapy in multiple myeloma: promise and challenges
Bone Marrow Transplantation (2021)
-
Evaluation of EuroFlow minimal residual disease measurement and donor chimerism monitoring following tandem auto-allogeneic transplantation for multiple myeloma
Bone Marrow Transplantation (2021)