Abstract
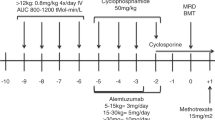
BU and CY (BU/CY; 200 mg/kg) before HLA-matched sibling allo-SCT in children with sickle cell disease (SCD) is associated with ~85% EFS but is limited by the acute and late effects of BU/CY myeloablative conditioning. Alternatives include reduced toxicity but more immunosuppressive conditioning. We investigated in a prospective single institutional study, the safety and efficacy of a reduced-toxicity conditioning (RTC) regimen of BU 12.8–16 mg/kg, fludarabine 180 mg/m2, alemtuzumab 54 mg/m2 (BFA) before HLA-matched sibling donor transplantation in pediatric recipients with symptomatic SCD. Eighteen patients, median age 8.9 years (2.3–20.2), M/F 15/3, 15 sibling BM and 3 sibling cord blood (CB) were transplanted. Mean whole blood and erythroid donor chimerism was 91% and 88%, at days +100 and +365, respectively. Probability of grade II–IV acute GVHD was 17%. Two-year EFS and OS were both 100%. Neurological, pulmonary and cardiovascular function were stable or improved at 2 years. BFA RTC and HLA-matched sibling BM and CB allo-SCT in pediatric recipients result in excellent EFS, long-term donor chimerism, low incidence of GVHD and stable/improved organ function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med 2004; 350: 886–895.
Kato GJ, McGowan V, Machado RF, Little JA, Jt Taylor, Morris CR et al. Lactate dehydrogenase as a biomarker of hemolysis-associated nitric oxide resistance, priapism, leg ulceration, pulmonary hypertension, and death in patients with sickle cell disease. Blood 2006; 107: 2279–2285.
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med 1994; 330: 1639–1644.
Rees DC, Williams TN, Gladwin MT . Sickle-cell disease. Lancet 2010; 376: 2018–2031.
Bernaudin F, Socie G, Kuentz M, Chevret S, Duval M, Bertrand Y et al. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease. Blood 2007; 110: 2749–2756.
Johnson FL, Look AT, Gockerman J, Ruggiero MR, Dalla-Pozza L, Billings FT 3rd . Bone-marrow transplantation in a patient with sickle-cell anemia. N Engl J Med 1984; 311: 780–783.
Vermylen C, Cornu G, Ferster A, Brichard B, Ninane J, Ferrant et al. Haematopoietic stem cell transplantation for sickle cell anaemia: the first 50 patients transplanted in Belgium. Bone Marrow Transplant 1998; 22: 1–6.
Walters MC, Patience M, Leisenring W, Eckman JR, Scott JP, Mentzer WC et al. Bone marrow transplantation for sickle cell disease. N Engl J Med 1996; 335: 369–376.
Locatelli F, Kabbara N, Ruggeri A, Ghavamzadeh A, Roberts I, Li CK et al. Outcome of patients with hemoglobinopathies given either cord blood or bone marrow transplantation from an HLA-identical sibling. Blood 2013; 122: 1072–1078.
Bhatia M, Walters MC . Hematopoietic cell transplantation for thalassemia and sickle cell disease: past, present and future. Bone Marrow Transplant 2008; 41: 109–117.
Walters MC, Hardy K, Edwards S, Adamkiewicz T, Barkovich J, Bernaudin F et al. Pulmonary, gonadal, and central nervous system status after bone marrow transplantation for sickle cell disease. Biol Blood Marrow Transplant 2010; 16: 263–272.
Walters MC, Patience M, Leisenring W, Eckman JR, Buchanan GR, Rogers ZR et al. Barriers to bone marrow transplantation for sickle cell anemia. Biol Blood Marrow Transplant 1996; 2: 100–104.
Satwani P, Harrison L, Morris E, Del Toro G, Cairo MS . Reduced-intensity allogeneic stem cell transplantation in adults and children with malignant and nonmalignant diseases: end of the beginning and future challenges. Biol Blood Marrow Transplant 2005; 11: 403–422.
Satwani P, Morris E, BradLey MB, Bhatia M, van de Ven C, Cairo MS . Reduced intensity and non-myeloablative allogeneic stem cell transplantation in children and adolescents with malignant and non-malignant diseases. Pediatr Blood Cancer 2008; 50: 1–8.
Styczynski J, Tallamy B, Waxman I, van de Ven C, Milone MC, Shaw LM et al. A pilot study of reduced toxicity conditioning with BU, fludarabine and alemtuzumab before the allogeneic hematopoietic SCT in children and adolescents. Bone Marrow Transplant 2011; 46: 790–799.
Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med 2009; 361: 2309–2317.
Geyer MB, Jacobson JS, Freedman J, George D, Moore V, van de Ven C et al. A comparison of immune reconstitution and graft-versus-host disease following myeloablative conditioning versus reduced toxicity conditioning and umbilical cord blood transplantation in paediatric recipients. Br J Haematol 2011; 155: 218–234.
Le Gall JB, Milone MC, Waxman IM, Shaw LM, Harrison L, Duffy D et al. The pharmacokinetics and safety of twice daily i.v. BU during conditioning in pediatric allo-SCT recipients. Bone Marrow Transplant 2013; 48: 19–25.
Osunkwo I, Bessmertny O, Harrison L, Cheung YK, Van de Ven C, del Toro G et al. A pilot study of tacrolimus and mycophenolate mofetil graft-versus-host disease prophylaxis in childhood and adolescent allogeneic stem cell transplant recipients. Biol Blood Marrow Transplant 2004; 10: 246–258.
Bhatia M, Militano O, Jin Z, Figurski M, Shaw L, Moore V et al. An age-dependent pharmacokinetic study of intravenous and oral mycophenolate mofetil in combination with tacrolimus for GVHD prophylaxis in pediatric allogeneic stem cell transplantation recipients. Biol Blood Marrow Transplant 2010; 16: 333–343.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 1974; 18: 295–304.
Waxman IM, Militano O, Baldinger L, Roman E, Qualter E, Morris E et al. Sequential administration of sargramostim and filgrastim in pediatric allogeneic stem cell transplantation recipients undergoing myeloablative conditioning. Pediatr Transplant 2009; 13: 464–474.
Roman E, Osunkwo I, Militano O, Cooney E, van de Ven C, Cairo MS . Liposomal amphotericin B prophylaxis of invasive mold infections in children post allogeneic stem cell transplantation. Pediatr Blood Cancer 2008; 50: 325–330.
Shereck EB, Cooney E, van de Ven C, Della-Lotta P, Cairo MS . A pilot phase II study of alternate day ganciclovir and foscarnet in preventing cytomegalovirus (CMV) infections in at-risk pediatric and adolescent allogeneic stem cell transplant recipients. Pediatr Blood Cancer 2007; 49: 306–312.
Horn B, Soni S, Khan S, Petrovic A, Breslin N, Cowan M et al. Feasibility study of preemptive withdrawal of immunosuppression based on chimerism testing in children undergoing myeloablative allogeneic transplantation for hematologic malignancies. Bone Marrow Transplant 2009; 43: 469–476.
Satwani P, Baldinger L, Freedman J, Jacobson JS, Guerra J, van de Ven C et al. Incidence of Viral and fungal infections following busulfan-based reduced-intensity versus myeloablative conditioning in pediatric allogeneic stem cell transplantation recipients. Biol Blood Marrow Transplant 2009; 15: 1587–1595.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS et al. Risk factors for acute GVHDand survival after hematopoietic cell transplantation. Blood 2012; 119: 296–307.
Sung AD, Chao NJ . Concise review: acute graft-versus-host disease: immunobiology, prevention, and treatment. Stem Cells Transl Med 2013; 2: 25–32.
Krishnamurti L, Kharbanda S, Biernacki MA, Zhang W, Baker KS, Wagner JE et al. Stable long-term donor engraftment following reduced-intensity hematopoietic cell transplantation for sickle cell disease. Biol Blood Marrow Transplant 2008; 14: 1270–1278.
Panepinto JA, Walters MC, Carreras J, Marsh J, Bredeson CN, Gale RP et al. Matched-related donor transplantation for sickle cell disease: report from the Center for International Blood and Transplant Research. Br J Haematol 2007; 137: 479–485.
Satwani P, Jin Z, Duffy D, Morris E, Bhatia M, Garvin JH et al. Transplantation-related mortality, graft failure, and survival after reduced-toxicity conditioning and allogeneic hematopoietic stem cell transplantation in 100 consecutive pediatric recipients. Biol Blood Marrow Transplant 2013; 19: 552–561.
Walters MC, Patience M, Leisenring W, Rogers ZR, Aquino VM, Buchanan GR et al. Stable mixed hematopoietic chimerism after bone marrow transplantation for sickle cell anemia. Biol Blood Marrow Transplant 2001; 7: 665–673.
Scothorn DJ, Price C, Schwartz D, Terrill C, Buchanan GR, Shurney W et al. Risk of recurrent stroke in children with sickle cell disease receiving blood transfusion therapy for at least five years after initial stroke. J Pediatr 2002; 140: 348–354.
Noe A, Cappelli B, Biffi A, Chiesa R, Frugnoli I, Biral E et al. High incidence of severe cyclosporine neurotoxicity in children affected by haemoglobinopaties undergoing myeloablative haematopoietic stem cell transplantation: early diagnosis and prompt intervention ameliorates neurological outcome. Ital J Pediatr 2010; 36: 14.
Wong R, Beguelin GZ, de Lima M, Giralt SA, Hosing C, Ippoliti C et al. Tacrolimus-associated posterior reversible encephalopathy syndrome after allogeneic haematopoietic stem cell transplantation. Br J Haematol 2003; 122: 128–134.
Freed J, Talano J, Small T, Ricci A, Cairo MS . Allogeneic cellular and autologous stem cell therapy for sickle cell disease: 'whom, when and how'. Bone Marrow Transplant 2012; 47: 1489–1498.
Sheth S, Licursi M, Bhatia M . Sickle cell disease: time for a closer look at treatment options? Br J Haematol 2013; 162: 455–464.
Acknowledgements
The authors would like to thank all the families who participated in this clinical trial and all the faculty and staff on the Pediatric Blood and Marrow Transplant unit at Columbia University. This research was supported in part by grants from the Pediatric Cancer Research Foundation (MSC), Doris Duke Charitable Foundation (MG and KR) and Food and Drug Administration (5R01FD004090-02) (MSC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bhatia, M., Jin, Z., Baker, C. et al. Reduced toxicity, myeloablative conditioning with BU, fludarabine, alemtuzumab and SCT from sibling donors in children with sickle cell disease. Bone Marrow Transplant 49, 913–920 (2014). https://doi.org/10.1038/bmt.2014.84
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.84
This article is cited by
-
Significant improvement of child physical and emotional functioning after familial haploidentical stem cell transplant
Bone Marrow Transplantation (2022)
-
Matched related hematopoietic cell transplant for sickle cell disease with alemtuzumab: the Texas Children’s Hospital experience
Bone Marrow Transplantation (2021)
-
Hematopoietic stem cell transplantation reverses white matter injury measured by diffusion-tensor imaging (DTI) in sickle cell disease patients
Bone Marrow Transplantation (2021)
-
Stable to improved cardiac and pulmonary function in children with high-risk sickle cell disease following haploidentical stem cell transplantation
Bone Marrow Transplantation (2021)