Abstract
While nonmyeloablative peripheral blood stem cell transplantation (NST) has shown efficacy against several solid tumors, it is untested in nasopharyngeal cancer (NPC). In a phase II clinical trial, 21 patients with pretreated metastatic NPC underwent NST with sibling PBSC allografts, using CY conditioning, thymic irradiation and in vivo T-cell depletion with thymoglobulin. Stable lymphohematopoietic chimerism was achieved in most patients and prophylactic CYA was tapered at a median of day +30. Seven patients (33%) showed partial response and three (14%) achieved stable disease. Four patients were alive at 2 years and three showed prolonged disease control of 344, 525 and 550 days. With a median follow-up of 209 (4–1147) days, the median PFS was 100 days (95% confidence interval (CI), 66–128 days), and median OS was 209 days (95% CI, 128–236 days). Patients with chronic GVHD had better survival—median OS 426 days (95% CI, 194–NE days) vs 143 days (95% CI, 114–226 days) (P=0.010). Thus, NST may induce meaningful clinical responses in patients with advanced NPC.
Similar content being viewed by others
Introduction
Nasopharyngeal carcinoma (NPC) is endemic in southern China and Southeast Asia and long-term survival for patients with advanced NPC remains poor, despite the use of salvage chemotherapy agents.1, 2, 3 Molecular targeted therapies have not yet achieved significant benefit against NPC. Thus, novel approaches are urgently needed. Because NPC in Asia is almost universally associated with EBV, and viral oncoproteins (EBNA1, LMP1 and LMP2) are expressed by tumor cells, immunotherapy represents a promising therapeutic strategy.4, 5, 6 Studies using adoptively transferred EBV-specific cytotoxic T cells (CTLs) in NPC have shown clinical responses in patients;7, 8, 9 however, their overall efficacy is modest, especially in patients with metastatic and/or bulky disease.
Nonmyeloablative peripheral blood stem cell transplantation (NST) may present another immunotherapeutic approach for patients with advanced stage NPC. Through a potent graft-vs-tumor (GVT) effect,10 NST has shown some efficacy against a range of solid tumors including renal cell, breast and colon cancers.11, 12, 13, 14, 15, 16, 17 Its role in NPC, however, has not yet been evaluated.
To evaluate the role of NST in patients with pretreated metastatic NPC, we conducted a prospective phase II study. We used an NST regimen modified from Spitzer et al.,18 using the comparably more lymphodepleting rabbit antithymocyte globulin, thymoglobulin, aiming to induce stable mixed chimerism, before final conversion to a full donor lymphohematopoietic chimera. Single agent CYA was tapered rapidly in our protocol and donor lymphocyte infusions were used as needed.
Although patients in our study were heavily pretreated, we achieved a reasonable response rate with NST, and several patients had durable disease control.
Patients and methods
Patients
Patients <70 years and Eastern Cooperative Oncology Group performance status (PS) of ⩽2, metastatic NPC who had received at least one line of salvage chemotherapy were eligible. Patients with a left ventricular ejection fraction of <45%, active angina pectoris, uncontrolled arrhythmia, hypertension, severe chronic or restrictive lung disease, or corrected diffusing capacity for carbon monoxide of ⩽50%, creatinine clearance of <50 mL/min, serum bilirubin of >2 mg/100 mL or ALT or AST >3 × the upper limit of normal were excluded, as were patients with active uncontrolled infection, active central nervous system disease, human immunodeficiency virus and hepatitis B or C positive serology. Written informed consent was obtained from all patients. This study was approved by the institutional ethics committee of the National Cancer Centre of Singapore.
Procedures
In dedicated HEPA-filtered BMT rooms, patients received a conditioning regimen of i.v. CY 50 mg/kg/day from day −5 to −3, a single fraction of 7 Gy thymic irradiation (unless there had been previous mediastinal radiation) on day −1, in vivo T-cell depletion with rabbit antithymocyte globulin (thymoglobulin; Genzyme, Cambridge, MA, USA), at 2.5 mg/kg/day initially on day −1, +1, +3 and +5 (regimen 1). This schedule was later modified to day −1, +1, +2 and +3 (regimen 2) because of secondary graft loss in patients receiving regimen 1.
Hematopoietic SCT
Patients received unmanipulated allogeneic PBSC grafts from their HLA-identical or single Ag-mismatch sibling donor. Donor PBMC were collected by leukapheresis and donor leukocyte infusion (DLIs) were considered at least 14 days after complete prophylactic CYA taper provided there was no acute GVHD and/or if the donor T-cell chimerism was not increasing. After the first DLI, at a dose of 1 × 107 per kg CD3+ T cells, subsequent DLI was considered monthly at incrementally increasing doses. Donor chimerism was analyzed weekly using semiquantitative PCR analysis, until full donor chimerism (>95% of donor cells in the mononuclear cell population) was achieved.
GVHD prophylaxis
All patients received GVHD prophylaxis of CYA (Neoral; Novartis, Singapore) starting at 5 mg/kg/day i.v. divided into two doses from day −1 that was reduced to 3 mg/kg/day from day+4. Once engrafted, patients were converted to daily oral CYA 12 mg/kg, aiming for a therapeutic trough level between 200 and 400 ng/mL. In the absence of acute GVHD, CYA was rapidly tapered.
Supportive care
Prophylactic ciprofloxacin, fluconazole, acyclovir and cotrimoxazole were administered as described previously.18 For acute GVHD of ⩾grade II, methylprednisolone of 2 mg/kg/day was initiated. CMV infection was screened using viral pp65 antigenemia assay weekly after hospital discharge until day +100. Pre-emptive i.v. ganciclovir was administered according to institutional practice.
Treatment-related toxicities and GVHD
Toxicities were graded according to National Cancer Institute Common Toxicity Criteria (version 3.0) and the severity of acute GVHD according to the International Bone Marrow Transplant Registry criteria and post-DLI acute and chronic GVHD by the common criteria.19
Immunophenotyping T-cell subpopulations
Peripheral blood was collected from 20 evaluable NPC patients pre-NST and serially up to 1-year post-NST, and from 20 healthy volunteers to serve as normal controls. Immunophenotyping of human T lymphocytes was performed by multicolor flow cytometric analysis by FACSCalibur (Becton Dickinson, San Jose, CA, USA) to determine the levels of specific functional T-cell subsets, such as naive, memory/effector T cells and regulatory T (Treg) cells.20
Monitoring cell-free EBV DNA in plasma
DNA was extracted from plasma samples collected at monthly intervals. Real-time PCR with EBV-specific probe and primer sets targeted at the Epstein-Barr Nuclear Antigen region was performed as previously described.21
Statistical analysis
The interval of PFS was calculated from the date of transplantation to the first documentation of disease progression or death from any cause, or last follow-up; and OS duration from the date of transplantation to the first documentation of death from any cause, or last follow-up. Duration of response was measured from date of first objective RECIST response to date of disease progression or death, whichever earlier. Time to response was measured from the date of transplantation to the first documentation of response.
Pearson χ2-test or Fisher's exact test was used to test the association between categorical variables, whereas Mann–Whitney U-test was used to test the difference of continuous variables. Best overall tumor response rate was summarized with 95% confidence interval using the Wilson method.22 Survival and response curves were estimated by the Kaplan–Meier method and comparisons between curves were tested by log-rank test.
Results
Patient characteristics
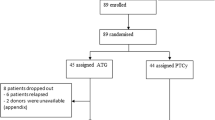
Between July 2002 and July 2007, 59 advanced NPC patients and their siblings were screened and HLA-typed. Twenty-six patients with histologically confirmed metastatic NPC and available HLA-matched sibling donor allografts (n=24) or an HLA one-Ag mismatched donor allograft (n=2) were accrued. Only 21 patients eventually received NST due to rapid progressive disease in 5 patients. In 2003, the severe acute respiratory syndrome epidemic halted accrual of patients for almost a year.
Median age (n=21) was 48 (34–57) years, and patients had received a median of two previous chemotherapy regimens (1–8) with a median of four (2–8) chemotherapy agents. All patients had extensive metastases, with a median of four (2–5) organ sites and 17 had previous progressive disease (Table 1). Seventeen patients (81%) had performance status (PS) of 0–1 and four (19%) had a PS of 2.
Transplant and engraftment
The median hospitalization for NST was 25 (12–90) days and the median PBSC dose infused was 5.25 × 106 (2.42–10.18 × 106) CD34+ PBSC per kg. Median time to engraftment was 12 (9–20) days. Three patients (15%) developed mild engraftment syndrome (⩽grade II). Four patients (20%) had secondary engraftment loss, under regimen 1, whereas no patient under regimen 2 experienced graft loss (P=0.087). One patient on regimen 1 was given i.v. CY before third DLI to augment donor chimerism.
Patients with mixed chimerism who did not have acute GVHD underwent rapid CYA taper. The median time to complete removal of CsA for 19 evaluated patients was on day +30 (day +16 to +42). CYA was subsequently restarted for the treatment of either acute or chronic GVHD in 10 patients, with patients receiving concurrent corticosteroids.
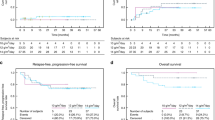
The median level of donor chimerism among patients who had achieved stable mixed chimerism was 50% at day +100 and 95% at 6 months post-NST. Sixteen patients received DLIs. The median number of DLIs administered per patient was 2 (1–6), and the mean dose at each administration per patient was 1.53±0.43 × 107 CD3+ T cells per kg. Immune reconstitution of CD3+, CD4+ and CD8+ T-cell populations post-NST is outlined in Supplementary Figure 1A and Treg cell data are provided in Supplementary Figure 1B. Patients on study had higher baseline Treg cells (9.41%) compared to normal controls (P=0.009) though there was no difference in pre-NST CD4+ Treg numbers between responders and nonresponders.
Transplant mortality and adverse events
Two patients died within 100 days of transplant, one of acute GVHD on day +91 (patient 5), and one of acute pulmonary embolism on day +4 (patient 21). Bacterial infections (grades III, IV and V) constituted the commonest complication, occurring in seven patients (Table 2). In most instances, sepsis occurred within 100 days of NST, and was effectively treated with i.v. antibiotics. One patient died from a strongyloides infection on day +137 post-NST. One patient developed CMV retinitis and was successfully treated with ganciclovir.
Grade II–IV acute GVHD occurred in five patients (25%), and was controllable with standard immunosuppressive agents in all except in one patient who died on day +91, following a second DLI. Chronic GVHD (all limited) was diagnosed in six patients (30%), and only one patient required prolonged CYA treatment.
Clinical response
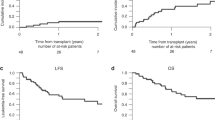
Seven patients (33%) achieved partial responses (PR) and three (14%) achieved stable disease, yielding an overall response rate of 47% (Supplementary Figure 2). The median time to PR was 57 (26–662) days and the median duration of PR was 77 (36–396) days. Late responses (>day +100) were observed in three patients (patients 7, 16 and 19) coincident with rising donor chimerism. Patients with GVHD had a much higher likelihood of response than patients without GVHD (P=0.004, Figure 1a). Serial evaluation of EBV DNA levels were performed in 11 patients and showed a strong correlation to the observed clinical responses (Supplementary Table 1).
(a) Kaplan–Meier estimate of cumulative probability of a response (that is, partial response, PR) in all patients and in patients with or without GVHD. Patients in whom GVHD developed after NST had significantly higher probability of response. (b) Kaplan–Meier estimated PFS. (c) Kaplan–Meier estimated OS according to chronic GVHD status.
PFS and OS
At the time of analysis, only one patient was alive. With a median follow-up of 209 (4–1147) days, the estimated median PFS was 100 (95% CI, 66–128) days (Figure 1b) and the 1-year PFS rate was 5% (s.e., 0.047). Two patients showed prolonged disease control of 344 and 525 days and a third had a second PFS of 550 days.
Patient 7, a lady with progressive lung, nodal, and bone metastases pre-NST achieved brief tumor shrinkage post-NST but progressed on day +118. Following limited chronic GVHD on day +202, she achieved stable disease for approximately 3 months before progressing again. Five DLIs were then administered (Supplementary Figure 2). Although her disease continued to regress on CT scans, objective PR did not occur until much later on day +662. Her response duration was 211 days and the duration of her second PFS was 550 days.
Patient 16 experienced the longest response duration (396 days), even though he had entered the study with an extremely aggressive disease and evidence of impending BM failure. Pre-NST, he was symptomatic with worsening dyspnea and intense bone pain despite NSAID and opioid analgesia. He achieved tumor shrinkage of 34% on day +129 when donor chimerism increased from 25 to 87% that correlated with a decreasing EBV DNA titer (Figure 2). Upon onset of limited chronic GVHD, his tumor continued to shrink further, and regressed once again when donor chimerism reached 100% (Figure 2b). One year after NST, he achieved PR and complete resolution of all symptoms with significant improvement in quality of life, and his BM biopsy, that had still been positive at day+100, finally showed no detectable NPC.
(a) CT scan images for patient 16. The tumor masses (indicated by arrowheads) show reduction in sizes that correlates with a corresponding increase in donor chimerism. On day +336, patient 16 continues to show tumor response. (b) Donor lymphohematopoietic chimerism levels and tumor diameter. (c) Serial plasma cell-free EBV DNA titer in patient 16.
Patient 19 achieved a chimerism of 60% 6 weeks post-NST but this decreased to 12% by day +111. He attained a late PR on day +101 with a more than 75% reduction in tumor diameter. Chimerism improved from 12 to 62.5%, 18 days after the PR that was related to mild GHVD.
The median OS for patients who underwent NST was 209 (95% CI, 128–236) days, the 1-year OS rate was 29% (s.e., 0.099) and the 2-year OS rate was 19% (s.e., 0.088). Patients with chronic GVHD also had much better survival—median OS was 426 days (95% CI, 194–NE days) vs 143 days (95%CI, 114–226 days) in patients without chronic GVHD (P=0.010, Figure 2c). Patients who responded to treatment (PR or stable disease) also had a trend toward better survival than nonresponders; median survival time of 326 (95% CI, 136–782) days against 195 (95% CI, 100–235) days, respectively (univariate P=0.055). Responders and nonresponders were similar in age, number of disease sites and previous chemotherapy, although pre-NST performance status was poorer in responders.
Discussion
We report results of the first study exploring NST in advanced NPC. Our results show that NST is feasible, and may induce durable responses in subsets of patients, even in the presence of extensive, bulky disease. In our study, we achieved a response rate of 33% and a clinical benefit of 47%, which compares well with the response rates achieved in second- and third-line chemotherapy against NPC (approximately 11–23%).1, 2, 3
Our NST regimen was overall well tolerated. The integration of thymoglobulin into the same ATG schedule as the Spitzer regimen18 (regimen 1) resulted in a high incidence of secondary engraftment loss in 4 out of 10 patients. After we revised to incorporate thymoglobulin earlier into the conditioning timeline (regimen 2), which may have worked better to deplete host than donor T lymphocytes, all 10 evaluable patients achieved stable and full donor lymphohematopoietic chimerism. In our study, engraftment syndrome occurred only in 15% of patients and was mild, requiring no treatment, as compared to 67% in the Boston study18 in which some patients required high-dose steroids for control of this syndrome.
Although our median PFS was short, PFS may underestimate clinical benefit for several reasons. Patients may experience late responses, which occur only after an initial disease progression—however, because only the first event (progressive disease) is used to construct the Kaplan–Meier graph, it would give the false impression of a lack of benefit. Late responses have been described in earlier NST studies and occur typically 3–6 months post transplant,23, 24 after conversion to a full donor chimerism, although it may be influenced by factors such as the early withdrawal of immunosuppressants or the use of DLIs.12 Second, patients on NST may experience more than one response. For example, patient 7 had 2 periods of responses—whereas her first PFS was 127 days, the second PFS was significantly longer at 550 days. Finally, NST through reconstituting the immune system may change the biological and growth characteristics of the disease, and thus OS (which is not reliant on any single time point cutoff) may be a more accurate measure of true benefit.
The median OS in our NST study was 7.4 months, with 1- and 2-year OS rate of 29 and 19%, respectively, which is comparable to the median 7–14 months OS for metastatic NPC patients in literature.1, 2, 3 More importantly, our subgroup analysis indicates that chronic GVHD significantly predicted for both response and OS. This raises questions regarding the role of mHA in mediating the GVT effect, which could be exploited further as an antitumor strategy.14, 25, 26
Despite early prophylactic CYA taper, GVHD incidence in our study was acceptable, largely due to the high percentage of patients who achieved mixed chimerism by day +100. Still, infections were more commonly observed in our study as compared with other NST studies.11, 12, 13 This may be related to xerostomia, poor dentition, chronic sinusitis and altered mucosal barriers in our NPC patients, most of whom had previous radiotherapy for primary disease. Future NST studies should consider such local immunosuppressive features when selecting patients for NST.
In summary, our study shows that our thymoglobulin-based NST can induce durable responses in NPC patients and overall allow for early taper of prophylactic CYA with acceptable GVHD rates and evidence of GVT. However regimen-related toxicities require careful patient selection. In the study of NST in Hodgkin's disease, an EBV-related tumor, better outcomes were achieved in patients with induced remission before NST.27 It is therefore likely that better outcomes may have been achievable if NST were to be performed in metastatic NPC patients who show response to induction chemotherapy.
References
Poon D, Chowbay B, Cheung YB, Leong SS, Tan EH . Phase II study of irinotecan (CPT-11) as salvage therapy for advanced nasopharyngeal carcinoma. Cancer 2005; 103: 576–581.
Chan TC, Hsu MM, Goh BC, Hui EP, Liu TW, Millward MJ et al. Multicenter, phase II study of cetuximab in combination with carboplatin in patients with recurrent or metastatic nasopharyngeal carcinoma. J Clin Oncol 2005; 23: 3568–3576.
Chua TT, Sham ST, Au KH . A phase II study of capecitabine in patients with recurrent and metastatic nasopharyngeal carcinoma pretreated with platinum-based chemotherapy. Oral Oncol 2003; 39: 361–366.
Zur Hausen H, Schulte-Holthausen H, Klein G, Henle W, Henle G, Clifford P et al. EBV DNA in biopsies of Burkitt tumours and anaplastic carcinomas of the nasopharynx. Nature 1970; 228: 11056–11058.
Klein G, Giovanella B, Lindahl T, Fialkow PJ, Singh S, Stehlin JS . Direct evidence for the presence of Epstein-Barr virus DNA and nuclear antigen in malignant epithelial cells from patients with poorly differentiated carcinoma of the nasopharynx. Proc Natl Acad Sci USA 1974; 71: 4737–4741.
Cohen JI . Epstein-Barr virus infection. N Engl J Med 2000; 343: 481–492.
Comoli P, Pedrazzoli P, Maccario R, Basso S, Carminati O, Labirio M et al. Cell therapy of stage IV nasopharyngeal carcinoma with autologous Epstein-Barr virus-targeted cytotoxic T lymphocytes. J Clin Oncol 2005; 23: 8942–8949.
Straathof KC, Bollard CM, Popat U, Huls MH, Lopez T, Morriss MC et al. Treatment of nasopharyngeal carcinoma with Epstein-Barr virus-specific T lymphocytes. Blood 2005; 105: 1898–1904.
Louis CU, Straathof K, Bollard CM, Gerken C, Huls MH, Gresik MV et al. Enhancing the in vivo expansion of adoptively transferred EBV-specific CTL with lymphodepleting CD45 monoclonal antibodies in NPC patients. Blood 2009; 113: 2442–2450.
Thomas ED, Blume KG . Historical markers in the development of allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 1999; 5: 341–346.
Childs R, Chernoff A, Contentin N, Bahceci E, Schrump D, Leitman S et al. Regression of metastatic renal cell carcinoma after nonmyeloablative allogeneic peripheral-blood stem-cell transplantation. N Engl J Med 2000; 343: 750–758.
Artz AS, Van Besian K, Zimmerman T, Gajewski TF, Rini BI, Hu HS et al. Long-term follow up of nonmyeloablative allogeneic stem-cell transplantation for renal cell carcinoma. The University of Chicago Experience. Bone Marrow Transplant 2005; 35: 253–260.
Carella AM, Beltrami G, Corsetti MT, Nati S, Musto P, Scalzulli P et al. Reduced intensity conditioning for allograft after cytoreductive autograft in metastatic breast cancer. Lancet 2005; 366: 318–320.
Eibl B, Schwaighofer H, Nachbaur D, Marth C, Gachter A, Knapp R et al. Evidence for graft-versus-tumor effect in a patient treated with marrow ablative chemotherapy and allogenic bone marrow transplantation for breast cancer. Blood 1996; 88: 1501–1508.
Ueno NT, Rondon G, Mirza NQ, Geisler DK, Anderlini P, Giralt SA et al. Allogeneic peripheral-blood progenitor-cell transplantation for poor-risk patients with metastatic breast cancer. J Clin Oncol 1998; 16: 986–993.
Bregni M, Dodero A, Peccatori J, Pescarollo A, Bernardi M, Sassi I et al. Nonmyeloablative conditioning followed by hematopoietic cell allografting and donor lymphocyte infusions for patients with metastatic renal and breast cancer. Blood 2002; 99: 4234–4236.
Busca A, Novarino A, de Fabritiis P, Picardi A, Zeuli M, Locatelli F et al. Nonmyeloablative allogeneic blood stem cell transplantation in patients with metastatic solid tumors. Hematology 2006; 11: 171–177.
Spitzer TR, McAfee S, Sackstein R, Colby C, Toh HC, Multani P et al. Intentional induction of mixed chimerism and achievement of antitumor responses after nonmyeloablative conditioning therapy and HLA-matched donor bone marrow transplantation for refractory hematologic malignancies. Biol Blood Marrow Transplant 2000; 6: 309–320.
Del Toro G, Satwani P, Harrison L, Cheung YK, Brigid Bradley M, George D et al. A pilot study of reduced intensity conditioning and allogeneic stem cell transplantation from unrelated cord blood and matched family donors in children and adolescent recipients. Bone Marrow Transplant 2004; 33: 613–622.
Baecher-Allan C, Wolf E, Hafler DA . Functional analysis of highly defined, FACS-isolated populations of human regulatory CD4+ CD25+ T cells. Clin Immunol 2005; 115: 10–18.
Lo YM, Chan AT, Chan LY, Leung SF, Lam CW, Huang DP et al. Molecular prognostication of nasopharyngeal carcinoma by quantitative analysis of circulating Epstein-Barr virus DNA. Cancer Res 2000; 60: 6878–6881.
Altman DG, Machin D, Bryant TN, Gardner S (eds). Statistics with Confidence, 2nd edn. BMJ Books: London, 2000.
Yang JC, Childs R . Immunotherapy for renal cell cancer. J Clin Oncol 2006; 24: 5576–5583.
Blaise D, Bay JO, Faucher C, Michallet M, Boiron JM, Choufi B et al. Reduced-intensity preparative regimen and allogeneic stem cell transplantation for advanced solid tumors. Blood 2004; 103: 435–441.
Spellman S, Warden MB, Haagenson M, Pietz BC, Goulmy E, Warren EH et al. Effects of mismatching for minor histocompatibility antigens on clinical outcomes in HLA-matched unrelated hematopoietic stem cell transplants. Biol Blood Marrow Transplant 2009; 15: 856–863.
Nishida T, Hudecek M, Kostic A, Bleakley M, Warren EH, Maloney D et al. Development of tumor-reactive T cells after nonmyeloablative allogeneic hematopoietic stem cell transplant for chronic lymphocytic leukemia. Clin Cancer Res 2009; 15: 4759–4768.
Peggs KS, Hunter A, Chopra R, Parker A, Mahendra P, Milligan D et al. Clinical evidence of a graft-versus-Hodgkin's-lymphoma effect after reduced-intensity allogeneic transplantation. Lancet 2005; 365: 1934–1941.
Acknowledgements
We acknowledge the kind assistance of Dr Stephen Gottschalk, who has helped in the review and editing of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Toh, H., Chia, W., Sun, L. et al. Graft-vs-tumor effect in patients with advanced nasopharyngeal cancer treated with nonmyeloablative allogeneic PBSC transplantation. Bone Marrow Transplant 46, 573–579 (2011). https://doi.org/10.1038/bmt.2010.161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2010.161
Keywords
This article is cited by
-
Reduced-intensity allografting in patients with therapy-related myeloid neoplasms and active primary malignancies
Bone Marrow Transplantation (2011)