Abstract
Background:
The relationship between hormone exposure and breast cancer risk in women treated with chest radiotherapy for childhood cancer is uncertain.
Methods:
Participants included 1108 females from the Childhood Cancer Survivor Study who were diagnosed with childhood cancer 1970–1986, treated with chest radiotherapy, and survived to ages ⩾20 years. Hazard ratios (HRs) and 95% confidence intervals (CIs) from Cox models adjusted for chest radiation field, delivered dose, anthracycline exposure, and age at childhood cancer estimated risk.
Results:
Among 195 women diagnosed with breast cancer, 102 tumours were oestrogen-receptor positive (ER+). Breast cancer risk increased with ⩾10 years of ovarian function after chest radiotherapy vs <10 years (HR=2.89, CI 1.56–5.53) and for radiotherapy given within 1 year of menarche vs >1 year from menarche (HR=1.80, CI 1.19–2.72). Risk decreased with decreasing age at menopause (Ptrend=0.014). Risk factors did not differ for ER+ breast cancer. Survivors with an age at menopause <20 years treated with hormone therapy had a lower breast cancer risk than premenopausal survivors (HR=0.47, CI 0.23–0.94).
Conclusions:
Endogenous hormones are key contributors to breast cancer observed among childhood cancer survivors. Hormone therapy given for premature ovarian insufficiency does not fully replace the function that endogenous hormones have in breast cancer development.
Similar content being viewed by others
Main
Women treated with chest radiotherapy for a pediatric malignancy have a very high risk of breast cancer. With cumulative incidence estimates ranging from 13 to 20% at age 40–45 years in all childhood cancer survivors (Bhatia et al, 2003; Kenney et al, 2004; Taylor et al, 2007) up to 35% by age 50 years in Hodgkin lymphoma (HL) survivors (Moskowitz et al, 2014), their risk compares to that observed among carriers of deleterious BRCA mutations (Taylor et al, 2007; Moskowitz et al, 2014).
Previous studies demonstrated that the magnitude of breast cancer risk in this population varies by treatment-related factors including chest radiation field (Koh et al, 2007; De Bruin et al, 2009; Lange et al, 2014; Moskowitz et al, 2014; Schaapveld et al, 2015), radiation dose to the breast tumour site (Travis et al, 2003; van Leeuwen et al, 2003; Inskip et al, 2009), and ovarian radiation (Travis et al, 2003; van Leeuwen et al, 2003; De Bruin et al, 2009; Inskip et al, 2009; Swerdlow et al, 2012; Moskowitz et al, 2014). Other factors that may modify risk but for which results differ across studies include ages at menarche and menopause, and parity (van Leeuwen et al, 2003; Hill et al, 2005; Inskip et al, 2009). Importantly, while the association of age at radiation exposure with breast cancer risk also differs across studies (Ronckers et al, 2005), recent work shows that among HL survivors the highest risk is observed among women treated with chest radiotherapy near puberty (Swerdlow et al, 2012; Cooke et al, 2013).
In the general population, there have been multiple studies evaluating the relationship between breast cancer and exposure to exogenous hormones. The presence and magnitude of risk has been dependent on the formulation and schedule of the specific hormones used in menopausal hormone therapy (HT). In particular, combination oestrogen and progestin therapy (E+P) is associated with an increased breast cancer risk compared with either no HT or HT with oestrogen alone (Chlebowski et al, 2003; Lee et al, 2005). Female survivors of childhood cancer exposed to either ovarian radiation or alkylating agents have an increased risk of premature ovarian insufficiency (POI). While POI is associated with a decreased breast cancer risk, HT is frequently used to prevent sequelae of oestrogen deficiency such as osteoporosis and impaired sexual function (Sklar et al, 2006; Panay & Kalu, 2009; van Dorp et al, 2016; Wijnen et al, 2016). It is unknown how HT affects breast cancer risk in survivors who also received chest radiotherapy. Furthermore, in the general population the association between gonadal hormonal factors and breast cancer development appears to differ by age at breast cancer diagnosis and by molecular subtype of breast cancer (Pike et al, 1981; Clavel-Chapelon & Gerber, 2002; Ma et al, 2006; Narod, 2011; Yang et al, 2011; Barnard et al, 2015; Chollet-Hinton et al, 2016). Published data on the influence of these factors on breast cancer risk after radiotherapy for childhood cancer are very sparse.
Using a large cohort of childhood cancer survivors with detailed treatment exposure data we evaluated the association between factors related to gonadal hormone exposure and the risk of radiation-associated breast cancer and characterised associations by age at onset of breast cancer and oestrogen receptor-status.
Materials and methods
Study population
The Childhood Cancer Survivor Study (CCSS) is a hospital-based retrospective cohort study with longitudinal follow-up of 5-year survivors of a cancer diagnosed prior to age 21 years at 26 participating centers in North America. Data were collected from a baseline questionnaire administered 1994–1998 and from follow-up questionnaires administered in 2000, 2003, 2005, 2007, and 2012 (available online at http://ccss.stjude.org). Next of kin were contacted for participants who died after surviving 5 years. Cohort methodology was described previously (Robison et al, 2002, 2009; Leisenring et al, 2009). The CCSS was approved by institutional review boards at participating centers. Participants provided informed consent.
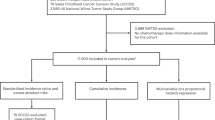
We restricted this analysis to 1108 female participants diagnosed with childhood cancer 1970–1986 who received chest radiotherapy within 5 years of their childhood cancer diagnosis and survived until at least 20 years of age. Participants treated with mantle, mediastinal (including involved field), whole lung, hemithorax (one-sided anterior chest fields), abdominal (with extension above the diagram) fields or with total body irradiation (TBI) were included. A diagram showing the flow of these participants throughout the follow-up questionnaires can be found in the Supplementary Material (Supplementary Figure S1).
Childhood cancer treatment exposures
Information on treatment received within 5 years of childhood cancer diagnosis, including radiation fields and doses and chemotherapy use, was abstracted from medical records using a standardised protocol.
We defined chest radiation field as a categorical variable ordered by size of the treatment field (TBI and whole lung, mantle, other fields). Participants treated with more than one field were included in the category for the widest field received.
The delivered dose of chest radiotherapy was taken as the sum of delivered doses (as abstracted from radiation therapy records or treatment summaries) for all chest fields. The only exception were patients treated with abdominal fields including breast tissue (including the diaphragm) and a non-overlapping chest field for whom only the dose for the superior field was included.
Cumulative doses of alkylators were determined using the Cyclophosphamide Equivalent Dose (CED) method (Green et al, 2014).
Identification of breast cancer and hormone receptor status
Breast cancers, including invasive cancers and ductal carcinoma in situ, were ascertained through self- or proxy-report and the National Death Index. Pathology reports and medical records were reviewed to confirm diagnoses. Information on hormone receptor status was abstracted. Complete information was available on oestrogen receptor status for n=114, progesterone receptor status for n=107, and HER2 status for n=64.
Endogenous hormone exposure
Across CCSS questionnaires, participants were asked about age at menarche, current menstrual status, age at last menstrual period, type of menopause (i.e., surgical or natural), pregnancy outcomes, and ages at pregnancies (<15, 15–20, 21–25, 26–30, 31–35, 36+ years). For surgical menopause, the procedure was listed (e.g., oophorectomy). We considered participants menopausal if they had not experienced normal menses for at least 6 months and other causes such as pregnancy or hormonal contraceptives could be excluded (Sklar et al, 2006).
Exogenous hormone exposure
Participants were asked in all CCSS questionnaires if they had taken oestrogens or progestin in the preceding 2 years and to list the name of the oral or other hormonal contraceptive or HT. Beginning in the Follow-up 2003 questionnaire, if they responded ‘yes’ participants were also asked to list the age at first use of the drug.
Years of ovarian function and gonadal hormone exposure after chest radiation
We counted years of normal ovarian function starting either at menarche or initiation of chest radiotherapy, whichever occurred later, until menopause, first reported use of exogenous hormones, or last contact for women who were still menstruating at last contact. Participants were censored after reported use of hormonal contraceptives or HT if they did not previously report they were post-menopausal. Women with a hysterectomy without a bilateral oophorectomy (n=45) were considered to have ovarian function until the hysterectomy and then censored at this time.
Years of gonadal hormone exposure was calculated as years of ovarian function (endogenous hormone exposure) plus years of subsequent exogenous hormone exposure. We assumed continuous exogenous hormone use from the age it was first reported until participants reported no longer taking it. If the only information on contraceptive or HT use was from questionnaires prior to 2003 we took age at which the survey was returned as age at first use.
Statistics
We used Cox proportional hazards regression to model cause-specific hazard functions with age as the time scale and modelled age at first breast cancer diagnosis. Participants were considered at risk of breast cancer beginning at age 20 years or 5 years after their primary childhood cancer diagnosis, whichever occurred later, until a late recurrence of their childhood cancer (i.e., more than 5 years after the primary diagnosis), a breast cancer diagnosis, death, or date of last contact. Participants who had a late recurrence, died, or were alive without a diagnosis of breast cancer at last contact were censored at that date. By censoring at the date of last contact, we incorporate the uncertainty that arises from participants who are lost-to-follow-up. Data were split into 1-year intervals for all analyses. Variables reflecting events occurring after age 20 years (age at first live birth, age at menopause, years of ovarian function and gonadal hormone exposure, HT) were treated as time-dependent covariates. To evaluate risk of breast cancer diagnosed before age 40 years, we included only those intervals where women were less than age 40 years at the beginning of the interval. To evaluate risk of breast cancer diagnosed at ages ⩾40 years, we included only those intervals where women were age 40 years or older at the beginning of the interval. All models were adjusted for age at childhood cancer diagnosis (using restricted cubic splines with three knots), chest radiation field and delivered dose (<20, 20–29, 30–39, 40–49, ⩾50 Gy), and exposure to anthracyclines (yes, no). All analyses involving age at first live birth were restricted to women who experienced menarche.
We assessed risk of oestrogen-receptor positive (ER+) breast cancer by modelling the hazard of a first breast cancer diagnosis being ER+. Women with breast cancer diagnoses that were not identified as ER+, including women with more than one breast cancer where an ER+ breast cancer was preceded by ER- breast cancer (n=5) or breast cancer with unknown receptor status (n=7), were censored at the date of the first breast cancer diagnosis.
To study the association between HT and breast cancer risk, we restricted the analysis to participants who never experienced menarche and, for those participants who experienced menarche, to the time after they reported menstrual periods stopped. Cox regression modelled the hazard of breast cancer after menopause as a function of combined oestrogen and progestin use, age at menopause, age at childhood cancer diagnosis, chest radiation field and delivered dose and anthracycline use. Participants entered this analysis at menopause or age 20 years, whichever occurred later, and were followed until a late recurrence, breast cancer diagnosis, death, or last contact. Participants who never experienced menarche were included from age 20 years.
Results
Overall
With a median follow-up of 26 years (range 5–38 years), 195 participants were diagnosed with breast cancer, 112 prior to age 40 years and 83 at age 40 years or older. Among women diagnosed with breast cancer, median age at breast cancer diagnosis was 38 years (range 23–58 years). Median age at menarche was13 years (range 9–20 years). Among post-menopausal women, median age at menopause was 33 years (range 11–54 years); the probability of menopause by age 40 years was approximately 34%.
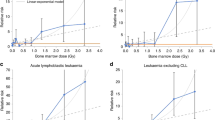
One hundred two women were diagnosed with ER+ breast cancer, 83 of these were also progesterone receptor-positive. Among the 93 other women, 24 had ER- breast cancer; receptor status was unknown for the remaining 69 women. Due to the small sample size, we were unable to evaluate risk of ER- breast cancer separately.
Further cohort characteristics are presented in Table 1 and Supplementary Table S1. All analyses presented below are adjusted for factors related to the treatment for the primary childhood cancer and for which previous work has suggested an association with the risk of breast cancer. Univariable analysis results for these adjustment factors are shown in Table 2.
Following ovarian-toxic therapy
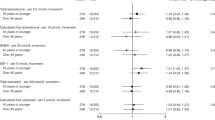
Ovarian-toxic therapy, having the ovaries in a concurrent radiation field or high doses of alkylators (CED ⩾14 000 mg m2), reduced breast cancer risk (ovarian radiation: HR=0.35, 95% CI: 0.18–0.69, P=0.002; CED ⩾14 000 mg m−2 vs no alkylators: HR=0.41, 95% CI 0.21–0.79, P=0.007). The protective effect was particularly apparent for breast cancer diagnosed ⩾40 years of age (Figures 1 and 2, Supplementary Tables S2, S4, and S5).
Risk of breast cancer overall and separately by age at breast cancer diagnosis. Estimated cause-specific hazard ratios (95% confidence intervals) for univariable associations adjusted for chest radiation field and dose, age at primary childhood cancer diagnosis, and exposure to anthracyclines. All analyses are done using age as the time scale split into 1-year intervals. Years of ovarian function represents years of normal ovarian hormone exposure starting either at menarche or initiation of chest radiotherapy, whichever occurred last, until menopause, first reported use of exogenous hormones, or last contact for women who were still menstruating at last contact. Years of gonadal hormone exposure is estimated as years of ovarian function (endogenous hormone exposure) plus years of subsequent exogenous hormone exposure.
Risk of oestrogen receptor-positive breast cancer. Estimated cause-specific hazard ratios (95% confidence intervals) for univariable associations adjusted for chest radiation field and dose, age at primary childhood cancer diagnosis, and exposure to anthracyclines. All analyses are done using age as the time scale split into 1-year intervals. Years of ovarian function represents years of normal ovarian hormone exposure starting either at menarche or initiation of chest radiotherapy, whichever occurred last, until menopause, first reported use of exogenous hormones, or last contact for women who were still menstruating at last contact. Years of gonadal hormone exposure is estimated as years of ovarian function (endogenous hormone exposure) plus years of subsequent exogenous hormone exposure.
Menstrual and reproductive factors
While breast cancer risk varied by age at menarche, especially for breast cancer diagnosed before age 40 years, the timing of chest radiotherapy relative to menarche was a notable risk factor. Women who began chest radiotherapy within 1 year of menarche had a significantly elevated risk of breast cancer compared to women who began chest radiotherapy further from menarche (Figure 1, Supplementary Tables S2, S4, S5, and S7). Removing 64 women who never experienced menarche and adjusting for age at menarche resulted in an attenuated but significant association (chest radiotherapy within 1 year of menarche vs otherwise, HR=1.66, 95% CI 1.10–2.52, P=0.017). Risk of ER+ breast cancer was similar (Figure 2, Supplementary Table S5). We found no association between age at first live birth and risk of breast cancer. There was a significant trend for risk to increase with increasing age at menopause (Ptrend=0.016), though this effect was most pronounced before age 40 years.
Years of ovarian function and hormonal exposure
Risk was more than two-fold higher for women with 10+ years of ovarian function after chest irradiation relative to women with less than 10 years of ovarian function after chest irradiation. Both risk of breast cancer diagnosed before age 40 years (HR=3.30, 95% CI 1.50–7.25, P=0.003; Figure 1, Supplementary Tables S2, S3, and S4) and risk of ER+ breast cancer (HR=5.32, 95% CI 1.88–15.06, P=0.002; Figure 2, Supplementary Table S5) were significantly increased with 10+ years of ovarian function after chest irradiation. For breast cancer diagnosed at ages ⩾40 years, estimated risk was elevated but to a lesser degree (HR=2.57, 95% CI 0.91–7.23, P=0.074).
Separately modelling the number of years of ovarian function prior to chest irradiation (median 1 year, range 0–12 years) and the number of years of ovarian function after chest irradiation (median 11 years, range 0–36 years) as continuous variables, there was no significant association between the risk of breast cancer and years prior to chest irradiation (HR=0.94 per year, 95% CI 0.81–1.09, P=0.445) while risk was significantly increased with years of ovarian function after chest irradiation (HR=1.04 per year, 95% CI 1.01–1.07, P=0.003). Including both variables in a joint model did not substantively change these results.
The association of years of gonadal hormone exposure, including both endogenous and exogenous hormone exposure, with breast cancer was markedly weaker. Risk of breast cancer diagnosed before age 40 years was elevated with 10+ years of gonadal hormone exposure although this was not statistically significant (HR=2.00, 95% CI 0.92–4.36, P=0.082). We found no association with breast cancer diagnosed at ages ⩾40 years (HR=1.08, 95% CI 0.43–2.72, P=0.873).
Among 259 menopausal women with available information on HT, risk was elevated for women reporting E+P after adjusting for age at menopause, although the association was not statistically significant (Table 3 and Supplementary Table S6). The same was true after further adjusting for age at which use was first reported (median age=28 years, range 10–51 years, HR=1.72, 95% CI 0.55–5.42, P=0.352) or when restricted to the 202 women with an age at menopause under 40 (HR=1.46, 95% CI 0.35–6.16, P=0.607). When compared with women who were still menstruating and had never reported E+P, women in menopause had a lower risk of breast cancer even with E+P (Table 4).
Discussion
Our understanding of how hormonal factors influence breast cancer risk in childhood cancer survivors exposed to chest radiotherapy is evolving. Several findings emerge from this study. Formerly evaluated only among Hodgkin lymphoma survivors (Cooke et al, 2013), we corroborate that chest radiotherapy given near menarche significantly increases breast cancer risk. As previously described, treatment with ovarian-toxic therapy substantially reduces breast cancer risk (Travis et al, 2003; van Leeuwen et al, 2003; Inskip et al, 2009; Moskowitz et al, 2014). Notably, though, use of HT in postmenopausal childhood cancer survivors does not appear to impact breast cancer risk to the same degree as endogenous hormones. Our analyses suggest that HT after treatment-induced menopause may increase breast cancer risk, but does not fully reverse the protective effect of POI.
Studies have yielded inconclusive results as to whether age at childhood cancer diagnosis modifies breast cancer risk (Metayer et al, 2000; Travis et al, 2003; Hill et al, 2005; Inskip et al, 2009; Swerdlow et al, 2012). Cooke et al (2013) observed a trend for risk to increase the nearer chest radiotherapy was to menarche with risk peaking when radiotherapy was given within 6 months of menarche relative to 10 or more years after menarche (odds ratio=5.52, 95% CI 1.97–15.46). We confirm this finding among a broader population of childhood cancer survivors. Although breast development begins 2–3 years before menarche, similar to Cooke and colleagues, we found the strongest association between breast cancer and chest radiotherapy given near menarche; the association was weaker when it was given before menarche, but this may change as the cohort matures.
A novel and clinically important finding, our data suggest that E+P menopausal HT modestly increases breast cancer risk in this population, but not to the same degree as endogenous hormones. Studies of women in natural menopause indicate that E+P increases breast cancer risk (Chlebowski et al, 2003). Whether these results are applicable to younger women experiencing POI where HT replaces hormones that would normally be produced has been previously unclear (Panay & Kalu, 2009). Similar to van Leeuwen et al (2003) and Cooke et al (2013) we found risk substantially increases with the number of premenopausal years after chest radiotherapy. However, our study is the first to find this result was attenuated when considering the number of premenopausal years after chest radiotherapy together with length of time on HT after chest radiotherapy. In postmenopausal women, breast cancer risk was elevated for women reporting E+P, although this analysis, conducted in a small subset, was not statistically significant. Finally, when comparing postmenopausal women who had taken E+P to premenopausal women, premenopausal women had a higher risk of breast cancer. Collectively these analyses point to endogenous female hormones as key contributors to the elevated risk in this population.
We attempted to evaluate that it is the number of years of ovarian function after chest radiotherapy that is the salient consideration rather the total number of years (before and after chest radiotherapy) of ovarian function. While our results do support the focus on years after chest radiotherapy, it is difficult to draw definitive conclusions from this cohort where the number of years of ovarian function prior to chest radiotherapy is restricted to a narrow range and is highly correlated with the age at which radiotherapy is given and its proximity to menarche.
Studies in other populations have shown effects of gonadal hormone factors varying by tumour hormone receptor expression status (Ma et al, 2006; Yang et al, 2011) and by age at breast cancer diagnosis (Clavel-Chapelon & Gerber, 2002; Althuis et al, 2003; Chollet-Hinton et al, 2016) suggesting that early breast cancer is a clinically and biologically different disease than breast cancer diagnosed at older ages (Althuis et al, 2003; Chollet-Hinton et al, 2016). It is unknown whether these differences are applicable to radiation-associated breast cancer in childhood cancer survivors. We observed differences in the strength of associations between multiple risk factors, (ovarian radiation, high doses of alkylators, age at menarche, timing of chest radiotherapy relative to menarche, and years of ovarian function after chest radiotherapy) with breast cancer diagnosed earlier vs later. It may be that the mechanisms by which these factors modify breast cancer risk differ by age at breast cancer diagnosis or menopausal status. However, this is a relatively young cohort limiting our ability to test whether these are true differences. Further, due to the era in which many of the breast cancers were diagnosed, we lacked hormone receptor expression on many cancers and HER2 status on most cancers and thus were unable to evaluate risk according to luminal type.
In agreement with our previous report (Moskowitz et al, 2014), our data indicate that higher doses of delivered chest radiotherapy do not confer a statistically significantly higher risk of breast cancer. Lower doses of therapeutic radiation delivered to wide chest fields (e.g., whole lung irradiation) are associated with elevated breast cancer risk. These results are in contrast to the linear dose-response relationship previously observed between the absorbed dose of radiation to the breast as estimated by radiation dosimetry and breast cancer risk (Guibout et al, 2005; Inskip et al, 2009). Because delivered doses of chest radiotherapy are highly correlated with the delivered chest field (e.g., mantle field irradiation was typically used with delivered doses of 35 Gy or higher whereas whole lung irradiation and total body irradiation are used with delivered doses of 20 Gy or less), it is difficult to disentangle the effect of the delivered dose and the effect of the delivered field which may account for these discrepant findings.
Our results should be interpreted in light of several considerations. Aside from treatment-related factors, data for hormonal factors and medication use were self-reported without external validation. When participants did not reply to later questionnaires, but reported exogenous hormone use at the baseline survey, we were unable to reconstruct age at first use. In these cases, we used age at the time of the survey as age at first use, but likely miss some years. Notably, it was difficult to tease apart exogenous hormone use for contraception vs HT in this population. The risk we observed for premenopausal women reporting hormone use relative to premenopausal women without any hormone use may be underestimated due to instances when women were prescribed oral contraceptive pills as HT. Future work should focus on exploring and understanding possible differences in breast cancer risk associated with using oral contraceptive pills as HT as opposed to traditional HT. In some cases where women reported both oestrogen and progestin use, it was difficult to know if use occurred concurrently or sequentially. Previous work has shown that concurrent use in the U.S. has a no greater risk than sequential use possibly due to a reduction in progestin dose with concurrent use (Lee et al, 2005). Finally, we were unable to test for differences by age at breast cancer diagnosis due to small sample sizes.
In conclusion, chest radiotherapy substantially increases breast cancer risk, particularly when administered near menarche. Ovarian-toxic therapy significantly reduces this risk, but women treated with chest radiotherapy and ovarian-toxic therapy still have a significantly elevated risk compared with the general population (Moskowitz et al, 2014). Among women with POI, E+P modestly increases breast cancer risk. In spite of this increase, however, women with POI who take E+P have a lower risk of breast cancer when compared with women who continue to menstruate naturally (i.e., normal endogenous hormone function).
Change history
11 July 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Althuis MD, Brogan DD, Coates RJ, Daling JR, Gammon MD, Malone KE, Schoenberg JB, Brinton LA (2003) Breast cancers among very young premenopausal women (United States). Cancer Causes Control 14 (2): 151–160.
Barnard ME, Boeke CE, Tamimi RM (2015) Established breast cancer risk factors and risk of intrinsic tumor subtypes. Biochim Biophys Acta 1856 (1): 73–85.
Bhatia S, Yasui Y, Robison LL, Birch JM, Bogue MK, Diller L, DeLaat C, Fossati-Bellani F, Morgan E, Oberlin O, Reaman G, Ruymann FB, Tersak J, Meadows AT Late Effects Study G (2003) High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin’s disease: report from the Late Effects Study Group. J Clin Oncol 21 (23): 4386–4394.
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA, Khandekar J, Petrovitch H, McTiernan A Women’s Health Initiative Investigators (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA 289 (24): 3243–3253.
Chollet-Hinton L, Anders CK, Tse CK, Bell MB, Yang YC, Carey LA, Olshan AF, Troester MA (2016) Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res 18 (1): 79.
Clavel-Chapelon F, Gerber M (2002) Reproductive factors and breast cancer risk. Do they differ according to age at diagnosis? Breast Cancer Res Treat 72 (2): 107–115.
Cooke R, Jones ME, Cunningham D, Falk SJ, Gilson D, Hancock BW, Harris SJ, Horwich A, Hoskin PJ, Illidge T, Linch DC, Lister TA, Lucraft HH, Radford JA, Stevens AM, Syndikus I, Williams MV, England, Wales Hodgkin Lymphoma Follow-up G, Swerdlow AJ (2013) Breast cancer risk following Hodgkin lymphoma radiotherapy in relation to menstrual and reproductive factors. Br J Cancer 108 (11): 2399–2406.
De Bruin ML, Sparidans J, van’t Veer MB, Noordijk EM, Louwman MW, Zijlstra JM, van den Berg H, Russell NS, Broeks A, Baaijens MH, Aleman BM, van Leeuwen FE (2009) Breast cancer risk in female survivors of Hodgkin’s lymphoma: lower risk after smaller radiation volumes. J Clin Oncol 27 (26): 4239–4246.
Green DM, Nolan VG, Goodman PJ, Whitton JA, Srivastava D, Leisenring WM, Neglia JP, Sklar CA, Kaste SC, Hudson MM, Diller LR, Stovall M, Donaldson SS, Robison LL (2014) The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer 61 (1): 53–67.
Guibout C, Adjadj E, Rubino C, Shamsaldin A, Grimaud E, Hawkins M, Mathieu MC, Oberlin O, Zucker JM, Panis X, Lagrange JL, Daly-Schveitzer N, Chavaudra J, de Vathaire F (2005) Malignant breast tumors after radiotherapy for a first cancer during childhood. J Clin Oncol 23 (1): 197–204.
Hill DA, Gilbert E, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, Glimelius B, Andersson M, Wiklund T, Lynch CF, Van’t Veer M, Storm H, Pukkala E, Stovall M, Curtis RE, Allan JM, Boice JD, Travis LB (2005) Breast cancer risk following radiotherapy for Hodgkin lymphoma: modification by other risk factors. Blood 106 (10): 3358–3365.
Inskip PD, Robison LL, Stovall M, Smith SA, Hammond S, Mertens AC, Whitton JA, Diller L, Kenney L, Donaldson SS, Meadows AT, Neglia JP (2009) Radiation dose and breast cancer risk in the Childhood Cancer Survivor Study. J Clin Oncol 27 (24): 3901–3907.
Kenney LB, Yasui Y, Inskip PD, Hammond S, Neglia JP, Mertens AC, Meadows AT, Friedman D, Robison LL, Diller L (2004) Breast cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Intern Med 141 (8): 590–597.
Koh ES, Tran TH, Heydarian M, Sachs RK, Tsang RW, Brenner DJ, Pintilie M, Xu T, Chung J, Paul N, Hodgson DC (2007) A comparison of mantle versus involved-field radiotherapy for Hodgkin’s lymphoma: reduction in normal tissue dose and second cancer risk. Radiat Oncol 2: 13.
Lange JM, Takashima JR, Peterson SM, Kalapurakal JA, Green DM, Breslow NE (2014) Breast cancer in female survivors of Wilms tumor: a report from the national Wilms tumor late effects study. Cancer 120 (23): 3722–3730.
Lee SA, Ross RK, Pike MC (2005) An overview of menopausal oestrogen-progestin hormone therapy and breast cancer risk. Br J Cancer 92 (11): 2049–2058.
Leisenring WM, Mertens AC, Armstrong GT, Stovall MA, Neglia JP, Lanctot JQ, Boice JD Jr, Whitton JA, Yasui Y (2009) Pediatric cancer survivorship research: experience of the Childhood Cancer Survivor Study. J Clin Oncol 27 (14): 2319–2327.
Ma H, Bernstein L, Pike MC, Ursin G (2006) Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res 8 (4): R43.
Metayer C, Lynch CF, Clarke EA, Glimelius B, Storm H, Pukkala E, Joensuu T, van Leeuwen FE, van’t Veer MB, Curtis RE, Holowaty EJ, Andersson M, Wiklund T, Gospodarowicz M, Travis LB (2000) Second cancers among long-term survivors of Hodgkin’s disease diagnosed in childhood and adolescence. J Clin Oncol 18 (12): 2435–2443.
Moskowitz CS, Chou JF, Wolden SL, Bernstein JL, Malhotra J, Novetsky Friedman D, Mubdi NZ, Leisenring WM, Stovall M, Hammond S, Smith SA, Henderson TO, Boice JD, Hudson MM, Diller LR, Bhatia S, Kenney LB, Neglia JP, Begg CB, Robison LL, Oeffinger KC (2014) Breast cancer after chest radiation therapy for childhood cancer. J Clin Oncol 32 (21): 2217–2223.
Narod SA (2011) Hormone replacement therapy and the risk of breast cancer. Nat Rev Clin Oncol 8 (11): 669–676.
Panay N, Kalu E (2009) Management of premature ovarian failure. Best Pract Res Clin Obstetr Gynaecol 23 (1): 129–140.
Pike MC, Henderson BE, Casagrande JT, Rosario I, Gray GE (1981) Oral contraceptive use and early abortion as risk factors for breast cancer in young women. Br J Cancer 43 (1): 72–76.
Robison LL, Armstrong GT, Boice JD, Chow EJ, Davies SM, Donaldson SS, Green DM, Hammond S, Meadows AT, Mertens AC, Mulvihill JJ, Nathan PC, Neglia JP, Packer RJ, Rajaraman P, Sklar CA, Stovall M, Strong LC, Yasui Y, Zeltzer LK (2009) The Childhood Cancer Survivor Study: a National Cancer Institute-supported resource for outcome and intervention research. J Clin Oncol 27 (14): 2308–2318.
Robison LL, Mertens AC, Boice JD, Breslow NE, Donaldson SS, Green DM, Li FP, Meadows AT, Mulvihill JJ, Neglia JP, Nesbit ME, Packer RJ, Potter JD, Sklar CA, Smith MA, Stovall M, Strong LC, Yasui Y, Zeltzer LK (2002) Study design and cohort characteristics of the Childhood Cancer Survivor Study: a multi-institutional collaborative project. Med Pediatr Oncol 38 (4): 229–239.
Ronckers CM, Erdmann CA, Land CE (2005) Radiation and breast cancer: a review of current evidence. Breast Cancer Res 7 (1): 21–32.
Schaapveld M, Aleman BM, van Eggermond AM, Janus CP, Krol AD, van der Maazen RW, Roesink J, Raemaekers JM, de Boer JP, Zijlstra JM, van Imhoff GW, Petersen EJ, Poortmans PM, Beijert M, Lybeert ML, Mulder I, Visser O, Louwman MW, Krul IM, Lugtenburg PJ, van Leeuwen FE (2015) Second cancer risk up to 40 years after treatment for Hodgkin’s lymphoma. N Engl J Med 373 (26): 2499–2511.
Sklar CA, Mertens AC, Mitby P, Whitton J, Stovall M, Kasper C, Mulder J, Green D, Nicholson HS, Yasui Y, Robison LL (2006) Premature menopause in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst 98 (13): 890–896.
Swerdlow AJ, Cooke R, Bates A, Cunningham D, Falk SJ, Gilson D, Hancock BW, Harris SJ, Horwich A, Hoskin PJ, Linch DC, Lister TA, Lucraft HH, Radford JA, Stevens AM, Syndikus I, Williams MV (2012) Breast cancer risk after supradiaphragmatic radiotherapy for Hodgkin’s lymphoma in England and Wales: a National Cohort Study. J Clin Oncol 30 (22): 2745–2752.
Taylor AJ, Winter DL, Stiller CA, Murphy M, Hawkins MM (2007) Risk of breast cancer in female survivors of childhood Hodgkin’s disease in Britain: a population-based study. Int J Cancer 120 (2): 384–391.
Travis LB, Hill DA, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, Glimelius B, Andersson M, Wiklund T, Lynch CF, Van’t Veer MB, Glimelius I, Storm H, Pukkala E, Stovall M, Curtis R, Boice JD Jr, Gilbert E (2003) Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA 290 (4): 465–475.
van Dorp W, Mulder RL, Kremer LC, Hudson MM, van den Heuvel-Eibrink MM, van den Berg MH, Levine JM, van Dulmen-den Broeder E, di Iorgi N, Albanese A, Armenian SH, Bhatia S, Constine LS, Corrias A, Deans R, Dirksen U, Gracia CR, Hjorth L, Kroon L, Lambalk CB, Landier W, Levitt G, Leiper A, Meacham L, Mussa A, Neggers SJ, Oeffinger KC, Revelli A, van Santen HM, Skinner R, Toogood A, Wallace WH, Haupt R (2016) Recommendations for premature ovarian insufficiency surveillance for female survivors of childhood, adolescent, and young adult cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in Collaboration With the PanCareSurFup Consortium. J Clin Oncol 34 (28): 3440–3450.
van Leeuwen FE, Klokman WJ, Stovall M, Dahler EC, van’t Veer MB, Noordijk EM, Crommelin MA, Aleman BM, Broeks A, Gospodarowicz M, Travis LB, Russell NS (2003) Roles of radiation dose, chemotherapy, and hormonal factors in breast cancer following Hodgkin’s disease. J Natl Cancer Inst 95 (13): 971–980.
Wijnen M, van den Heuvel-Eibrink MM, Medici M, Peeters RP, van der Lely AJ, Neggers SJ (2016) Risk factors for subsequent endocrine-related cancer in childhood cancer survivors. Endocr Relat Cancer 23 (6): R299–R321.
Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, Gaudet M, Schmidt MK, Broeks A, Cox A, Fasching PA, Hein R, Spurdle AB, Blows F, Driver K, Flesch-Janys D, Heinz J, Sinn P, Vrieling A, Heikkinen T, Aittomaki K, Heikkila P, Blomqvist C, Lissowska J, Peplonska B, Chanock S, Figueroa J, Brinton L, Hall P, Czene K, Humphreys K, Darabi H, Liu J, Van’t Veer LJ, van Leeuwen FE, Andrulis IL, Glendon G, Knight JA, Mulligan AM, O’Malley FP, Weerasooriya N, John EM, Beckmann MW, Hartmann A, Weihbrecht SB, Wachter DL, Jud SM, Loehberg CR, Baglietto L, English DR, Giles GG, McLean CA, Severi G, Lambrechts D, Vandorpe T, Weltens C, Paridaens R, Smeets A, Neven P, Wildiers H, Wang X, Olson JE, Cafourek V, Fredericksen Z, Kosel M, Vachon C, Cramp HE, Connley D, Cross SS, Balasubramanian SP, Reed MW, Dork T, Bremer M, Meyer A, Karstens JH, Ay A, Park-Simon TW, Hillemanns P, Arias Perez JI, Menendez Rodriguez P, Zamora P, Benitez J, Ko YD, Fischer HP, Hamann U, Pesch B, Bruning T, Justenhoven C, Brauch H, Eccles DM, Tapper WJ, Gerty SM, Sawyer EJ, Tomlinson IP, Jones A, Kerin M, Miller N, McInerney N, Anton-Culver H, Ziogas A, Shen CY, Hsiung CN, Wu PE, Yang SL, Yu JC, Chen ST, Hsu GC, Haiman CA, Henderson BE, Le Marchand L, Kolonel LN, Lindblom A, Margolin S, Jakubowska A, Lubinski J, Huzarski T, Byrski T, Gorski B, Gronwald J, Hooning MJ, Hollestelle A, van den Ouweland AM, Jager A, Kriege M, Tilanus-Linthorst MM, Collee M, Wang-Gohrke S, Pylkas K, Jukkola-Vuorinen A, Mononen K, Grip M, Hirvikoski P, Winqvist R, Mannermaa A, Kosma VM, Kauppinen J, Kataja V, Auvinen P, Soini Y, Sironen R, Bojesen SE, Orsted DD, Kaur-Knudsen D, Flyger H, Nordestgaard BG, Holland H, Chenevix-Trench G, Manoukian S, Barile M, Radice P, Hankinson SE, Hunter DJ, Tamimi R, Sangrajrang S, Brennan P, McKay J, Odefrey F, Gaborieau V, Devilee P, Huijts PE, Tollenaar RA, Seynaeve C, Dite GS, Apicella C, Hopper JL, Hammet F, Tsimiklis H, Smith LD, Southey MC, Humphreys MK, Easton D, Pharoah P, Sherman ME, Garcia-Closas M (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103 (3): 250–263.
Acknowledgements
This work was supported by grants from the National Cancer Institute (U24CA55727, PI: GT Armstrong; R01CA136783, PI: CS Moskowitz; K05CA160724 and R01CA134722, PI: KC Oeffinger; P30CA21765, PI: C Roberts; and the Memorial Sloan Kettering Cancer Center Core Grant P30 CA008748), and the Meg Berté Owen Foundation. Support to St Jude Children’s Research Hospital was also provided by the American Lebanese-Syrian Associated Charities (ALSAC). Support to CM Ronckers was provided by the Dutch Cancer Society (#2012-5517).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Moskowitz, C., Chou, J., Sklar, C. et al. Radiation-associated breast cancer and gonadal hormone exposure: a report from the Childhood Cancer Survivor Study. Br J Cancer 117, 290–299 (2017). https://doi.org/10.1038/bjc.2017.169
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.169
Keywords
This article is cited by
-
International recommendations for screening and preventative practices for long-term survivors of transplantation and cellular therapy: a 2023 update
Bone Marrow Transplantation (2024)
-
Subsequent female breast cancer risk associated with anthracycline chemotherapy for childhood cancer
Nature Medicine (2023)
-
A systematic approach to the endocrine care of survivors of pediatric hematopoietic stem cell transplantation
Cancer and Metastasis Reviews (2020)