Abstract
Background:
Copper and zinc are essential micronutrients and cofactors of many enzymatic reactions that may be involved in liver-cancer development. We aimed to assess pre-diagnostic circulating levels of copper, zinc and their ratio (Cu/Zn) in relation to hepatocellular carcinoma (HCC), intrahepatic bile duct (IHBD) and gall bladder and biliary tract (GBTC) cancers.
Methods:
A nested case–control study was conducted within the European Prospective Investigation into Cancer and Nutrition cohort. Serum zinc and copper levels were measured in baseline blood samples by total reflection X-ray fluorescence in cancer cases (HCC n=106, IHDB n=34, GBTC n=96) and their matched controls (1:1). The Cu/Zn ratio, an indicator of the balance between the micronutrients, was computed. Multivariable adjusted odds ratios and 95% confidence intervals (OR; 95% CI) were used to estimate cancer risk.
Results:
For HCC, the highest vs lowest tertile showed a strong inverse association for zinc (OR=0.36; 95% CI: 0.13–0.98, Ptrend=0.0123), but no association for copper (OR=1.06; 95% CI: 0.45–2.46, Ptrend=0.8878) in multivariable models. The calculated Cu/Zn ratio showed a positive association for HCC (OR=4.63; 95% CI: 1.41–15.27, Ptrend=0.0135). For IHBC and GBTC, no significant associations were observed.
Conclusions:
Zinc may have a role in preventing liver-cancer development, but this finding requires further investigation in other settings.
Similar content being viewed by others
Main
Hepatocellular carcinoma (HCC) and intrahepatic bile duct (IHBC) cancers are two subtypes of liver cancer, where HCC is the most common (Page et al, 2014). The prognosis for liver cancer is poor with overall mortality to incidence rate reaching 95%, making it the second deadliest cancer worldwide (Globocan, 2012). Main known risk factors for liver cancers include hepatitis infection, aflatoxin exposure, heavy alcohol intake, smoking, body fatness and non-alcoholic fatty liver disease (NAFLD; Gomaa et al, 2008; Augustine and Fong, 2014). In addition to the established factors, chronic inflammatory and oxidative pathways may be involved in liver-cancer development as a consequence of free radical damage to hepatocytes (Bishayee, 2014).
Zinc and copper are essential micronutrients whose levels are controlled by their rate of absorption in the intestine and excretion with bile (Hotz et al, 2003; Iakovidis et al, 2011; Osredkar, 2011). The richest food sources of zinc and copper include meat, shellfish, offal, seeds and nuts, whole grains, beans and chocolate (Ma and Betts, 2000). Both zinc and copper are cofactors for many enzymatic reactions, including the copper–zinc-dependent superoxide dismutase (Cu/Zn-SOD) with antioxidant functions that requires adequate zinc and copper to support cellular defence systems against reactive oxygen species (ROS; Osredkar, 2011). It is suspected that the disruption of copper–zinc homoeostasis and overproduction of ROS may lead to DNA damage, protein modification and possibly to cancer development (Osredkar, 2011). Although copper deficiency may diminish Cu/Zn-SOD activity and impair antioxidant defences (Aigner et al, 2015), at high levels copper may exhibit toxic effects, particularly in the liver where it is stored (Iakovidis et al, 2011). Excess circulating copper in relation to zinc has been shown to increase lipid peroxidation and deplete glutathione (GSH) reserves in rat liver (Ozcelik et al, 2003).
A disruption of zinc and/or copper homoeostasis has been observed in different stages of liver diseases (Sawa, 1990; Hyun et al, 1992; Lin et al, 2006; Guo et al, 2013) and was linked to altered production of carrier proteins for these micronutrients in response to inflammatory signals or because of impaired liver synthesis (Deshmukh et al, 1985; Brown et al, 2004). In fact, information from case–control studies indicates higher circulating copper and lower zinc levels in patients with hepatitis C (Ko et al, 2005) and liver cirrhosis (Rahelic et al, 2006; Nangliya et al, 2015). Additional evidence suggests a link between hepatitis C infection and higher antioxidant enzyme Cu/Zn-SOD activity which has also been observed to be high in liver biopsies of NAFLD patients (Ko et al, 2005; Perlemuter et al, 2005). Both of these disorders are related to oxidative stress and inflammatory pathways (Satapati et al, 2015; Piciocchi et al, 2016) and are risk factors for liver cancers (Augustine and Fong, 2014). Specific to liver cancers, two case–control studies have reported decreased levels of zinc and increased levels of copper and Cu/Zn ratio in patients with gall bladder carcinoma (Gupta et al, 2005) and HCC (Poo et al, 2003). The only existing evidence in a prospective setting, the Shanghai Women’s Health Study and the Shanghai Men’s Health Study, found no significant liver-cancer risk associations (Ma et al, 2017). But the study was based on dietary zinc and copper intake estimates which are likely to have considerable measurement errors. A prospective study based on biomarkers of copper and zinc status is lacking in the current literature.
In this case–control study nested within a large prospective multicentre cohort, we measured baseline circulating levels of these two microelements and related them to the later incidence of cancers located within the liver (HCC, IHBC) and the anatomically related cancers of the gall bladder and biliary tract (GBTC). Additional understanding on possible underlying mechanisms of liver-cancer development may provide greater insight into prevention strategies and modifiable determinants.
Materials and methods
Study design and participants
The European Prospective Investigation into Cancer and Nutrition (EPIC) study is a multicentre prospective cohort study from 23 centres in 10 European countries (Denmark, France, Germany, Greece, Italy, The Netherlands, Norway, Spain, Sweden, and the United Kingdom) (Riboli and Kaaks, 1997). Between 1992 and 2000 over 520 000 men and women were recruited for whom socio-demographic, dietary (using validated country-specific food frequency questionnaires), lifestyle, anthropometric data and biological samples (from approximately 80% participants) were collected at baseline. Samples from all countries are stored in −196 °C liquid nitrogen at the International Agency for Research on Cancer (IARC, Lyon, France), except Denmark (at −150 °C under nitrogen vapour) and Sweden (−80 °C freezers). Written informed consent was collected from all participants. Approval for the EPIC study was obtained from the IARC Ethical Review Committee and the relevant Ethical Review Boards of the participating institutions.
Cancer incidence and case ascertainment
For this specific analysis, determination of cancer incidence is complete up to December 2006, conducted by record linkage with regional cancer registries. Exceptions are France, Germany and Greece where a combination of methods was used (health insurance records, contacts with cancer and pathology registries, active follow-up) and is complete up to June 2010.
Cases were identified according to the 10th revision of the International Statistical Classification of Diseases, Injury and Causes of Death (ICD10) and the 2nd edition of the International Classification of Diseases for Oncology (ICD-O-2). HCC was defined as C22.0. GBTC were defined as tumours in the gall bladder (C23.9), extrahepatic bile ducts (C24.0), ampulla of Vater (C24.1) and biliary tract (C24.8 and C24.9). IHBD were defined as C22.1. For each identified case, the histology and the methods used for diagnosis were reviewed and metastatic cases or other types of primary liver cancer were excluded. In detail, from all recruited cohort participants, 23 818 subjects with prevalent cancer other than non-melanoma skin cancer, 4380 with incomplete follow-up data or missing information on the date of diagnosis, 6192 with missing dietary information, 60 with missing lifestyle information, and 9596 who were at the top or bottom 1% of the distribution of the ratio of reported energy intake to energy requirement, and 78 with metastasis in the liver or ineligible histology code were excluded from the above classifications, which were conducted on 477 206 eligible participants.
Nested case–control study design
The present analyses are based on a nested case–control subset of the EPIC cohort (for full description see (Trichopoulos et al, 2011)), and include 106 HCC subjects with available biological samples from seven out of ten European countries participating in EPIC (excluding France, Sweden and Norway). Additional analyses were conducted for 34 IHBC and 96 GBTC cases. Each case was matched to a cohort participant who was free of cancer and alive at the time of diagnosis of the case. Control subjects were matched (1:1) using incidence density sampling from all cohort members by: age at blood collection (±1 year), sex, study centre, time of the day at blood collection (±3 h), fasting status at blood collection (<3, 3–6, and >6 h); among women, additionally by menopausal status (pre-, peri-, and postmenopausal), and hormone replacement therapy use at time of blood collection (yes/no).
Laboratory assays
Duplicate samples of 20 μl of serum were analysed at Charité University Medical School (Berlin, Germany) in a bench-top total reflection X-ray fluorescence (TXRF) spectrometer (Picofox S2, Bruker Nano GmbH, Berlin, Germany), as described earlier (Hughes et al, 2016). Fluorescence of copper and zinc were determined from the emission spectrograms, and the concentrations were determined in relation to a gallium standard added as internal calibrator. The Seronorm Trace Elements Serum L-2 (LOT 0903107, SERO AS, Billingstad, Norway) was used as standard to verify recovery of copper and zinc within the reference concentrations. Samples for which the coefficient of variation (CV) was higher than 10% (n=24 and 39 for copper and zinc, respectively) were re-analysed. Two serum samples of known concentration per each biomarker were used as controls in each plate. Inter-plate CVs were computed and evaluated using GraphPad Prism 6.01 (La Jolla, CA, USA). The coefficients were 9% for copper and 6.9% for zinc.
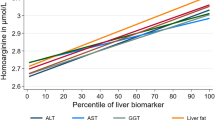
The present analysis made secondary use of existing biomarker measurements of hepatitis infection status (measured by HBsAg and anti-HCV assays), inflammatory marker high sensitivity CRP (hsCRP), alpha-fetoprotein (AFP), liver function biomarkers (gamma-glutamyltransferase, GGT; alanine aminotransferase, ALT; aspartate aminotransferase, AST; alkaline phosphatase, ALP; total bilirubin and albumin) available for a subset of participants. Circulating levels of these biomarkers at recruitment were previously determined using standard protocols at the Centre de Biologie République laboratory, Lyon, France, as described elsewhere (Stepien et al, 2016b). Measurements of amino acids for the calculation of the Fischer’s ratio (ratio of branched chain (isoleucine, leucine, valine) to aromatic (phenylalanine+tyrosine) amino acids; a clinical indicator of severity of liver dysfunction (Ishikawa, 2012) was formerly performed using a targeted metabolomics approach (Biocrates Life Sciences, Innsbruck, Austria), as previously detailed (Stepien et al, 2016a).
Statistical analyses
Comparisons of the baseline subject characteristics for continuous variables were conducted with the t-test for continuous and Fisher’s exact test for categorical variables other than the matching factors. The Cu/Zn ratio was computed by dividing the concentration of copper by that of zinc. Crude and sex-, country- and fasting status-adjusted general linear models (GLM) were used to compare biomarker levels among controls by each potential confounder category. Threshold for the Fischer’s ratio median category was based on median values for control subjects for each cancer subsite.
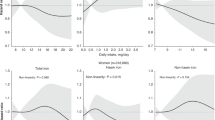
Conditional logistic regression models were used to calculate odds ratios (OR) and 95% confidence intervals (95% CI) for baseline serum copper (per 25 μg dl−1), zinc (per 20 μg dl−1) and Cu/Zn levels (per 0.33 unit), as an approximation of a standard deviation (1 s.d.) increase, in relation to risk of HCC, IHBC and GBTC separately. Categorical analyses for HCC and GBTC were conducted by tertiles of copper, zinc and Cu/Zn ratio. Thirds were defined using sex-specific tertile cut-points in the distribution of concentrations in control participants for each cancer subsite. Sex-specific categories were used because of an apparent heterogeneity of circulating levels between men and women and limited power for sub-group analyses based on low sample size, particularly of women. Crude models were conditioned on the matching criteria (model 1). Multivariable models were additionally adjusted for the following a priori selected confounders: body mass index (BMI), physical activity, alcohol intake at recruitment, lifetime alcohol intake pattern, smoking status, highest level of attained education (model 2; see Table 1 for additional information). Other potential confounders were considered but not kept in the model because they did not modify risk estimates by more than 10%, including daily intakes of: meat and meet products, fruits, nuts and seeds, legumes, cereal products, fish and shellfish, coffee, and self-reported diabetes status at baseline. For HCC, a third model was also applied with additional adjustment for hepatitis B/C infection status (model 3). Additional analyses were performed with model 2, adjusting additionally also for: the liver function score, the Fischer’s ratio category (see footnotes f and g in Table 1, respectively, both of which are indicative of possible liver impairment/damage), diabetes status, inflammatory marker hsCRP and circulating albumin levels, which is the carrier protein for zinc in the circulation and whose production may be altered in the event of liver impairment. Cut-offs for categories of hsCRP and albumin were 3 mg l−1 and 34 g l−1, respectively, as previously employed (Stepien et al, 2016b). To maintain all subjects in the analyses, a category of missing data was created for all the additional variables. Sensitivity analyses excluding the missing category were performed. Restricted cubic spline curves were constructed to visualise the dose–response association between biomarker levels and IHBC and GBTC risk. Minimum value for all participants was chosen as a reference and three knots were employed. The OR (95% CI) are presented on log10 scale in relation to continues values of the biomarkers (μg dl−1 or units).
As an attempt to control for potential reverse causation, subjects with a short follow-up of <2 years after blood collection were excluded. As hepatitis infection, an established risk factor for liver cancers may alter liver function and hence circulating copper and zinc levels, additional sensitivity analyses were performed by excluding hepatitis positive subjects. Sub-group analyses based on hepatitis negative subjects were conducted using continuous unconditional logistic regression models adjusted for sex, country and age at recruitment. Additional sensitivity analyses were performed excluding samples from Denmark and Sweden, where bio-sample storage conditions differed from those at the IARC biobank.
Analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC, USA). All statistical tests were two-sided and P-values <0.05 were considered statistically significant.
Results
Baseline characteristics
Anthropometric and lifestyle characteristics by HCC status are displayed in Table 1. More HCC cases were current smokers (P=0.0054) and former alcohol drinkers (P=0.0025), had abnormal liver function tests (P=0.005), belonged to lower median for the Fischer’s ratio (⩽0.0001), indicating possible impairment of their liver functions, and had higher Cu/Zn ratio (P=0.0001). Five HCC cases had zinc levels in the range of deficiency (below 70 μg dl−1), none were copper deficient (<63 μg dl−1) and 10 cases had low albumin levels (<34 g l−1). Results for GBTC and IHBC are presented in Supplementary Table 1; there were no significant differences between cases and controls. For the levels of copper, zinc and their ratio by matching factors and potential confounder categories see Supplementary Table 2. In brief, in the GLM sex, country and fasting status- adjusted models zinc levels were significantly different among education level, physical activity, and hepatitis and diabetes status categories. Both copper and its ratio to zinc varied between smoking, physical activity, hsCRP categories, but only the Cu/Zn ratio was different among categories of liver function indices (score and the Fischer’s ratio).
Associations with HCC risk
Associations between zinc, copper and Cu/Zn ratio with HCC risk are shown in Table 2. Higher serum zinc levels were inversely associated with HCC risk in crude (model 1, OR=0.39; 95% CI: 0.19–0.81 for 3rd vs 1st tertile, Ptrend=0.0072) and multivariable adjusted models (model 2, OR=0.36; 95% CI: 0.13–0.98 for 3rd vs 1st tertile, Ptrend=0.0123). Each 20 μg dl−1 increase in circulating zinc was associated with 45% (OR=0.55; 95% CI: 0.39–0.78) and 47% (OR=0.53; 95% CI: 0.33–0.84) lower HCC risk in models 1 and 2, respectively. For copper, no significant associations were observed with HCC risk in any of the analytic models. For the Cu/Zn, the third tertile was significantly associated with increased HCC risk compared with the reference category (model 1: OR=4.75; 95% CI: 1.86, 12.12, Ptrend=0.0029; model 2: OR=4.63; 95% CI: 1.41, 15.27, Ptrend=0.0135). Each 1 s.d. increase of Cu/Zn ratio was associated with higher HCC risk (model 1: OR=2.29; 95% CI: 1.52, 3.46; model 2: OR=2.53; 95% CI: 1.44, 4.46). Further adjustment for hepatitis status (model 3) attenuated the strength of effects and associations lost statistical significance in the top category (Table 2). Additional adjustment of the model 2 for the liver function score, the Fischer’s ratio, hsCRP, diabetes status and albumin (for zinc) categories resulted in similar findings as obtained from the hepatitis adjusted model 3 (Supplementary Table 3). Exclusion of missing categories for the above variables did not modify the findings.
Additional analyses on the associations between zinc and copper and IHBC and GBTC risks are presented in Supplementary Figure 1. For these cancer sites, no statistically significant associations were observed for any of the biomarkers measured. Exclusion of the two countries that did not store their samples in IARC (n=15 and 12 case–control sets for HCC and GBTC, respectively) did not change the risk estimates.
Sensitivity analyses
In sensitivity analyses, exclusion of cases and matched controls (n=19 case-sets) with a follow-up period of <2 years did not significantly modify the findings in continuous analyses (model 2 for zinc: OR=0.60; 95% CI: 0.36, 1.02 and Cu/Zn ratio: OR=7.80; 95% CI: 1.07, 56.84, Supplementary Table 4A). For copper, null associations were observed (OR=1.00; 95% CI: 0.66, 1.51). Similar risk estimates were obtained after exclusion of 68 subjects with <4 years of follow-up, although these analyses are based on low number of subjects (n=72 case-sets) (data not shown).
Restricting these analyses to hepatitis negative participants (44 cases, 66 controls, not matched, Supplementary Table 4B), we observed a statistically significantly higher risk of HCC per 1 s.d. increase for Cu/Zn ratio (OR=2.23; 95% CI: 1.17, 4.29) and no apparent change in the magnitude of the effect estimates for zinc (OR per 20 μg dl−1=0.55; 95% CI: 0.29, 1.02) and copper (OR per 25 μg dl−1=1.15; 95% CI: 0.73, 1.83) in fully adjusted model. In crude models adjusted only for the matching factors, zinc was significantly negatively (OR=0.56; 95% CI: 0.35, 0.90) and Cu/Zn ratio positively (OR=2.45; 95% CI: 1.49, 4.05) associated with HCC, whereas for copper the association was not significant (OR=1.35; 95% CI: 0.92, 1.98).
Discussion
In this prospective study we observed an inverse association between circulating levels of zinc with risk of development of HCC, but not IHBC nor GBTC. The association with HCC may not be fully independent of hepatitis status or extent of liver dysfunction. Although higher copper levels were not associated with risk of hepatobiliary cancers, its increased levels in relation to zinc demonstrated a positive HCC risk association. To our knowledge this is the first prospective investigation on these associations to date.
The possible roles of zinc and copper in development of cancers at several anatomical sites have been previously explored in experimental settings (Theophanides and Anastassopoulou, 2002; Franklin and Costello, 2009). A meta-analysis of six case–control studies predominantly conducted among Asian populations which showed that an imbalance between circulating levels of copper and zinc may be associated with bladder cancer development (Mao and Huang, 2013) was in line with our findings. Differences in the Cu/Zn ratio have also been noted comparing blood and tissue samples in malignant vs benign ovarian (Lightman et al, 1986) and lung (Diez et al, 1989) tumours. Other data from a small French cohort study (Leone et al, 2006) and the US NHANES study (Wu et al, 2004) also suggest an association between high circulating levels of copper and lower zinc with cancer mortality. A prospective cohort from Iran indicated an inverse association between dietary zinc and non-linear tend for copper with oesophageal cancer risk (Hashemian et al, 2015).
Zinc is thought to have an important role in development and progression of chronic liver diseases and HCC (Costello and Franklin, 2014). Lower circulating zinc levels have been observed in these disorders (Costello and Franklin, 2014), possibly due to impaired hepatic function and lower production of albumin, the carrier protein for zinc (Brown et al, 2004). Our observed zinc-HCC association was attenuated by statistical adjustment for hepatitis status, liver function markers, and albumin levels, particularly at the top tertile. This suggests that liver dysfunction and hepatitis infection may have a confounding or mediating effect on zinc-HCC risk association. For this reason, the potential of reverse causality in our observations cannot be completely ruled out, despite the prospective nature of our study and our lag analyses suggesting consistent associations. However, it is well established that zinc has numerous important physiologic and metabolic roles. Its functions in antioxidant pathways are central to its purported cancer protective effects (Osredkar, 2011). In addition, clinical studies of zinc supplementation indicate that it also acts to improve gut barrier function, decrease pro-inflammatory cytokine production and improve liver function in patients with liver diseases (Mohammad et al, 2012). This implies that maintenance of adequate zinc levels may be an important factor to support hepatocytes from cancer development in patients with underlying liver disease, but this needs to be confirmed in further studies.
In our study, copper was not directly associated with HCC development, but its level in relation to zinc (i.e. a higher Cu/Zn ratio) was strongly associated with increased HCC risk. This observation is likely to be derived more from the influence of zinc in calculation of the ratio. Nevertheless, copper itself has important metabolic roles whose impairment is relevant to cancer development. For example, excess copper may be pro-oxidative and pro-inflammatory (Bo et al, 2008), particularly in the liver where it is stored (Perlemuter et al, 2005). Data from animal studies show that copper excess, imbalanced by lower zinc level, increases lipid peroxidation and depletes GSH reserves (Ozcelik et al, 2003) suggesting a pro-oxidative effect. Interestingly, in the present study circulating copper was significantly increased in those with higher hsCRP levels, a marker of chronic inflammation, suggesting that higher serum copper is linked to inflammatory processes. Such processes may in turn activate production of ceruloplasmin, the copper carrier protein (Deshmukh et al, 1985), thus increasing its availability to bind copper within hepatocytes to release it to circulation. Liver disease progression and concomitant hepatocyte destruction can also cause the release of copper from the liver into the circulation by the damaged cells (Osredkar, 2011). However, as copper was not associated with HCC in our prospective study, it seems unlikely that this mechanism is an early event in liver tumorigenesis.
It is well recognised that copper to zinc ratio has a significant role in oxidative stress (Osredkar, 2011). The ratio has been previously studied as a measure of susceptibility or progression for a range of neurological, developmental and metabolic disorders, including diabetes and cardiovascular disease (Osredkar, 2011). The Cu/Zn ratio has been observed to be elevated in patients with hepatitis, liver cirrhosis or HCC, and appears to be correlated with the severity of liver disease (Nakayama et al, 2002; Lin et al, 2006). The role of Cu/Zn-SOD, whose functions are dependent on the adequate presence of both copper and zinc, is to catalyse ROS degradation originating from metabolic pathways to less reactive compounds, which are then removed by other antioxidant enzymes such as GSH peroxidase, thus reducing oxidative stress (Johnson and Giulivi, 2005). Maintenance of adequate copper to zinc status is important for supporting anti-oxidative functions of Cu/Zn-SOD and protection from damage.
The gall bladder, bile ducts and biliary tract are anatomically related to liver and liver metabolism. Excess body copper and zinc, are excreted with bile (Iakovidis et al, 2011; Osredkar, 2011), potentially exposing the biliary system to these microelements. However, copper and zinc status is highly regulated and excess levels are not common (Osredkar, 2011), suggesting low exposure of GBTC in the population studied. Although there is some existing evidence that gall bladder cancer patients have decreased serum zinc, increased copper and increased Cu/Zn ratio compared with healthy controls (Shukla et al, 2003; Gupta et al, 2005) our observations did not show any associations with development of GBTC or IHBD tumours. This may be indicative of no aetiological role for these micronutrients, but it may also be a consequence of our low sample size for these rarer tumours. In our previous study a pro-inflammatory cytokine, interleukin 6 that was linked to hypozincemia in a mouse model (Liuzzi et al, 2005), was also positively associated with HCC, but not other hepatobiliary cancers risk (Aleksandrova et al, 2014).
Despite being the second most common cause of death worldwide, indicating the need of more research to better understand its aetiology, liver cancer is relatively uncommon in more developed world regions with age-standardised rates of <10 per 100 000, compared with >20 in East and South-East Asia (Globocan, 2012). For this reason the main limitation of this study conducted on European populations was a relatively small sample size, especially with regard to the less prevalent type of liver cancer, IHBC. We also have no information on evolution of the biomarkers or lifestyle/dietary changes during the follow-up. Oxidative stress has been linked to initiation and progression of cancers (Hjelmeland and Zhang, 2016). Whether oxidative stress-related malignant changes are a consequence or a cause of underlying liver diseases, and specifically of HCC, still needs to be clearly established. Another limitation of the study is that we have measurements of total zinc and copper and cannot differentiate between bound and free forms; both free circulating zinc and copper represent the biologically active forms (Walshe, 2003; Twomey et al, 2005; Maret, 2013). Also, serum zinc and copper are only short-term biomarkers of status. However, given lack of gold standard to measure zinc and copper status, their serum levels are considered useful biomarkers (de Benoist et al, 2007; Harvey et al, 2009). Importantly, potential residual confounding with smoking and alcohol consumption cannot be discounted, nor can the possibility of reverse causality given the long term nature of HCC development and role of the liver in metabolism of these micronutrients. The strengths of our study include its prospective design, being conducted in separate labs with personnel blinded to the clinical identity of the samples and possibility to study early differences in biomarker status years before cancer diagnosis. In addition, availability of additional measures and information on liver-cancer associated disorders (diabetes, hepatitis B and C infection), indices of liver function (liver function tests, Fischer’s ratio) and inflammation status (hsCRP), and detailed information on relevant lifestyle factors, including body size, alcohol intake and smoking, allowed us to explore multiple factors in relation to biomarker levels, although this information was not available for all case-sets.
In conclusion, this study indicates an inverse association between pre-diagnostic zinc but not copper levels and HCC risk. Copper imbalance in relation to zinc concentration was in turn positively associated with HCC risk. If these results are confirmed in other prospective cohort studies and different population groups, they would suggest that maintenance of adequate circulating levels of zinc and copper may have an important role in preventing development of liver cancer.
Data availability
For information on how to submit an application for gaining access to EPIC data and/or bio-specimens, please follow the instructions at http://epic.iarc.fr/access/index.php.
Change history
28 February 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aigner E, Weiss G, Datz C (2015) Dysregulation of iron and copper homeostasis in nonalcoholic fatty liver. World J Hepatol 7 (2): 177–188.
Aleksandrova K, Boeing H, Nothlings U, Jenab M, Fedirko V, Kaaks R, Lukanova A, Trichopoulou A, Trichopoulos D, Boffetta P, Trepo E, Westhpal S, Duarte-Salles T, Stepien M, Overvad K, Tjonneland A, Halkjaer J, Boutron-Ruault MC, Dossus L, Racine A, Lagiou P, Bamia C, Benetou V, Agnoli C, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita B, Peeters PH, Gram IT, Lund E, Weiderpass E, Quiros JR, Agudo A, Sanchez MJ, Gavrila D, Barricarte A, Dorronsoro M, Ohlsson B, Lindkvist B, Johansson A, Sund M, Khaw KT, Wareham N, Travis RC, Riboli E, Pischon T (2014) Inflammatory and metabolic biomarkers and risk of liver and biliary tract cancer. Hepatology 60 (3): 858–871.
Augustine MM, Fong Y (2014) Epidemiology and risk factors of biliary tract and primary liver tumors. Surg Oncol Clin N Am 23 (2): 171–188.
Bishayee A (2014) The role of inflammation and liver cancer. Adv Exp Med Biol 816: 401–435.
Bo S, Durazzo M, Gambino R, Berutti C, Milanesio N, Caropreso A, Gentile L, Cassader M, Cavallo-Perin P, Pagano G (2008) Associations of dietary and serum copper with inflammation, oxidative stress, and metabolic variables in adults. J Nutr 138 (2): 305–310.
Brown KH, Rivera JA, Bhutta Z, Gibson RS, King JC, Lonnerdal B, Ruel MT, Sandtrom B, Wasantwisut E, Hotz C (2004) International Zinc Nutrition Consultative Group (IZiNCG) technical document #1. Assessment of the risk of zinc deficiency in populations and options for its control. Food Nutr Bull 25 (1 Suppl 2): S99–S203.
Costello LC, Franklin RB (2014) The status of zinc in the development of hepatocellular cancer: an important, but neglected, clinically established relationship. Cancer Biol Ther 15 (4): 353–360.
de Benoist B, Darnton-Hill I, Davidsson L, Fontaine O, Hotz C (2007) Conclusions of the joint WHO/UNICEF/IAEA/IZiNCG interagency meeting on zinc status indicators. Food Nutr Bull 28 (3 Suppl): S480–S484.
Deshmukh VK, Raman PH, Dhuley JN, Naik SR (1985) Role of ceruloplasmin in inflammation: increased serum ceruloplasmin levels during inflammatory conditions and its possible relationship with anti-inflammatory agents. Pharmacol Res Commun 17 (7): 633–642.
Diez M, Cerdan FJ, Arroyo M, Balibrea JL (1989) Use of the copper/zinc ratio in the diagnosis of lung cancer. Cancer 63 (4): 726–730.
Franklin RB, Costello LC (2009) The important role of the apoptotic effects of zinc in the development of cancers. J Cell Biochem 106 (5): 750–757.
Globocan (2012) Estimated Age-Standardised Incidence and Mortality Rates: Both Sexeshttp://globocan.iarc.fr/Pages/fact_sheets_population.aspx (accessed on 1 July 2015).
Gomaa AI, Khan SA, Toledano MB, Waked I, Taylor-Robinson SD (2008) Hepatocellular carcinoma: epidemiology, risk factors and pathogenesis. World J Gastroenterol 14 (27): 4300–4308.
Guo CH, Chen PC, Ko WS (2013) Status of essential trace minerals and oxidative stress in viral hepatitis C patients with nonalcoholic fatty liver disease. Int J Med Sci 10 (6): 730–737.
Gupta SK, Singh SP, Shukla VK (2005) Copper, zinc, and Cu/Zn ratio in carcinoma of the gallbladder. J Surg Oncol 91 (3): 204–208.
Harvey LJ, Ashton K, Hooper L, Casgrain A, Fairweather-Tait SJ (2009) Methods of assessment of copper status in humans: a systematic review. Am J Clin Nutr 89 (6): 2009S–2024S.
Hashemian M, Poustchi H, Abnet CC, Boffetta P, Dawsey SM, Brennan PJ, Pharoah P, Etemadi A, Kamangar F, Sharafkhah M, Hekmatdoost A, Malekzadeh R (2015) Dietary intake of minerals and risk of esophageal squamous cell carcinoma: results from the Golestan Cohort Study. Am J Clin Nutr 102 (1): 102–108.
Hjelmeland A, Zhang J (2016) Metabolic, autophagic, and mitophagic activities in cancer initiation and progression. Biomed J 39 (2): 98–106.
Hotz C, Peerson JM, Brown KH (2003) Suggested lower cutoffs of serum zinc concentrations for assessing zinc status: reanalysis of the second National Health and Nutrition Examination Survey data (1976–1980). Am J Clin Nutr 78 (4): 756–764.
Hughes DJ, Duarte-Salles T, Hybsier S, Trichopoulou A, Stepien M, Aleksandrova K, Overvad K, Tjonneland A, Olsen A, Affret A, Fagherazzi G, Boutron-Ruault MC, Katzke V, Kaaks R, Boeing H, Bamia C, Lagiou P, Peppa E, Palli D, Krogh V, Panico S, Tumino R, Sacerdote C, Bueno-de-Mesquita HB, Peeters PH, Engeset D, Weiderpass E, Lasheras C, Agudo A, Sanchez MJ, Navarro C, Ardanaz E, Dorronsoro M, Hemmingsson O, Wareham NJ, Khaw KT, Bradbury KE, Cross AJ, Gunter M, Riboli E, Romieu I, Schomburg L, Jenab M (2016) Prediagnostic selenium status and hepatobiliary cancer risk in the European Prospective Investigation into cancer and nutrition cohort. Am J Clin Nutr 104 (2): 406–414.
Hyun MS, Suh SK, Yoon NK, Lee JY, Lee SH, Lee MS (1992) Association of serum copper and zinc levels with liver cirrhosis and hepatocellular carcinoma. Korean J Prev Med 25 (2): 127–140.
Iakovidis I, Delimaris I, Piperakis SM (2011) Copper and its complexes in medicine: a biochemical approach. Mol Biol Int 2011: 594529.
Ishikawa T (2012) Branched-chain amino acids to tyrosine ratio value as a potential prognostic factor for hepatocellular carcinoma. World J Gastroenterol 18 (17): 2005–2008.
Johnson F, Giulivi C (2005) Superoxide dismutases and their impact upon human health. Mol Aspects Med 26 (4-5): 340–352.
Ko WS, Guo CH, Yeh MS, Lin LY, Hsu GS, Chen PC, Luo MC, Lin CY (2005) Blood micronutrient, oxidative stress, and viral load in patients with chronic hepatitis C. World J Gastroenterol 11 (30): 4697–4702.
Leone N, Courbon D, Ducimetiere P, Zureik M (2006) Zinc, copper, and magnesium and risks for all-cause, cancer, and cardiovascular mortality. Epidemiology 17 (3): 308–314.
Lightman A, Brandes JM, Binur N, Drugan A, Zinder O (1986) Use of the serum copper/zinc ratio in the differential diagnosis of ovarian malignancy. Clin Chem 32 (1 Pt 1): 101–103.
Lin CC, Huang JF, Tsai LY, Huang YL (2006) Selenium, iron, copper, and zinc levels and copper-to-zinc ratios in serum of patients at different stages of viral hepatic diseases. Biol Trace Elem Res 109 (1): 15–24.
Liuzzi JP, Lichten LA, Rivera S, Blanchard RK, Aydemir TB, Knutson MD, Ganz T, Cousins RJ (2005) Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Proc Natl Acad Sci USA 102 (19): 6843–6848.
Ma J, Betts NM (2000) Zinc and copper intakes and their major food sources for older adults in the 1994–96 continuing survey of food intakes by individuals (CSFII). J Nutr 130 (11): 2838–2843.
Mao S, Huang S (2013) Zinc and copper levels in bladder cancer: a systematic review and meta-analysis. Biol Trace Elem Res 153 (1-3): 5–10.
Ma X, Yang Y, Li HL, Zheng W, Gao J, Zhang W, Yang G, Shu XO, Xiang YB (2017) Dietary trace element intake and liver cancer risk: results from two population-based cohorts in China. Int J Cancer 140 (5): 1050–1059.
Maret W (2013) Zinc biochemistry: from a single zinc enzyme to a key element of life. Adv Nutr 4 (1): 82–91.
Mohammad MK, Zhou Z, Cave M, Barve A, McClain CJ (2012) Zinc and liver disease. Nutr Clin Pract 27 (1): 8–20.
Nakayama A, Fukuda H, Ebara M, Hamasaki H, Nakajima K, Sakurai H (2002) A new diagnostic method for chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma based on serum metallothionein, copper, and zinc levels. Biol Pharm Bull 25 (4): 426–431.
Nangliya V, Sharma A, Yadav D, Sunder S, Nijhawan S, Mishra S (2015) Study of trace elements in liver cirrhosis patients and their role in prognosis of disease. Biol Trace Elem Res 165 (1): 35–40.
Osredkar JSN (2011) Copper and Zinc, Biological Role and Significance of Copper/Zinc Imbalance. J Clin Toxicol S3: 001.
Ozcelik D, Ozaras R, Gurel Z, Uzun H, Aydin S (2003) Copper-mediated oxidative stress in rat liver. Biol Trace Elem Res 96 (1-3): 209–215.
Page AJ, Cosgrove DC, Philosophe B, Pawlik TM (2014) Hepatocellular carcinoma: diagnosis, management, and prognosis. Surg Oncol Clin N Am 23 (2): 289–311.
Perlemuter G, Davit-Spraul A, Cosson C, Conti M, Bigorgne A, Paradis V, Corre MP, Prat L, Kuoch V, Basdevant A, Pelletier G, Oppert JM, Buffet C (2005) Increase in liver antioxidant enzyme activities in non-alcoholic fatty liver disease. Liver Int 25 (5): 946–953.
Piciocchi M, Cardin R, Cillo U, Vitale A, Cappon A, Mescoli C, Guido M, Rugge M, Burra P, Floreani A, Farinati F (2016) Differential timing of oxidative DNA damage and telomere shortening in hepatitis C and B virus-related liver carcinogenesis. Transl Res 168: 122–133.
Poo JL, Rosas-Romero R, Montemayor AC, Isoard F, Uribe M (2003) Diagnostic value of the copper/zinc ratio in hepatocellular carcinoma: a case control study. J Gastroenterol 38 (1): 45–51.
Rahelic D, Kujundzic M, Romic Z, Brkic K, Petrovecki M (2006) Serum concentration of zinc, copper, manganese and magnesium in patients with liver cirrhosis. Coll Antropol 30 (3): 523–528.
Riboli E, Kaaks R (1997) The EPIC Project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol 26 (Suppl 1): S6–S14.
Satapati S, Kucejova B, Duarte JA, Fletcher JA, Reynolds L, Sunny NE, He T, Nair LA, Livingston K, Fu X, Merritt ME, Sherry AD, Malloy CR, Shelton JM, Lambert J, Parks EJ, Corbin I, Magnuson MA, Browning JD, Burgess SC (2015) Mitochondrial metabolism mediates oxidative stress and inflammation in fatty liver. J Clin Invest 125 (12): 4447–4462.
Sawa AOK (1990) The Role of Copper and Zinc as Pathogenic Factors in Liver Disease. Springer: Japan.
Shukla VK, Adukia TK, Singh SP, Mishra CP, Mishra RN (2003) Micronutrients, antioxidants, and carcinoma of the gallbladder. J Surg Oncol 84 (1): 31–35.
Stepien M, Duarte-Salles T, Fedirko V, Floegel A, Barupal DK, Rinaldi S, Achaintre D, Assi N, Tjonneland A, Overvad K, Bastide N, Boutron-Ruault MC, Severi G, Kuhn T, Kaaks R, Aleksandrova K, Boeing H, Trichopoulou A, Bamia C, Lagiou P, Saieva C, Agnoli C, Panico S, Tumino R, Naccarati A, Bueno-de-Mesquita HB, Peeters PH, Weiderpass E, Quiros JR, Agudo A, Sanchez MJ, Dorronsoro M, Gavrila D, Barricarte A, Ohlsson B, Sjoberg K, Werner M, Sund M, Wareham N, Khaw KT, Travis RC, Schmidt JA, Gunter M, Cross A, Vineis P, Romieu I, Scalbert A, Jenab M (2016a) Alteration of amino acid and biogenic amine metabolism in hepatobiliary cancers: Findings from a prospective cohort study. Int J Cancer 138 (2): 348–360.
Stepien M, Fedirko V, Duarte-Salles T, Ferrari P, Freisling H, Trepo E, Trichopoulou A, Bamia C, Weiderpass E, Olsen A, Tjonneland A, Overvad K, Boutron-Ruault MC, Fagherazzi G, Racine A, Kuhn T, Kaaks R, Aleksandrova K, Boeing H, Lagiou P, Benetou V, Trichopoulos D, Palli D, Grioni S, Tumino R, Naccarati A, Panico S, Bueno-de-Mesquita HB, Peeters PH, Lund E, Quiros JR, Napoles OC, Sanchez MJ, Dorronsoro M, Huerta JM, Ardanaz E, Ohlsson B, Sjoberg K, Werner M, Nystrom H, Khaw KT, Key TJ, Gunter M, Cross A, Riboli E, Romieu I, Jenab M (2016b) Prospective association of liver function biomarkers with development of hepatobiliary cancers. Cancer Epidemiol 40: 179–187.
Theophanides T, Anastassopoulou J (2002) Copper and carcinogenesis. Crit Rev Oncol/Hematol 42 (1): 57–64.
Trichopoulos D, Bamia C, Lagiou P, Fedirko V, Trepo E, Jenab M, Pischon T, Nothlings U, Overved K, Tjonneland A, Outzen M, Clavel-Chapelon F, Kaaks R, Lukanova A, Boeing H, Aleksandrova K, Benetou V, Zylis D, Palli D, Pala V, Panico S, Tumino R, Sacerdote C, Bueno-De-Mesquita HB, Van Kranen HJ, Peeters PH, Lund E, Quiros JR, Gonzalez CA, Sanchez Perez MJ, Navarro C, Dorronsoro M, Barricarte A, Lindkvist B, Regner S, Werner M, Hallmans G, Khaw KT, Wareham N, Key T, Romieu I, Chuang SC, Murphy N, Boffetta P, Trichopoulou A, Riboli E (2011) Hepatocellular carcinoma risk factors and disease burden in a European cohort: a nested case–control study. J Natl Cancer Inst 103 (22): 1686–1695.
Twomey PJ, Viljoen A, House IM, Reynolds TM, Wierzbicki AS (2005) Relationship between serum copper, ceruloplasmin, and non-ceruloplasmin-bound copper in routine clinical practice. Clin Chem 51 (8): 1558–1559.
Walshe JM (2003) Wilson’s disease: the importance of measuring serum caeruloplasmin non-immunologically. Ann Clin Biochem 40 (Pt 2): 115–121.
Wu T, Sempos CT, Freudenheim JL, Muti P, Smit E (2004) Serum iron, copper and zinc concentrations and risk of cancer mortality in US adults. Ann Epidemiol 14 (3): 195–201.
Acknowledgements
This work was supported by the French National Cancer Institute (L’Institut National du Cancer; INCA; grant number 2009-139; PI: M Jenab) and the Health Research Board of Ireland (award number HRA_PHS/2013/397; PI: DJ Hughes). The coordination of EPIC is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by Danish Cancer Society (Denmark); Ligue Contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (INSERM) (France); Deutsche Krebshilfe, Deutsches Krebsforschungszentrum and Federal Ministry of Education and Research (Germany); the Hellenic Health Foundation (Greece); Associazione Italiana per la Ricerca sul Cancro-AIRC-Italy and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (The Netherlands); Nordic Centre of Excellence programme on Food, Nutrition and Health. (Norway); Health Research Fund (FIS), PI13/00061 to Granada), Regional Governments of Andalucía, Asturias, Basque Country, Murcia (No. 6236) and Navarra, ISCIII RETIC (RD06/0020) (Spain); Swedish Cancer Society, Swedish Scientific Council and County Councils of Skåne and Västerbotten (Sweden); Cancer Research UK (14136 to EPIC-Norfolk; C570/A16491 and C8221/A19170 to EPIC-Oxford), Medical Research Council (1000143 to EPIC-Norfolk and MR/M012190/1 to EPIC-Oxford) (UK); Medical Research Council (1000143 to EPIC-Norfolk) (UK). For information on how to submit an application for gaining access to EPIC data and/or bio-specimens, please follow the instructions at http://epic.iarc.fr/access/index.php.
Disclaimer
None of the funding sources had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript, and decision to submit the manuscript for publication.
Author contributions
All named authors have read the manuscript, have agreed to the submission and have participated
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Stepien, M., Hughes, D., Hybsier, S. et al. Circulating copper and zinc levels and risk of hepatobiliary cancers in Europeans. Br J Cancer 116, 688–696 (2017). https://doi.org/10.1038/bjc.2017.1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.1
Keywords
This article is cited by
-
Cellular zinc metabolism and zinc signaling: from biological functions to diseases and therapeutic targets
Signal Transduction and Targeted Therapy (2024)
-
Circulating Copper and Liver Cancer
Biological Trace Element Research (2023)
-
Determination of potential sources of heavy metals in patients with urothelial carcinoma in central Taiwan: a biomonitoring case–control study
Environmental Geochemistry and Health (2023)
-
Copper in Cancer: from transition metal to potential target
Human Cell (2023)
-
Associations of Iron Intake, Serum Iron and Serum Ferritin with Bone Mineral Density in Women: The National Health and Nutrition Examination Survey, 2005–2010
Calcified Tissue International (2020)