Abstract
Background:
Insulin/insulin-like growth factor-1 signalling may underlie the promoting effect of type 2 diabetes on cancer. This study examined the association of diabetes, including steroid-induced diabetes (SID), and the impact of anti-diabetic medication on clinical outcomes of multiple myeloma (MM).
Methods:
A retrospective review was conducted of 1240 MM patients. Overall survival (OS) and MM disease status prior to death were analysed.
Results:
Diabetic patients had a significantly shorter OS than non-diabetic patients (median: 65.4 vs 98.7 months). In multivariate analysis, SID was a significant predictor of decreased OS, along with age, comorbidity, MM stage, and cytogenetic abnormalities. Analyzing only the diabetic MM patients, Cox regression showed that metformin predicted an increased OS, whereas use of insulin/analogues predicted a decreased OS. Competing risk analysis showed that DM was associated with increased cumulative incidence of death with progressive MM. Among the diabetics, multivariate regression showed that insulin/analogues were associated with increased, but metformin with decreased death with progressive MM. Potential immortal time bias was evaluated by landmark analyses.
Conclusions:
DM, SID in particular, is associated with poor clinical outcomes in MM. Insulin/analogues are associated with poor outcomes, whereas metformin is associated with improved outcomes. No conclusion about causal relationships can be made at this time. Managing hyperglycaemia with non-insulin regimens should be investigated in randomised trials.
Similar content being viewed by others
Main
Extensive epidemiologic data suggest important roles of type 2 diabetes mellitus in carcinogenesis (Nilsen and Vatten, 2001; Verlato et al, 2003; Coughlin et al, 2004; Richardson and Pollack, 2005). The current consensus is that type 2 diabetes may influence the neoplastic process through hyperglycaemia, hyperinsulinemia, and chronic inflammation (Giovannucci et al, 2010). The important roles of interleukin 6–Janus kinase–signal transducer and activator of transcription 3 and insulin receptor (IR)/insulin-like growth factor-1 receptor (IGF-1R)–insulin receptor substrate 1 signalling pathways in multiple myeloma (MM) have been well established (Gado et al, 2001; Bommert et al, 2006; Cozen et al, 2006; Menu et al, 2009; Mahindra et al, 2010; Benetatos and Vartholomatos, 2012). These signalling pathways are also activated by insulin and insulin-like growth factors in obesity and insulin-resistant conditions, including type 2 diabetes mellitus (Reseland et al, 2009). Although obesity (Wallin and Larsson, 2011; Hofmann et al, 2013) and diabetes (Boffetta et al, 1989; Fortuny et al, 2005) are associated with an increased MM incidence, the impact of diabetes on the clinical outcome of MM after diagnosis (i.e., prognosis) has only been investigated in a Taiwanese study (Chou et al, 2012), which found that pre-existing diabetes was associated with advanced stage and poor overall survival (OS). The potential impacts of steroid-induced diabetes (SID) and anti-diabetic medications on MM have not been reviewed in clinical cohorts.
Recent evidence has also shown that different anti-diabetic agents affect cancer cells in different ways. In vitro studies have shown that insulin and glucose promote cancer cell proliferation and can contribute to chemoresistance, whereas metformin and rosiglitazone suppress cancer cell growth and induce apoptosis (Feng et al, 2011; Pan et al, 2012). Our previous retrospective studies revealed that metformin was associated with an improved prognosis of prostate cancer (He et al, 2011), pancreatic cancer (Sadeghi et al, 2012), and HER2+ breast cancer (Huang et al, 2011), and so were thiazolidinediones for prostate cancer (He et al, 2011) and HER2+ breast cancer (Huang et al, 2011).
Hyperglycaemia in acute lymphoblastic leukaemia patients during induction chemotherapy (which includes high-dose glucocorticoids) was associated with poor prognosis (Weiser et al, 2004). Despite improved glycemic control, intensive insulin analogue management did not improve prognosis (Vu et al, 2012). This prospective randomised trial was closed at a scheduled interim analysis because the intensive insulin group trended towards having a worse OS than the control group. Secondary analysis suggested that high levels of exogenous insulin were associated with poor prognosis; in contrast, use of metformin and/or thiazolidinediones was associated with improved prognosis (Vu et al, 2012). As high-dose glucocorticoids are also used to treat MM, SID, and exacerbation of type 2 diabetes and their impact on prognosis are important clinical issues. We hypothesised that diabetes was associated with poor clinical outcomes of MM, and that the choice of anti-diabetic pharmacotherapy can influence the clinical outcome of the malignancy. Therefore, we performed a retrospective study to evaluate the hypotheses.
Materials and methods
Study population
This retrospective study was approved by The University of Texas MD Anderson Cancer Center (MDACC) Institutional Review Board in accordance with an assurance filed with, and approved by the Department of Health and Human Services. Using the Tumor Registry database, 1240 consecutive patients with newly diagnosed MM treated at MDACC from 1 January 1996 to 31 December 2010 were identified. The following exclusion criteria were applied to these 1240 patients: (i) type 1 diabetes mellitus, (ii) cancer diagnosis made more than 6 months prior to presentation to MDACC, (iii) incomplete medical records, and (iv) MDACC not being the primary institution of oncologic care. The final study cohort consisted of 1083 patients.
Data collection
Trained research personnel reviewed records to collect information on demographics and known or suspected risk factors for MM prognosis (i.e., age, stage, cytogenetic abnormalities, stem cell transplantation, obesity, and other comorbidities). Staging was based on the International Staging System (ISS) for MM. Bone marrow transplant status was based on both the medical records and the database maintained by the Stem Cell Transplantation Department. Based on the pathology reports, cytogenetic abnormalities were recorded. The presence of translocations involving chromosome 14 (t(11;14), t(4;14), t(14;16) and t(14;20)], which would include the majority of the patients with cytogenetic abnormalities in this cohort, was coded as a categorical variable. Body mass index (BMI; kg m−2) was calculated using the recorded height and body weight at the first MDACC visit and was categorised as follows: non-obese (BMI <30 kg m−2) and obese (BMI⩾30 kg m−2). Clinical data of each patient were reviewed to assess the Charlson Comorbidity Index (CCI) (Charlson et al, 1987). The primary clinical outcome was OS. Survival information was obtained through MDACC’s Tumor Registry. Methods of follow-up for the Tumor Registry include letters and phone calls, computer matches with the business office for kept appointments, searches of public databases (the Social Security Death Index, Bureau of Vital Statistics of Texas and neighboring states), and MDACC clinic staff notifications. If a patient was not known to be dead, survival time was censored at the last follow-up. OS was defined as the duration between cancer diagnosis and death or last contact. Treatment response was assessed by the oncologists based on the criteria of the International Myeloma Working Group (Durie et al, 2006). The MM disease status at the last clinical documentation was ascertained and categorised as progressive disease or without progressive disease. Death with progressive MM and death without progressive myeloma were analysed as competing events.
An MM patient was classified as having a history of diabetes (HxD) if there was a medical history of type 2 diabetes or the patient was on routine anti-diabetic medications at the time of diagnosis of MM and presentation to MDACC. Plasma glucose was routinely measured approximately weekly during induction therapy. A patient was classified as having SID if there was no HxD before diagnosis of MM and they had ⩾2 random plasma glucose>200 mg d−1, or received anti-diabetic medications after initiation of glucocorticoid therapy for MM treatment. MM patients that were not classified in the HxD and SID groups were classified as having no diabetes (ND).
The MDACC Clinical Laboratory database was searched to obtain all plasma glucose values of each study participant. The mean and maximum glucose levels were used to evaluate the degree of hyperglycaemia. Mean of all glucose values is expected to be disproportionately higher for the more severe diabetic patients, as they would have had more tests. This mean is included in the multivariate analysis as a discriminant of adequacy of glycemic control. The patients with poor glycemic control will have an increased value, separating them from those with good glycemic control.
The MDACC Pharmacy database, including all outpatient and inpatient dispensing records, was searched for glucocorticoids and anti-diabetic medications of all the study participants. Anti-diabetic pharmacotherapy was classified as (i) insulin or insulin analogues, (ii) insulin secretagogues (e.g., sulfonylureas and meglitinides), (iii) biguanides, (iv) thiazolidinediones, and (v) others (including α-glucosidase inhibitors, dipeptidyl peptidase-4 inhibitors, amylin analogues and glucagon-like peptide 1 analogues). Because many patients used combination therapy, the drugs or combinations might have changed over time, and the number of patients in each monotherapy group was small, we represented the anti-diabetic pharmacotherapy of each patient with five categorical attributes of user vs non-user of (i) insulin formulations or insulin analogues, (ii) insulin secretagogues, (iii) metformin, (iv) thiazolidinediones, (v) others. These attributes were classified according to medication use at the time of presentation and subsequent medication records at our institution. ‘Users’ of a class of drug meant that the patients used that class at presentation, or subsequently changed to or added a member of that class of drug regardless of dosage or duration of usage. These categorical variables were used in regression models to examine the association with specific types of anti-diabetic pharmacotherapy.
Statistical analysis
Baseline patient characteristics and clinical risk factors of MM prognosis were compared between groups by the χ2-test, Fisher’s exact test, Student’s t-test or Mann-Whitney rank sum test where appropriate. Univariate analysis of OS was performed using the Kaplan–Meier method with the log-rank test unless otherwise indicated. Multivariate regression analyses of survival data were based on the Cox proportional hazards modelling. Immortal time bias was examined by the landmark analysis (Giobbie-Hurder et al, 2013). Competing risk analysis based on the Fine and Gray model was carried out using the functions cuminc and crr in the R statistical package (R version 2.13.0, The R Foundation for Statistical Computing). All other statistical analyses were carried out using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA), S-Plus version 8.04 (TIBCO, Somerville, MA, USA), and SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). A P-value <0.05 was considered statistically significant.
Results
Patient demographics and clinical characteristics
The cohort consisted of 1083 MM patients whose median age at diagnosis of MM was 57 years (range: 23–91 years). The median follow-up was 52.73 months (range: 1.25–207.25 months). The patients were categorised as having ND, HxD, or SID. Demographics and clinical characteristics are summarised in Table 1. In this cohort, 12.6% had HxD and 31.7% had SID. The proportion of non-white minorities in the HxD group is higher (P<0.001) than the other groups. The age, BMI, and CCI at MM diagnosis of the HxD group were significantly higher than ND and SID. The proportion of obese patients in HxD was higher than the other two groups. The proportion of patients with CCI >5 in HxD was higher than the other two groups, and a lower proportion in HxD underwent stem cell transplantation than ND and SID. The maximum of glucose level was significantly lower (P<0.05, ANOVA on ranks, post hoc intergroup comparisons with Dunn’s method) in the ND group than the HxD and SID groups. The average glucose level of each patient was significantly different in all intergroup comparisons (P<0.05, ANOVA on ranks; medians: ND, 101.1 mg dl−1; SID, 116.3 mg dl−1; HxD, 135.2 mg dl−1).
Association of type 2 diabetes and SID with lower rates of complete remission than non-diabetic MM patients
The status of complete remission was based on the assessment made by the treating oncologist based on established criteria (Durie et al, 2006) with corroboration by pathology results. The rate of complete remission after induction therapy was 21.2% (29/136) in HxD and 20.4% (70/344) in SID, which were significantly (P=0.003) different from 28.7% (173/603) in ND. Binary logistic regression showed that diabetes (HxD or SID) was significantly associated with a decreased probability of complete remission (P=0.008, odds ratio=0.672, 95% CI: 0.901–0.501), whereas stem cell transplantation was significantly associated with increased probability of complete remission (P<0.001, odds ratio=4.324, 95% CI: 2.475–7.575). Age >65 years at diagnosis, the presence of translocations to chromosome 14, and CCI >5 were not significant predictors in the same regression model (P=0.615, 0.059 and 0.156, respectively). Therefore, the MM patients with diabetes (HxD or SID) have lower complete remission rates than ND.
Association of type 2 diabetes and SID with decreased OS of myeloma patients
Univariate Kaplan–Meier analyses of potential prognostic factors for OS are shown in Figure 1. The age of diagnosis >65 years (Figure 1A), CCI >5 (Figure 1E), ISS stage (Figure 1F), and the presence of cytogenetic abnormalities with translocation involving chromosome 14 (Figure 1G) were significant predictors of decreased OS. Race (non-white compared with white) (Figure 1B), gender (Figure 1C) ,and obesity (BMI⩾30 kg m−2 compared with <30 kg m−2) (Figure 1D) were not significant risk factors. Patients who underwent stem cell transplantation (Figure 1H) had significantly longer survival. Based on the records of all the glucose laboratory test results for each patient, a mean plasma glucose level ⩾120 mg dl−1 was associated with poor OS (Figure 1I), and so was a maximum plasma glucose level ⩾200 mg dl−1 (Figure 1J). Diabetic MM patients (HxD and SID groups combined) had significantly decreased survival (Figure 1K, median OS: 65.4 vs 98.7 months). Steroid-induced diabetes was a significant predictor of poor OS (P<0.001, median OS=62.8 months), whereas HxD was not (P=0.0593, median OS=69.8 months) when compared with ND (median OS=98.7 months) (Figure 1L). Using the date of the first anti-diabetic medication recorded in our pharmacy database or the date of the first plasma glucose >200 mg dl−1, the time from diagnosis of MM to the discovery of SID was calculated to estimate the latency of SID assuming that MM treatment involving glucocorticoid would be started within 1 month of MM diagnosis. The cumulative incidence of SID was plotted against the time after MM diagnosis in Supplementary Figure 1A. The median time from diagnosis of MM to discovery of SID was 159 days. For those patients treated with metformin, the median time from diagnosis of MM to the pharmacy record of metformin was 175 days. As the induction chemotherapy for MM typically lasts for 6 months or more after MM diagnosis, we sub-divided the SID group into those identified as <6 months and those identified as ⩾6 months after MM diagnosis. A univariate Kaplan–Meier analysis demonstrated that patients with SID identified as <6 months after MM diagnosis survived shorter (median OS: 45.5 vs 59.9 months) than those with SID identified later (Supplementary Figure 1B; P=0.008, Gehan–Breslow test). Therefore, hyperglycaemia and diabetes (particularly SID diagnosed <6 months after myeloma diagnosis) were associated with shorter OS, along with age at diagnosis >65 years, CCI >5, ISS stage, and the presence of translocations to chromosome 14. Undergoing stem cell transplantation was a very important prognostic factor associated with greater OS.
Univariate Kaplan–Meier analyses of prognostic factors for myeloma patients. Kaplan–Meier curves of overall survival are shown for age of diagnosis (A), race (B), sex (C), obesity (D), Charlson Comorbidity Score (CCI) >5 (E), ISS Stage (F), chromosome 14 translocation (G), Stem cell transplant (H), Mean glucose values <120 mg dl−1 (I), maximum glucose values <200 mg dl−1 (J), diabetes status (HxD type 2 and SID groups combined) (K), and diabetes status as three groups (no diabetes, pre-existing diabetes, and SID) (L).
A Cox model for OS was constructed using the patient demographic categorical variables of age at diagnosis >65 years, white race, and male gender; the myeloma-related categorical variables of ISS stage, the presence of cytogenetic abnormalities involving translocation involving chromosome 14, and having undergone stem cell transplantation; the comorbidity categorical variable of CCI >5, and diabetes status (ND, HxD, or SID). The categorical variable of mean plasma glucose >120 mg dl−1 was included as an indicator of suboptimal glucose control over the long term. The multivariate Cox regression analysis of OS using this model is shown in Table 2. Having undergone stem cell transplantation was associated with improved OS. ISS stage, translocation involving chromosome 14, stem cell transplantation, CCI >5, and SID were associated with decreased OS. Therefore, while controlling for the effects of all the covariates in the model, SID was a significant independent predictor of poor OS of MM patients.
The FDA approval of thalidomide for myeloma therapy on 26 May 2006 is an event that marked the beginning of changes in myeloma therapy. Among the patients diagnosed before 26 May 2006, the prevalence of SID was 34.8% and HxD 10.5%. Among the MM patients diagnosed after 26 May 2006, the prevalence of SID was 27.1% and HxD 15.4%. Analyzing the MM patients diagnosed before and those diagnosed after 26 May 2006 separately showed that SID remained a significant predictor of poor OS in both groups (Supplementary Table 1).
Association of anti-diabetic pharmacotherapy with OS of diabetic myeloma patients
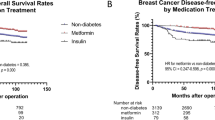
Among only the patients with diabetes (HxD or SID), univariate Kaplan–Meier analysis of maximum plasma glucose >200 mg dl−1 (Figure 2A) and mean plasma glucose >120 mg dl−1 (Figure 2B) did not show any significant association with OS. Anti-diabetic pharmacotherapy was classified as follows: (1) insulin or insulin analogues, (2) biguanides, (3) thiazolidinediones, (4) insulin secretagogues (e.g., sulfonylureas and meglitinides), (5) others (including α-glucosidase inhibitors, amylin analogues, DPP-4 inhibitors, and GLP-1 analogues). Usage of insulin and analogues had a significant (Figure 2C, P<0.001) decrease in OS (median=57.0 months) compared with no usage (median=101 months). In contrast, metformin usage (Figure 2E) was associated with a significantly (P=0.034) longer OS (median=74.3 months) compared with non-users (median=60.1 months). Usage of insulin secretagogues (Figure 2D), thiazolidinediones (Figure 2F), and other anti-diabetic medications (Figure 2G) were not significant predictors.
Univariate Kaplan–Meier analyses of glycemic control and anti-diabetic pharmacotherapies as prognostic factors for diabetic myeloma patients. The associations of anti-diabetic medications with overall survival were evaluated in diabetic myeloma patients (pre-existing and SID groups combined). Kaplan–Meier survival curves are shown for maximum glucose values <200 mg dl−1 (A), mean glucose values <120 mg dl−1 (B), insulin and analogues (C), insulin secretagogues (D), metformin (E), thiazolidinediones (F), other anti-diabetic drugs (G).
Five categorical variables (users vs non-users of (a) insulin formulations or insulin analogues, (b) insulin secretagogues, (c) metformin, (d) thiazolidinediones, and (e) other anti-diabetic medications) were used to examine the anti-diabetic medication usage pattern in MM patients with HxD and SID (Supplementary Table 2). There was no significant difference in the use of insulin and analogues, but all the other classes of anti-diabetic medications were less likely to be used in MM patients with SID than those with HxD. These five drug usage variables were included in a multivariate Cox Regression analysis that also included the categorical variables of ISS stage, translocation involving chromosome 14, CCI >5, and stem cell transplantation (Table 3). ISS stage and use of insulin or analogues were associated with decreased OS, whereas stem cell transplantation and use of metformin were associated with an increased OS. Specifically, usage of insulin and analogues was associated with a 1.8-fold increase in risk of death, whereas metformin usage was associated with a 0.66-fold decrease in risk of death (Table 3).
Not only is renal insufficiency one of the major complications of diabetes and of MM that impacts OS, but it is also a contraindication for the use of metformin. In our study cohort, there were 55 diabetic patients with chronic renal insufficiency (baseline serum creatinine <1.5 mg dl−1, excluding transient rises in creatinine during intercurrent illnesses), and none of them were prescribed metformin. Whether differences in the presence of chronic renal insufficiency between metformin users and non-users could account for the association of metformin use with improved OS was investigated by excluding patients with chronic renal insufficiency in the analysis. Among the diabetic patients without chronic renal insufficiency, the same multivariate Cox regression model of OS confirmed that metformin use remained a significant (P=0.039) predictor of improved survival (Supplementary Table 3). Therefore, chronic renal insufficiency could not completely account for the observed association of metformin use with improved OS.
To address the possible role of immortal time bias in the observed association of metformin, we performed landmark analyses at 3, 6, 9, and 12 months. Using the same Cox model as in Table 3, the P-values for the association of metformin remained significant at the 3-, 6-, 9- and 12-month landmarks (0.012, 0.022, 0.039, and 0.029, respectively) (Supplementary Table 4.1–4.4). Therefore, it was unlikely that the beneficial association of metformin use with OS was due to immortal time bias.
Association of diabetes with death in the presence of progressive myeloma
It was very difficult to determine cancer-specific death accurately based on death certificates, especially when the patients died outside a hospital or health care institution. Therefore, we used ‘death in the presence of progressive myeloma’ as a substitute because the overwhelming majority of these deaths would very probably attributable to myeloma. Death with progressive myeloma and death without progressive myeloma (i.e., no evidence of disease or stable disease) were competing events in our competing risk analysis. Plots of cumulative incidence estimate for death with progressive myeloma among patients grouped by diabetes status are presented in Figure 3A and B. When comparing the diabetic group (HxD and SID combined) with the ND group, there was a significant (P<0.001) increase in the cumulative incidence of death with progressive myeloma in diabetic patients (Figure 3A). When compared with ND with HxD and SID as separate groups, patients with SID had a significant (P<0.001) increase in mortality with progressive myeloma, and so did patients with HxD (P=0.034) (Figure 3B).
Univariate competing risk analyses of diabetes and anti-diabetic pharmacotherapies as prognostic factors for death in the presence of progressive myeloma. Based on Fine & Gray competing risk analysis, death with progressive myeloma and death without progressive myeloma were analysed as competing events. Cumulative incidence curves are shown as labelled for diabetic patients vs non-diabetic patients (A). Diabetes was associated with significantly (P<0.001) increased incidence of deaths with progressive myeloma (red vs black) but not deaths without progressive myeloma (blue vs green). Analyzing the diabetes status as three groups (no diabetes vs pre-existing diabetes vs SID), cumulative incidence curves and significant P-values are shown as labelled in (B). Analyzing only the diabetic patients, cumulative incidence curves of deaths with progressive myeloma comparing users (red line) and non-users (black line) and those of deaths without progressive myeloma comparing users (blue line) with non-users (green line) are shown for insulin/analogues (C), insulin secretagogues (D), metformin (E), thiazolidinediones (F), other anti-diabetic medications (G). Insulin and analogues usage was significantly (P=0.007) associated with death with progressive myeloma (C).
In the multivariate regression analysis of competing events, the covariates analysed were the same ones in Table 2. The result of this regression model (Supplementary Table 5.1) demonstrated that ISS stage and diabetes were associated with increased cumulative incidence of death with progressive myeloma (overall, P=0.037, HR=1.142, 95% CI: 1.008–1.295; and P<0.001, HR=1.346, 95% CI: 1.207–1.501, respectively), whereas stem cell transplantation was associated with decreased cumulative incidence of death with progressive myeloma (P=0.005, HR=0.647, 95% CI: 0.476–0.879). In contrast, diabetes was not associated with changes in cumulative incidence of death without progressive myeloma (Supplementary Table 5.2). High comorbidity (CCI >5) and poor glycemic control (mean plasma glucose level >120 mg dl−1) were associated with increased mortality without progressive myeloma, whereas stem cell transplantation was associated with decreased mortality. Therefore, diabetes, especially SID, was associated with increased mortality in the presence of progressive myeloma but not mortality in the absence of progressive myeloma.
Association of anti-diabetic pharmacotherapies with death in the presence of progressive myeloma
To investigate the impact of different classes of anti-diabetic pharmacotherapy, the diabetic myeloma patients (HxD and SID) were analysed by comparing users with non-users of various drug classes. There was a significant (P=0.007) increase in mortality with progressive myeloma in users of insulin and analogues compared with non-users (Figure 3C), and there was no significant difference in mortality without progressive myeloma. When comparing insulin secretagogue users vs non-users, metformin users vs non-users, thiazolidinedione users vs non-users, and users of other anti-diabetic drugs vs non-users, there were no significant differences in mortality with progressive myeloma (Figure 3D–G). These results suggested that SID was associated with increased cumulative incidence of mortality with progressive myeloma, and that insulin and analogues were associated with mortality with progressive myeloma in the diabetic myeloma patients.
In multivariate regression analysis of competing events, the covariates analysed included the pharmacological classes of anti-diabetic drugs. The result of this regression model (Supplementary Table 6.1) suggested that among the different pharmacological classes, insulin and analogues were associated with increased cumulative incidence of death with progressive myeloma (P=0.008, HR=1.562, 95% CI: 1.122–2.174), whereas metformin was associated with decreased cumulative incidence of death with progressive myeloma (P=0.037, HR=0.663, 95% CI: 0.452–0.975). In contrast, none of the drug classes were associated with changes in cumulative incidence of death without progressive myeloma (data not shown). The P-values for the association of metformin remained significant at the 3- and 6-month landmarks (0.041, and 0.027, respectively) (Supplementary Table 6.2 & 6.3). The P-values for the association of metformin were near significant at the 9- and 12-month landmarks (0.053, and 0.054, respectively) (Supplementary Table 6.4 & 6.5). Therefore, landmark analysis showed that the beneficial association of metformin use with mortality in the presence of progressive myeloma was not likely due to immortal time bias.
Discussion
We have investigated the association of diabetes with adverse clinical outcomes of malignant diseases (Wentholt et al, 2008; He et al, 2011; Sadeghi et al, 2012), and different cancer populations have their similarities, differences, and unique challenges. Steroid-induced diabetes was significantly associated with decreased OS of MM patients and increased mortality in the presence of progressive myeloma. This is the first report that documents the association of SID with adverse outcomes of a malignant disease.
Analysis of anti-diabetic pharmacotherapy showed a strong association of usage of insulin and insulin analogues with decreased OS and increased cumulative incidence of death with progressive myeloma. In contrast, metformin might have an association with these outcome measures in the opposite direction. These results suggest that diabetes, especially SID, may promote myeloma progression, whereas the interaction of anti-diabetic pharmacotherapy with myeloma cells may be different based on the mechanisms of glycemic control as well as their potential direct effects on myeloma cells. It remains possible that patients with less severe insulin resistance may have received metformin or other oral anti-diabetic agents without insulins, and the ones with severe insulin resistance may have received insulins; it is not possible to cleanly separate the impact of insulin resistance from those of anti-diabetic pharmacotherapies in retrospective studies.
An alternative explanation for the difference in MM clinical outcome among the groups (HxD, SID, and ND) is that diabetic patients are generally in worse health and may receive less intensive MM treatment than non-diabetic patients. This hypothesis may be feasible for HxD, given that the proportion of patients with CCI >5 in HxD was higher than ND, and the proportion of patients who underwent stem cell transplantation in HxD was lower than ND (Supplementary Table 1). In contrast, it cannot explain the findings for SID because the proportions of patients with CCI >5 were the same in SID and ND, and the proportions of patients who underwent stem cell transplantation were also the same in SID and ND (Table 1). Of course, poor general health and comorbidities, for example, longer duration of diabetes, more chronic diabetic complications, and so on, may contribute to poor MM clinical outcome. We investigated this possibility by including the CCI in multivariate analyses. Although controlling for the contribution of comorbidities, use of insulin and analogues, and use of metformin remained as independent predictors of OS in a multivariate regression model (Table 3). Therefore, these anti-diabetic pharmacotherapies are associated with MM clinical outcome independent of comorbidities.
Another potential reason for a poor outcome of HxD MM patients may be delayed diagnosis because diabetes patients may have chronic diabetic complications similar to those of MM, for example, renal insufficiency and anemia. However, there was no significant difference in the ISS stage distribution among the HxD, SID, and ND groups. The potential impact of delayed diagnosis on prognosis in the HxD group was controlled for by including the ISS stage in the multivariate analyses.
MM cells express high levels of IR and IGF-1R (Freund et al, 1994), and insulin stimulates their growth (Freund et al, 1993; Sprynski et al, 2010) through IR/IGF-1R hybrid receptor activation (Sprynski et al, 2010). Activation of IR/IGF-1R signalling pathway can lead to dexamethasone resistance in myeloma cells (Xu et al, 1997; Kuhn et al, 2012). Taken together, the theory that endogenous insulin and exogenous insulin and analogues promote malignant cell growth and chemoresistance is a more feasible explanation for the findings in this study.
In contrast to insulin, metformin may be associated with favourable myeloma outcome, which is consistent with in vitro (Feng et al, 2011; Pan et al, 2012) and epidemiological findings (Wentholt et al, 2008; He et al, 2011; Sadeghi et al, 2012) in other malignancies. As pointed out by Suissa (2008), immortal time bias is a significant issue in retrospective studies of drug benefit in pharmaco-epidemiology. In this study, we have addressed the issue of immortal time bias regarding the benefit of metformin in diabetic myeloma patients using landmark analysis. As metformin is the first-line drug for type 2 diabetes, the majority of the patients with a history of type 2 diabetes who took metformin had their initiation of drug exposure before the diagnosis of myeloma. The induction chemotherapy for MM, which starts shortly after diagnosis and includes high-dose glucocorticoids that typically lasts for 6 months or more. About half of the SID patients who were treated with metformin would have had the initiation of drug exposure within 6 months of myeloma diagnosis. Therefore, 3, 6, 9, and 12 months were chosen as the time points for the landmark analysis. The association of metformin with increased OS in the multivariate Cox model remained significant for all these landmarks (Supplementary Table 4). Therefore, we are quite confident that immortal time bias did not accounted for this finding of drug benefit for metformin. As for the association of metformin with decreased cumulative incidence of death with progressive myeloma, the significant P-values in the landmark analysis of the multivariate model (Supplementary Table 6.1–6.3) became borderline at the 9-month and 12-month landmarks (Supplementary Table 6.4 & 6.5). Therefore, this association is less certain than that found between metformin and OS. Overall, our findings warrant further investigation of a potentially beneficial effect of metformin in diabetic myeloma patients.
Other limitations of our study include that the median age of our patients was in the late 50’s, which is younger than most typical myeloma patients. This difference may be due to the fact that our institution is a tertiary referral centre for cancer care. Our results will need to be confirmed in study populations from other institutions. Another limitation of our study is the small number of patients using thiazolidinediones and other anti-diabetic medications. This study does not have enough statistical power to exclude the possible effects of these pharmacological categories on MM.
At this time, no causal relationship can be established from the retrospective epidemiological data presented. Our findings raise an important hypothesis that must be further investigated. Can exogenous insulin therapy stimulate MM growth or protect MM from antineoplastic therapy? This hypothesis should be further researched in animal models. Future research is also needed to investigate how we can mitigate the challenge of hyperglycaemia, especially in the presence of high-dose glucocorticoids, without heavy reliance on exogenous insulin and analogues in diabetic MM patients. Ultimately, whether management of glucocorticoid-induced hyperglycaemia with an insulin-sparing anti-diabetic regimen can improve the survival of diabetic MM patients can only be answered by a randomised clinical trial.
Change history
29 July 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Benetatos L, Vartholomatos G (2012) Deregulated microRNAs in multiple myeloma. Cancer 118 (4): 878–887.
Boffetta P, Stellman SD, Garfinkel L (1989) A case-control study of multiple myeloma nested in the American Cancer Society prospective study. Int J Cancer 43 (4): 554–559.
Bommert K, Bargou RC, Stuhmer T (2006) Signalling and survival pathways in multiple myeloma. Eur J Cancer 42 (11): 1574–1580.
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40 (5): 373–383.
Chou YS, Yang CF, Chen HS, Yang SH, Yu YB, Hong YC, Liu CY, Gau JP, Liu JH, Chen PM, Chiou TJ, Tzeng CH, Hsiao LT (2012) Pre-existing diabetes mellitus in patients with multiple myeloma. Eur J Haematol 89 (4): 320–327.
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159 (12): 1160–1167.
Cozen W, Gebregziabher M, Conti DV, Van Den Berg DJ, Coetzee GA, Wang SS, Rothman N, Bernstein L, Hartge P, Morhbacher A, Coetzee SG, Salam MT, Wang W, Zadnick J, Ingles SA (2006) Interleukin-6-related genotypes, body mass index, and risk of multiple myeloma and plasmacytoma. Cancer Epidemiol Biomarkers Prev 15 (11): 2285–2291.
Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K, Gertz M, Dimopoulos M, Westin J, Sonneveld P, Ludwig H, Gahrton G, Beksac M, Crowley J, Belch A, Boccadaro M, Cavo M, Turesson I, Joshua D, Vesole D, Kyle R, Alexanian R, Tricot G, Attal M, Merlini G, Powles R, Richardson P, Shimizu K, Tosi P, Morgan G, Rajkumar SV International Myeloma Working G (2006) International uniform response criteria for multiple myeloma. Leukemia 20 (9): 1467–1473.
Feng YH, Velazquez-Torres G, Gully C, Chen J, Lee MH, Yeung SC (2011) The impact of type 2 diabetes and antidiabetic drugs on cancer cell growth. J Cell Mol Med 15 (4): 825–836.
Fortuny J, Benavente Y, Bosch R, Garcia-Villanueva M, de Sevilla AF, de Sanjose S (2005) Type 2 diabetes mellitus, its treatment and risk for lymphoma. Eur J Cancer 41 (12): 1782–1787.
Freund GG, Kulas DT, Mooney RA (1993) Insulin and IGF-1 increase mitogenesis and glucose metabolism in the multiple myeloma cell line, RPMI 8226. J Immunol 151 (4): 1811–1820.
Freund GG, Kulas DT, Way BA, Mooney RA (1994) Functional insulin and insulin-like growth factor-1 receptors are preferentially expressed in multiple myeloma cell lines as compared to B-lymphoblastoid cell lines. Cancer Res 54 (12): 3179–3185.
Gado K, Silva S, Paloczi K, Domjan G, Falus A (2001) Mouse plasmacytoma: an experimental model of human multiple myeloma. Haematologica 86 (3): 227–236.
Giobbie-Hurder A, Gelber RD, Regan MM (2013) Challenges of guarantee-time bias. J Clin Oncol 31 (23): 2963–2969.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D (2010) Diabetes and cancer: a consensus report. CACancer J Clin 60 (4): 207–221.
He XX, Tu SM, Lee MH, Yeung SC (2011) Thiazolidinediones and metformin associated with improved survival of diabetic prostate cancer patients. Ann Oncol 22 (12): 2640–2645.
Hofmann JN, Moore SC, Lim U, Park Y, Baris D, Hollenbeck AR, Matthews CE, Gibson TM, Hartge P, Purdue MP (2013) Body mass index and physical activity at different ages and risk of multiple myeloma in the NIH-AARP diet and health study. Am J Epidemiol 177 (8): 776–786.
Huang Q, Shi J, Feng A, Fan X, Zhang L, Mashimo H, Cohen D, Lauwers G (2011) Gastric cardiac carcinomas involving the esophagus are more adequately staged as gastric cancers by the 7th edition of the American Joint Commission on Cancer Staging System. Mod Pathol 24 (1): 138–146.
Kuhn DJ, Berkova Z, Jones RJ, Woessner R, Bjorklund CC, Ma W, Davis RE, Lin P, Wang H, Madden TL, Wei C, Baladandayuthapani V, Wang M, Thomas SK, Shah JJ, Weber DM, Orlowski RZ (2012) Targeting the insulin-like growth factor-1 receptor to overcome bortezomib resistance in preclinical models of multiple myeloma. Blood 120 (16): 3260–3270.
Mahindra A, Cirstea D, Raje N (2010) Novel therapeutic targets for multiple myeloma. Future Oncol 6 (3): 407–418.
Menu E, van Valckenborgh E, van Camp B, Vanderkerken K (2009) The role of the insulin-like growth factor 1 receptor axis in multiple myeloma. Arch Physiol Biochem 115 (2): 49–57.
Nilsen TI, Vatten LJ (2001) Prospective study of colorectal cancer risk and physical activity, diabetes, blood glucose and BMI: exploring the hyperinsulinaemia hypothesis. Br J Cancer 84 (3): 417–422.
Pan J, Chen C, Jin Y, Fuentes-Mattei E, Velazquez-Tores G, Benito JM, Konopleva M, Andreeff M, Lee MH, Yeung SC (2012) Differential impact of structurally different anti-diabetic drugs on proliferation and chemosensitivity of acute lymphoblastic leukemia cells. Cell Cycle 11 (12): 2314–2326.
Reseland JE, Reppe S, Olstad OK, Hjorth-Hansen H, Brenne AT, Syversen U, Waage A, Iversen PO (2009) Abnormal adipokine levels and leptin-induced changes in gene expression profiles in multiple myeloma. Eur J Haematol 83 (5): 460–470.
Richardson LC, Pollack LA (2005) Therapy insight: Influence of type 2 diabetes on the development, treatment and outcomes of cancer. Nat Clin Pract Oncol 2 (1): 48–53.
Sadeghi N, Abbruzzese JL, Yeung SC, Hassan M, Li D (2012) Metformin use is associated with better survival of diabetic patients with pancreatic cancer. Clin Cancer Res 18 (10): 2905–2912.
Sprynski AC, Hose D, Kassambara A, Vincent L, Jourdan M, Rossi JF, Goldschmidt H, Klein B (2010) Insulin is a potent myeloma cell growth factor through insulin/IGF-1 hybrid receptor activation. Leukemia 24 (11): 1940–1950.
Suissa S (2008) Immortal time bias in pharmaco-epidemiology. Am J Epidemiol 167 (4): 492–499.
Verlato G, Zoppini G, Bonora E, Muggeo M (2003) Mortality from site-specific malignancies in type 2 diabetic patients from Verona. Diabetes Care 26 (4): 1047–1051.
Vu K, Busaidy N, Cabanillas ME, Konopleva M, Faderl S, Thomas DA, O'Brien S, Broglio K, Ensor J, Escalante C, Andreeff M, Kantarjian H, Lavis V, Yeung SC (2012) A randomized controlled trial of an intensive insulin regimen in patients with hyperglycemic acute lymphoblastic leukemia. Clin Lymphoma, Myeloma & Leukemia 12 (5): 355–362.
Wallin A, Larsson SC (2011) Body mass index and risk of multiple myeloma: a meta-analysis of prospective studies. Eur J Cancer 47 (11): 1606–1615.
Weiser MA, Cabanillas ME, Konopleva M, Thomas DA, Pierce SA, Escalante CP, Kantarjian HM, O'Brien SM (2004) Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer 100 (6): 1179–1185.
Wentholt IM, Hart AA, Hoekstra JB, DeVries JH (2008) Evaluating clinical accuracy of continuous glucose monitoring devices: other methods. Curr Diabetes Rev 4 (3): 200–206.
Xu F, Gardner A, Tu Y, Michl P, Prager D, Lichtenstein A (1997) Multiple myeloma cells are protected against dexamethasone-induced apoptosis by insulin-like growth factors. Br J Haematol 97 (2): 429–440.
Acknowledgements
This work was supported by a grant from Susan G Komen for the Cure (PROMISE grant KG081048), and a Developmental Research Program Award of The MD Anderson Cancer Center SPORE in MM (National Cancer Institute P50 CA142509, PI: R Orlowski) to SC Yeung and MH Lee. W Wu was supported by Health Professional Training Grant from Department of Health of Fujian Province, China, and Grant from Xiamen Public Health Bureau for Science and technology project (3502z20077042 and WQK0605). The University of Texas MD Anderson Cancer Center was supported by a National Institutes of Health Cancer Center Support Grant (CA16672).
Author contributions
WW, AN, NS, and DS researched data. HL, VB, DB, KM, and SJY performed statistical analyses. WW, KM, MW, MHQ, VB, HL, DB, RZO, MHL, SJY contributed to discussion. SJY, DS, and KM wrote manuscript. WW, AN, NS, KM, DS, HL MW, MHQ, VB, HL, DB, RZO, MHL and SJY reviewed and edited manuscript. RZO and SJY provided financial resources for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wu, W., Merriman, K., Nabaah, A. et al. The association of diabetes and anti-diabetic medications with clinical outcomes in multiple myeloma. Br J Cancer 111, 628–636 (2014). https://doi.org/10.1038/bjc.2014.307
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.307
Keywords
This article is cited by
-
Pre-existing hypertension is associated with poor progression-free survival in newly diagnosed multiple myeloma patients
Journal of Thrombosis and Thrombolysis (2022)
-
The impact of oral hypoglycemics and statins on outcomes in myelodysplastic syndromes
Annals of Hematology (2022)
-
Association between diabetes and haematological malignancies: a population-based study
Diabetologia (2021)
-
Metformin induces autophagy and G0/G1 phase cell cycle arrest in myeloma by targeting the AMPK/mTORC1 and mTORC2 pathways
Journal of Experimental & Clinical Cancer Research (2018)
-
Pretreatment glycemic control status is an independent prognostic factor for cervical cancer patients receiving neoadjuvant chemotherapy for locally advanced disease
BMC Cancer (2017)