Abstract
Background:
Axitinib, a potent and selective second-generation inhibitor of vascular endothelial growth factor receptors, enhanced the efficacy of chemotherapy in human xenograft tumour models. This phase I study investigated the safety, tolerability, pharmacokinetics and antitumour activity of axitinib combined with chemotherapy.
Methods:
A total of 42 patients with advanced solid tumours received a continuous axitinib starting dose of 5 mg twice daily (b.i.d.) plus paclitaxel (90 mg m–2 weekly), docetaxel (100 mg m–2 every 3 weeks) or capecitabine (1000 or 1250 mg m–2 b.i.d., days 1–14).
Results:
Common treatment-related adverse events across all cohorts were nausea (45.2%), hypertension (45.2%), fatigue (42.9%), diarrhoea (38.1%), decreased appetite (33.3%) and hand–foot syndrome (31.0%). There was one complete response, nine partial responses and seven patients with stable disease. Ten patients (23.8%) remained on therapy for >8 months. Paclitaxel and capecitabine pharmacokinetics were similar in the absence or presence of axitinib, but docetaxel exposure was increased in the presence of axitinib. Axitinib pharmacokinetics were similar in the absence or presence of co-administered agents.
Conclusions:
Axitinib combined with paclitaxel or capecitabine was well tolerated; no additive increase in toxicities was observed. Antitumour activity was observed for each treatment regimen and across multiple tumour types.
Similar content being viewed by others
Main
It is clear that the efficacy of chemotherapy is limited by the development of drug resistance and the occurrence of significant toxicities associated with such agents. There remains an urgent need to enhance the activity of chemotherapy through combinations with biologically targeted drugs that may help overcome resistance and/or have non-overlapping mechanisms of action and side effects. Much of the current clinical research has focussed on targeting angiogenesis pathways as a means to enhance chemotherapy efficacy, as these pathways are critical to tumour growth and metastasis. Tumour angiogenesis is mediated largely by vascular endothelial growth factor (VEGF) and its tyrosine kinase receptor VEGFR (Folkman, 1990, 1992; Ferrara et al, 2003; Hicklin and Ellis, 2005). Several angiogenesis inhibitors that target VEGF/VEGFR are approved or in clinical development (Tugues et al, 2011).
The strategy of combining drugs that inhibit VEGF signalling with chemotherapy is supported by several phase III clinical trials that showed that regimens of bevacizumab, an anti-VEGF monoclonal antibody, plus chemotherapy improved outcomes compared with chemotherapy alone in patients with metastatic colorectal cancer (CRC), advanced non-squamous non-small cell lung cancer (NSCLC) and metastatic breast cancer (Hurwitz et al, 2004; Miller et al, 2005; Sandler et al, 2006; Miller et al, 2007). Although the beneficial results to date have been seen mainly with drugs that bind to receptor ligands (e.g., VEGF) involved in angiogenesis, further improvement in patient outcomes may be achieved using agents that target this pathway by other mechanisms (e.g., kinase inhibition).
Axitinib is a potent, oral and selective second-generation inhibitor of VEGFR 1, 2 and 3 (Hu-Lowe et al, 2008). In preclinical studies, axitinib demonstrated antiangiogenic and antitumour activity in human tumour models. Phase II or phase III studies have shown that axitinib has single-agent clinical activity in a range of tumour types, including renal cell carcinoma (Rixe et al, 2007; Rini et al, 2009, 2011), thyroid cancer (Cohen et al, 2008), NSCLC (Schiller et al, 2009) and melanoma (Fruehauf et al, 2011). Preclinical studies showed that axitinib enhanced the antitumour efficacy of a number of chemotherapeutic agents, including docetaxel, carboplatin and gemcitabine (Hu-Lowe et al, 2008). Axitinib is approved in the United States for the treatment of advanced renal cell carcinoma after failure of one prior systemic therapy (Pfizer Inc., 2012).
The phase I study presented here investigated the safety, tolerability, pharmacokinetics and antitumour activity of axitinib in combination with weekly paclitaxel, docetaxel or capecitabine in patients with advanced solid tumours, including breast cancer and CRC. Another component of this study, which investigated axitinib plus chemotherapy doublet regimens commonly used in the treatment of advanced NSCLC, is reported in an accompanying article (Kozloff et al, 2012).
Materials and methods
Study design and end points
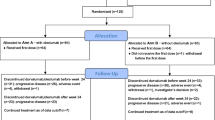
As part of an open-label, multicentre, phase I study, patients with advanced solid tumours were treated with axitinib in combination with standard doses and schedules of paclitaxel, docetaxel or capecitabine. The primary end point was maximum tolerated dose (MTD) of axitinib plus paclitaxel, docetaxel or capecitabine. Secondary end points were safety, tumour response rates and plasma pharmacokinetics.
The trial was performed in accordance with the International Conference on Harmonisation Guidelines on Good Clinical Practice and applicable local regulatory requirements and laws. All patients provided written informed consent. This trial is registered on ClinicalTrials.gov (NCT00454649).
Patients
Adult patients (⩾18 years of age) with histologically or cytologically proven advanced solid tumours suitable for treatment with taxanes or capecitabine were eligible. Key inclusion criteria included Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1; adequate liver, renal and bone marrow function; and no pre-existing uncontrolled hypertension (i.e., blood pressure (BP) ⩾140/90 mm Hg). Patients whose hypertension was controlled with antihypertensive therapy were eligible. For patients receiving axitinib plus docetaxel, no prior cytotoxic chemotherapy was allowed, except adjuvant treatment completed ⩾12 months before enrolment. Patients receiving axitinib plus weekly paclitaxel or capecitabine may have received any type of prior chemotherapy.
Key exclusion criteria included central nervous system metastases; clinically significant gastrointestinal abnormalities; myocardial infarction, severe/unstable angina, coronary/peripheral artery bypass graft, congestive heart failure, cerebrovascular accident (including transient ischaemic attack) or pulmonary embolus <12 months before enrolment; haemoptysis (>0.5 teaspoon of blood per day) within 1 week of enrolment; and one or more lung lesions with cavitation or any lesion invading and/or supporting large blood vessels.
Study treatments
The schedules for the four treatment cohorts are shown in Figure 1. Patients in all cohorts received axitinib 5 mg twice daily (b.i.d.) administered orally with food. A lead-in period, during which patients received an axitinib starting dose of 5 mg b.i.d., was utilised in the axitinib/docetaxel cohort. After cycle 1, patients with no grade >2 adverse events (AEs) related to axitinib for consecutive 2-week periods could have their axitinib dose titrated to 7 mg b.i.d. and then to a maximum of 10 mg b.i.d., unless BP measured >150/100 mm Hg or the patient was receiving antihypertensive medication. In patients who developed systolic BP >150 mm Hg or diastolic BP >100 mm Hg, antihypertensive therapy was initiated or the dose of current medication increased. In patients with grade ⩾3 nonhaematologic treatment-related AEs, axitinib was reduced to 3 mg b.i.d. and then, if needed, to 2 mg b.i.d. Axitinib was discontinued and a radiologic assessment was considered in patients who developed haemoptysis (>0.5 teaspoon of bright red blood per day).
Paclitaxel was administered in 4-week cycles as a 60-min intravenous (i.v.) infusion of 90 mg m−2 once weekly on days 1, 8 and 15 of each cycle, followed by a 1-week rest period. Docetaxel was administered in 3-week cycles as a 60-min i.v. infusion of 100 mg m−2 once every 3 weeks on day 1 of each treatment cycle. Two cohorts of patients received oral capecitabine in 3-week cycles as 1000 mg m−2 and 1250 mg m−2 b.i.d., respectively, within 30 min of a meal on days 1–14 of each treatment cycle, followed by a 1-week rest period. Chemotherapy doses were modified at the discretion of the investigator. Paclitaxel, docetaxel and capecitabine were delayed in patients with absolute granulocyte counts <1500 cells mm−3 or platelet counts <100 000 cells mm−3 and discontinued if recovery did not occur after 4 weeks. Patients with abnormal liver function tests had their dose of paclitaxel or docetaxel reduced. The dose of paclitaxel and docetaxel was withheld in patients with grade ⩾3 haematologic or nonhaematologic toxicities and resumed at one lower dose level when the toxicity was grade ⩽1. Paclitaxel and docetaxel were reduced in patients with grade 2 neurotoxicity or withheld until neurotoxicity was grade ⩽1. Capecitabine was interrupted in patients with grade ⩾2 toxicities and resumed when the toxicity was grade ⩽1, with capecitabine administered at a lower dose level if the toxicity was grade 2 and previously reported or grade 3. In patients with grade 4 toxicities, capecitabine was discontinued or interrupted and resumed when the toxicity was grade ⩽1. Treatment with chemotherapy and axitinib continued until disease progression or unacceptable toxicity. Patients who discontinued chemotherapy because of toxicity or who reached a maximum number of cycles according to institutional guidelines were allowed to continue treatment with axitinib monotherapy. Patients who permanently discontinued axitinib because of toxicity could continue to receive chemotherapy as long as such treatment was considered beneficial, at the discretion of the treating physician.
Assessments
The MTD for axitinib plus paclitaxel, docetaxel or capecitabine was defined as the highest dose level at which no more than one of the first six patients enrolled in each cohort experienced a dose-limiting toxicity (DLT) during the first cycle of therapy with two or more of the six patients experiencing a DLT at the next highest dose level. If the MTD was not exceeded within the planned dose levels, the MTD was defined as the maximum dose tested. The DLTs were defined as grade 4 neutropenia or thrombocytopenia for ⩾14 days or grade 4 febrile neutropenia; proteinuria ⩾2 g per 24 h; haemoptysis (⩾0.5 teaspoon per day) for ⩾7 days; uncontrolled grade ⩾3 nonhaematologic toxicity for ⩾7 days; or inability to resume study treatment within 14 days after stopping because of axitinib-related toxicity.
Severity of AEs was graded according to the Common Terminology Criteria for Adverse Events, version 3.0 (Trotti et al, 2003). Physical examinations, assessment of ECOG PS, chest X-rays and laboratory tests were conducted at baseline, day 1 of each cycle and at follow-up (28 days after the last dose). Additional physical examinations and haematology tests were performed at days 8 and 15 of each cycle. Measurements of BP were recorded at clinic visits and b.i.d. using a BP monitoring cuff and measurement diary by patients, who were instructed to contact their physicians immediately for systolic BP >150 mm Hg, diastolic BP >100 mm Hg or symptoms related to elevated BP. Home BP measurements were not used to assess DLTs. Objective tumour responses were radiologically assessed every two cycles according to Response Evaluation Criteria in Solid Tumours (RECIST version 1.0) (Therasse et al, 2000).
Pharmacokinetic analysis
Pharmacokinetics of axitinib alone were determined using blood samples collected on cycle 1 day 22 for patients receiving axitinib/paclitaxel, on cycle 1 day –1 for those receiving axitinib/docetaxel and on cycle 1 day 18 for those receiving axitinib/capecitabine. Pharmacokinetics of chemotherapy alone were determined using blood samples collected on cycle 2 day 1 for all treatment regimens. Pharmacokinetics of axitinib plus chemotherapy were determined using blood samples collected on cycle 1 day 1 for patients receiving axitinib/docetaxel and on cycle 1 day 8 for patients receiving axitinib/paclitaxel or axitinib/capecitabine. Samples for axitinib analysis were collected before dose and 1, 2, 3, 4, 6 and 8 h post dose. Samples for paclitaxel analysis were collected before dose and 0.5, 1, 2, 3, 4, 6, 8, 24 and 30 h after the start of paclitaxel infusion. Samples for docetaxel analysis were collected before dose and 0.5, 1, 1.5, 2, 3, 4, 6, 8, 24 and 30 h after the start of docetaxel infusion. Samples for capecitabine analysis were collected before dose and 0.25, 0.5, 1, 2, 3, 4, 6 and 8 h post dose. Plasma concentrations of axitinib were measured using a validated high-performance liquid chromatography with tandem mass spectrometric detection method (LC/MS/MS; Charles River Discovery and Development Services, Shrewsbury, MA, USA) (Rugo et al, 2005). Concentrations of paclitaxel and docetaxel (Covance Bioanalytical Services, Indianapolis, IN, USA) and capecitabine and metabolites (BASi, McMinnville, OR, USA) were measured using a validated LC/MS/MS assay. Pharmacokinetic parameter estimates were conducted using WinNonlin Professional (version 4.1; Pharsight Corp., Mountain View, CA, USA).
Statistical methods
All patients who received at least one dose of study medication were included in the safety analysis. Patients with one or more target lesions according to RECIST, who received at least one dose of study medication and who had a baseline assessment of disease were included in the analysis of best objective response. Descriptive statistics (including mean, median, standard error, ranges for continuous data and frequencies and percentages for categorical data) were reported for safety and pharmacokinetic analyses.
Results
Patient characteristics
A total of 42 patients were enrolled in the four treatment cohorts (Table 1). The axitinib/capecitabine 1250 mg m−2 b.i.d. group was expanded in August 2007 to include an additional 12 patients. Median chemotherapy exposure was two cycles of paclitaxel (range 2–6), four cycles of docetaxel (range 1–17), two cycles of 1000 mg m–2 capecitabine (range 1–11) and four cycles of 1250 mg m–2 capecitabine (range 1–24). Median chemotherapy doses per cycle were 225 mg m–2 paclitaxel (75 mg m–2 weekly), 78.6 mg m–2 docetaxel, and 7000 mg and 5825 mg capecitabine in the 1000 mg m−2 b.i.d. and 1250 mg m−2 b.i.d. cohorts, respectively. Median axitinib exposure was 136 days (range 43–1085), with a median daily dose of 6.4 mg (range 3.9–12.1), in the axitinib/paclitaxel group; 74 days (range 10–599), with a median daily dose of 8.7 mg (range 2.6–10.0), in the axitinib/docetaxel group; 42 days (range 2–290), with a median daily dose of 10.0 mg (range 5.2–10.0), in the axitinib/capecitabine 1000 mg m−2 b.i.d. group; and 75 days (range 18–593), with a median daily dose of 7.5 mg (range 4.4–10.0), in the axitinib/capecitabine 1250 mg m−2 b.i.d. group. Ten (23.8%) patients remained on therapy for >8 months in the axitinib/paclitaxel (n=3), axitinib/docetaxel (n=2) and axitinib/capecitabine (n=5) cohorts.
In all, 20 patients required an axitinib dose reduction because of any causality AEs: axitinib/paclitaxel cohort (n=5; 71.4%), axitinib/docetaxel cohort (n=4; 57.1%), axitinib/capecitabine 1000 mg m−2 b.i.d. cohort (n=2; 22.2%) and axitinib/capecitabine 1250 mg m−2 b.i.d. cohort (n=9; 47.4%). Twenty-nine patients required axitinib dose interruptions for any causality AEs: axitinib/paclitaxel cohort (n=4; 57.1%), axitinib/docetaxel cohort (n=5; 71.4%), axitinib/capecitabine 1000 mg m−2 b.i.d. cohort (n=6; 66.7%) and axitinib/capecitabine 1250 mg m−2 b.i.d. cohort (n=14; 73.7%).
In the axitinib/paclitaxel cohort, six patients discontinued study because of insufficient clinical response (n=3) or for other reasons (n=3). All patients receiving axitinib/docetaxel discontinued the study because of AEs (n=2), insufficient clinical response (n=4) or for other reasons (n=1). All patients receiving axitinib/capecitabine discontinued the study because of AEs (n=7), insufficient clinical response (n=18) or for other reasons (n=3).
DLTs and MTD
None of the first six patients receiving axitinib/paclitaxel experienced a DLT during the first cycle, and the MTD was determined to be axitinib 5 mg b.i.d. continuously in combination with weekly paclitaxel 90 mg m−2. In the axitinib/docetaxel cohort, three of the first six patients experienced DLTs during the first cycle: stomatitis and hand–foot syndrome (n=1), mucositis (n=1) and colitis (n=1). Axitinib 5 mg b.i.d. continuously in combination with docetaxel 100 mg m−2 was determined to exceed the MTD. One of the first six patients receiving axitinib/capecitabine 1000 mg m−2 had a DLT of hypertension and seizure, and one of the first six patients receiving axitinib/capecitabine 1250 mg m−2 experienced a DLT comprising diarrhoea, urinary tract infection and dyspnoea during the first cycle. The MTD was determined to be axitinib 5 mg b.i.d. continuously in combination with capecitabine 1250 mg m−2. Dose escalation to 10 mg b.i.d. was achieved in one patient receiving axitinib/paclitaxel; this patient required a subsequent axitinib dose reduction.
Adverse events
Serious treatment-related AEs occurred in 12 patients: 1 receiving axitinib/paclitaxel, 4 receiving axitinib/docetaxel and 7 receiving axitinib/capecitabine. Commonly reported treatment-related AEs were nausea (n=19; 45.2%), hypertension (n=19; 45.2%), fatigue (n=18; 42.9%) and diarrhoea (n=16; 38.1%; Table 2). Grade 4 treatment-related AEs were neutropenia and colitis (n=1 each) in the axitinib/docetaxel cohort and hypertension and dyspnoea (n=1 each) in the axitinib/capecitabine cohorts. No grade 5 treatment-related AEs were reported. Common haematologic laboratory abnormalities were anaemia and lymphopenia, reported in 79.5% and 71.8% of evaluable patients, respectively (Table 2); all cases of anaemia were grade ⩽2. Grade 4 haematologic laboratory abnormalities were one case of thrombocytopenia in the axitinib/paclitaxel cohort and five cases of neutropenia in the axitinib/docetaxel (n=4) and axitinib/capecitabine (n=1) cohorts. Treatment-related haematologic laboratory abnormalities reported as AEs were anaemia and neutropenia (n=3 each) and thrombocytopenia (n=1). Nine patients discontinued the study because of AEs, including two patients receiving axitinib/docetaxel and seven patients receiving axitinib/capecitabine; three of the nine were treatment related.
Antitumour activity
A total of 10 patients achieved objective responses (Table 3), including one complete response in a patient with squamous cell skin cancer who received axitinib/docetaxel; this patient had metastatic disease with lesions in lymph nodes (n=2) and neck (n=1). Nine partial responses were recorded in patients with thyroid cancer (n=3) or with CRC, melanoma or breast, hepatocellular, ovarian or pancreatic cancers (n=1 each). Seven patients had stable disease for >8 weeks.
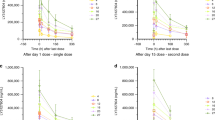
Pharmacokinetics
Overall, the pharmacokinetic parameters for paclitaxel and capecitabine were similar in the absence or presence of axitinib (Table 4 and Figure 2). Docetaxel pharmacokinetic parameters in the small cohort of patients appeared to indicate higher exposure in the presence of axitinib. Axitinib drug concentrations and pharmacokinetic parameters were largely unchanged when co-administered with any of the chemotherapeutic agents studied compared with axitinib alone (Table 4 and Figure 2).
Plasma concentration–time curves. (A) Axitinib/paclitaxel: Left panel, one patient excluded because cycle 2 day 1 pharmacokinetic (PK) samples were not collected. Right panel, two patients excluded because cycle 1 day 1 pharmacokinetics samples were not collected. (B) Axitinib/docetaxel: Left panel, two patients excluded because matching cycle 1 and cycle 2 PK evaluations were not completed. (C) Axitinib/capecitabine: Upper left panel, three patients excluded because matching cycle 1 and cycle 2 PK evaluations were not completed. Upper right panel, two patients excluded because matching cycle 1 and cycle 2 PK evaluations not completed and six patients excluded because of dose change from cycle 1 to cycle 2. Lower left panel, one patient excluded because matching cycle 1 and cycle 2 PK evaluations were not completed and one patient excluded because of dose reduction. Lower right panel, three patients excluded because matching cycle 1 and cycle 2 PK evaluations were not completed and two patients excluded because of dose reduction. *1000 mg m−2; †1250 mg m−2.
Discussion
Paclitaxel or capecitabine was well tolerated when administered in combination with axitinib in patients with advanced solid tumours. Based on the DLTs observed in this study, the recommended phase II doses of axitinib combined with chemotherapy are 5 mg axitinib b.i.d. plus standard-dose paclitaxel (90 mg m−2) or capecitabine (1000 mg m−2 or 1250 mg m−2 b.i.d.). The combination of axitinib 5 mg b.i.d. plus docetaxel 100 mg m−2 was found to be above the MTD. In addition, two patients in this cohort experienced febrile neutropenia and subsequent reductions in docetaxel doses were often required. These results are consistent with findings from a randomised phase II study that reported a numerically higher incidence of febrile neutropenia among patients with metastatic breast cancer receiving continuous axitinib 5 mg b.i.d. plus docetaxel 80 mg m−2 compared with docetaxel alone (Rugo et al, 2011).
Most AEs reported in patients receiving either axitinib/paclitaxel or axitinib/capecitabine were grade ⩽2 in severity (Table 2), which were manageable and similar to those previously seen with the respective chemotherapeutic agents (Crown and O'Leary, 2000; Eniu et al, 2005; Walko and Lindley, 2005) or single-agent axitinib (Rixe et al, 2007; Cohen et al, 2008; Rini et al, 2009; Schiller et al, 2009; Fruehauf et al, 2011). No apparent additive increases in toxicities were observed when axitinib was combined with paclitaxel or capecitabine. Dose reductions or treatment interruptions for axitinib, paclitaxel or capecitabine due to AEs were common, although discontinuation due to AEs was only required in a small proportion of patients.
Although paclitaxel and axitinib are primarily metabolised through distinct primary pathways – paclitaxel primarily via cytochrome P450 2C8 (CYP2C8) (Steed and Sawyer, 2007) and axitinib primarily via CYP3A4/5 (Pithavala et al, 2010) – results from in vitro analyses demonstrated that axitinib inhibits CYP2C8 with an inhibition coefficient of 0.5 μmol l−1 (Pfizer Inc., data on file), which suggests that axitinib has the potential to increase plasma concentrations of paclitaxel when administered in combination. In this study, paclitaxel exposure was similar when administered alone or in combination with axitinib. Moreover, the maximum plasma concentration of axitinib observed when the drug was co-administered with paclitaxel was 35.4 ng ml−1, which is substantially lower than 193.23 ng ml−1 (0.5 μmol l−1) required for CYP2C8 inhibition. Together, these results suggest that at clinical concentrations, axitinib does not inhibit CYP2C8.
Similarly, no change in capecitabine exposure was observed in the absence or presence of axitinib. However, 5-fluorouracil exposure was higher when capecitabine was co-administered with axitinib. Similar results were observed in a phase I study of the experimental epidermal growth factor receptor tyrosine kinase inhibitor EKB-569, in which 5-fluorouracil exposure was increased approximately two-fold when capecitabine was given in combination with EKB-569 compared with single-agent administration (Laheru et al, 2008). In contrast, results of a ongoing clinical study have shown that axitinib may be co-administered with 5-fluorouracil (as part of the folinic acid and 5-fluorouracil plus oxaliplatin (FOLFOX) or folinic acid and 5-fluorouracil plus irinotecan (FOLFIRI) regimens) without affecting the plasma concentration of either drug (Sharma et al, 2010). The observed differences in 5-fluorouracil exposure during co-administration with targeted agents may reflect the variability associated with the three-step metabolic process required for conversion of the capecitabine pro-drug to its active metabolite (Walko and Lindley, 2005). Overall, in the current study, the observed pharmacokinetic parameters and plasma profiles for axitinib, paclitaxel and capecitabine/5-fluorouracil were consistent with previously reported data (Kondo et al, 2005; Rugo et al, 2005; Albanell et al, 2008; Laheru et al, 2008).
In contrast, co-administration of axitinib and docetaxel appeared to change the pharmacokinetics of docetaxel. Although the sample size was small (n=5 for assessment of area under the plasma concentration–time curve from time zero to infinity (AUC0–∞) in the axitinib/docetaxel cohort), mean docetaxel exposure was ∼55% higher in the presence of continuous b.i.d. dosing with axitinib. Docetaxel exposure, when administered alone as observed in this study (4417 ng·h ml−1) was similar to what has been previously reported (Brunsvig et al, 2007). Our study was not statistically powered to enable a rigorous assessment of the quantitative change in exposure of each drug; however, an alteration in docetaxel pharmacokinetics in the presence of axitinib could not be excluded. Both drugs are primarily metabolised by the CYP3A4 pathway and are highly bound to plasma proteins (Clarke and Rivory, 1999; Tortorici et al, 2011). Changes in hepatic clearance and protein binding of axitinib and docetaxel may affect the disposition of these drugs, as both are characterised by a low hepatic extraction ratio (Crommentuyn et al, 1998). To avoid this potential increase in docetaxel exposure, an investigation of temporary interruption of axitinib dosing around the time of docetaxel administration is warranted.
To date, randomised clinical trials have not shown improved outcomes for tyrosine kinase inhibitors combined with chemotherapy compared with chemotherapy alone in the treatment of various cancers. Although this study was a phase I trial enrolling patients with diverse malignancies and treatment histories, preliminary evidence of antitumour activity was observed, with responses reported in each treatment cohort and across multiple tumour types. Co-administration of axitinib with chemotherapeutic agents was not associated with overlapping toxicities, making this an attractive strategy for cancer therapy. Larger studies are needed to document increases in efficacy with combination regimens of axitinib plus chemotherapy compared with chemotherapy alone. In a phase II study in metastatic breast cancer, higher objective response rates were seen with axitinib/docetaxel compared with docetaxel/placebo (41.1% vs 23.6%, respectively; P=0.011) (Rugo et al, 2011). Ongoing and recently completed studies of axitinib in combination with chemotherapy include a phase II study of axitinib compared with bevacizumab plus FOLFOX or FOLFIRI for metastatic CRC (NCT00615056), a phase II study of axitinib plus FOLFOX and bevacizumab as first-line treatment for metastatic CRC (NCT00460603) and a phase I study of axitinib plus cisplatin/capecitabine for advanced gastric cancer (NCT00842244).
Change history
04 October 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Albanell J, Montagut C, Jones ET, Pronk L, Mellado B, Beech J, Gascon P, Zugmaier G, Brewster M, Saunders MP, Valle JW (2008) A phase I study of the safety and pharmacokinetics of the combination of pertuzumab (rhuMab 2C4) and capecitabine in patients with advanced solid tumors. Clin Cancer Res 14: 2726–2731
Brunsvig PF, Andersen A, Aamdal S, Kristensen V, Olsen H (2007) Pharmacokinetic analysis of two different docetaxel dose levels in patients with non-small cell lung cancer treated with docetaxel as monotherapy or with concurrent radiotherapy. BMC Cancer 7: 197
Clarke SJ, Rivory LP (1999) Clinical pharmacokinetics of docetaxel. Clin Pharmacokinet 36: 99–114
Cohen EE, Rosen LS, Vokes EE, Kies MS, Forastiere AA, Worden FP, Kane MA, Sherman E, Kim S, Bycott P, Tortorici M, Shalinsky DR, Liau KF, Cohen RB (2008) Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. J Clin Oncol 26: 4708–4713
Crommentuyn KM, Schellens JH, van den Berg JD, Beijnen JH (1998) In-vitro metabolism of anti-cancer drugs, methods and applications: paclitaxel, docetaxel, tamoxifen and ifosfamide. Cancer Treat Rev 24: 345–366
Crown J, O'Leary M (2000) The taxanes: an update. Lancet 355: 1176–1178
Eniu A, Palmieri FM, Perez EA (2005) Weekly administration of docetaxel and paclitaxel in metastatic or advanced breast cancer. Oncologist 10: 665–685
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9: 669–676
Folkman J (1990) What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst 82: 4–6
Folkman J (1992) The role of angiogenesis in tumor growth. Semin Cancer Biol 3: 65–71
Fruehauf J, Lutzky J, McDermott D, Brown CK, Meric JB, Rosbrook B, Shalinsky DR, Liau KF, Niethammer AG, Kim S, Rixe O (2011) Multicenter, phase II study of axitinib, a selective second-generation inhibitor of vascular endothelial growth factor receptors 1, 2, and 3, in patients with metastatic melanoma. Clin Cancer Res 17: 7462–7469
Hicklin DJ, Ellis LM (2005) Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol 23: 1011–1027
Hu-Lowe DD, Zou HY, Grazzini ML, Hallin ME, Wickman GR, Amundson K, Chen JH, Rewolinski DA, Yamazaki S, Wu EY, McTigue MA, Murray BW, Kania RS, O'Connor P, Shalinsky DR, Bender SL (2008) Nonclinical antiangiogenesis and antitumor activities of axitinib (AG-013736), an oral, potent, and selective inhibitor of vascular endothelial growth factor receptor tyrosine kinases 1, 2, 3. Clin Cancer Res 14: 7272–7283
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350: 2335–2342
Kondo K, Kobayashi M, Kojima H, Hirabayashi N, Kataoka M, Araki K, Matsui T, Takiyama W, Miyashita Y, Nakazato H, Nakao A, Sakamoto J (2005) Phase I evaluation of continuous 5-fluorouracil infusion followed by weekly paclitaxel in patients with advanced or recurrent gastric cancer. Jpn J Clin Oncol 35: 332–337
Kozloff MF, Martin LP, Krzakowski M, Samuel TA, Rado TA, Arriola E, De Castro Carpen J, Herbst RS, Tarazi J, Kim S, Rosbrook B, Tortorici M, Olszanski AJ, Cohen RB (2012) Phase I trial of axitinib combined with platinum doublets in patients with advanced non-small cell lung cancer and other solid tumours. Br J Cancer e-pub ahead of print 18 September 2012; doi:10.1038/bjc.2012.406
Laheru D, Croghan G, Bukowski R, Rudek M, Messersmith W, Erlichman C, Pelley R, Jimeno A, Donehower R, Boni J, Abbas R, Martins P, Zacharchuk C, Hidalgo M (2008) A phase I study of EKB-569 in combination with capecitabine in patients with advanced colorectal cancer. Clin Cancer Res 14: 5602–5609
Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, Shenkier T, Cella D, Davidson NE (2007) Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med 357: 2666–2676
Miller KD, Chap LI, Holmes FA, Cobleigh MA, Marcom PK, Fehrenbacher L, Dickler M, Overmoyer BA, Reimann JD, Sing AP, Langmuir V, Rugo HS (2005) Randomized phase III trial of capecitabine compared with bevacizumab plus capecitabine in patients with previously treated metastatic breast cancer. J Clin Oncol 23: 792–799
Pfizer Inc (2012) Inlyta® (Axitinib) Prescribing Information. Pfizer Inc: New York, NY
Pithavala YK, Tortorici M, Toh M, Garrett M, Hee B, Kuruganti U, Ni G, Klamerus KJ (2010) Effect of rifampin on the pharmacokinetics of Axitinib (AG-013736) in Japanese and Caucasian healthy volunteers. Cancer Chemother Pharmacol 65: 563–570
Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, Michaelson MD, Gorbunova VA, Gore ME, Rusakov IG, Negrier S, Ou YC, Castellano D, Lim HY, Uemura H, Tarazi J, Cella D, Chen C, Rosbrook B, Kim S, Motzer RJ (2011) Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet 378: 1931–1939
Rini BI, Wilding G, Hudes G, Stadler WM, Kim S, Tarazi J, Rosbrook B, Trask PC, Wood L, Dutcher JP (2009) Phase II study of axitinib in sorafenib-refractory metastatic renal cell carcinoma. J Clin Oncol 27: 4462–4468
Rixe O, Bukowski RM, Michaelson MD, Wilding G, Hudes GR, Bolte O, Motzer RJ, Bycott P, Liau KF, Freddo J, Trask PC, Kim S, Rini BI (2007) Axitinib treatment in patients with cytokine-refractory metastatic renal-cell cancer: a phase II study. Lancet Oncol 8: 975–984
Rugo HS, Herbst RS, Liu G, Park JW, Kies MS, Steinfeldt HM, Pithavala YK, Reich SD, Freddo JL, Wilding G (2005) Phase I trial of the oral antiangiogenesis agent AG-013736 in patients with advanced solid tumors: pharmacokinetic and clinical results. J Clin Oncol 23: 5474–5483
Rugo HS, Stopeck AT, Joy AA, Chan S, Verma S, Lluch A, Liau KF, Kim S, Bycott P, Rosbrook B, Bair AH, Soulieres D (2011) Randomized, placebo-controlled, double-blind, phase II study of axitinib plus docetaxel versus docetaxel plus placebo in patients with metastatic breast cancer. J Clin Oncol 29: 2459–2465
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355: 2542–2550
Schiller JH, Larson T, Ou SH, Limentani S, Sandler A, Vokes E, Kim S, Liau K, Bycott P, Olszanski AJ, von Pawel J (2009) Efficacy and safety of axitinib in patients with advanced non-small-cell lung cancer: results from a phase II study. J Clin Oncol 27: 3836–3841
Sharma S, Abhyankar V, Burgess RE, Infante J, Trowbridge RC, Tarazi J, Kim S, Tortorici M, Chen Y, Robles RL (2010) A phase I study of axitinib (AG-013736) in combination with bevacizumab plus chemotherapy or chemotherapy alone in patients with metastatic colorectal cancer and other solid tumors. Ann Oncol 21: 297–304
Steed H, Sawyer MB (2007) Pharmacology, pharmacokinetics and pharmacogenomics of paclitaxel. Pharmacogenomics 8: 803–815
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205–216
Tortorici MA, Toh M, Rahavendran SV, Labadie RR, Alvey CW, Marbury T, Fuentes E, Green M, Ni G, Hee B, Pithavala YK (2011) Influence of mild and moderate hepatic impairment on axitinib pharmacokinetics. Invest New Drugs 29: 1370–1380
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13: 176–181
Tugues S, Koch S, Gualandi L, Li X, Claesson-Welsh L (2011) Vascular endothelial growth factors and receptors: anti-angiogenic therapy in the treatment of cancer. Mol Aspects Med 32: 88–111
Walko CM, Lindley C (2005) Capecitabine: a review. Clin Ther 27: 23–44
Acknowledgements
This study was sponsored by Pfizer Inc. Additional support was provided to Fox Chase Cancer Center by Grant 5P30CA006927 from the National Cancer Institute. We thank the patients who participated in this study and the physicians who referred them as well as the study coordinators and data managers, Shelley Mayfield and Carol Martins at Pfizer Inc., for support of the study conduct and Gamal ElSawah, Pfizer Medical Affairs, for his review of the manuscript. Medical writing support was provided by Joanna Bloom of UBC Scientific Solutions (Southport, CT, USA) and Christine Arris of ACUMED (Tytherington, UK) and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Martin, L., Kozloff, M., Herbst, R. et al. Phase I study of axitinib combined with paclitaxel, docetaxel or capecitabine in patients with advanced solid tumours. Br J Cancer 107, 1268–1276 (2012). https://doi.org/10.1038/bjc.2012.407
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.407
Keywords
This article is cited by
-
Clinical Pharmacokinetics of Paclitaxel Monotherapy: An Updated Literature Review
Clinical Pharmacokinetics (2018)
-
Impact of pazopanib on docetaxel exposure: results of a phase I combination study with two different docetaxel schedules
Cancer Chemotherapy and Pharmacology (2015)
-
Inhibition of OATP1B1 by tyrosine kinase inhibitors: in vitro–in vivo correlations
British Journal of Cancer (2014)
-
Practical Guidelines for Therapeutic Drug Monitoring of Anticancer Tyrosine Kinase Inhibitors: Focus on the Pharmacokinetic Targets
Clinical Pharmacokinetics (2014)
-
Clinical Pharmacology of Axitinib
Clinical Pharmacokinetics (2013)