Abstract
Aim:
Oral risedronate is effective in the treatment of postmenopausal osteoporosis when administered daily, weekly, or monthly. In this 1-year, randomized, double-blind, multicenter study we compared the weekly 35-mg and daily 5-mg risedronate dosing regimens in the treatment of Chinese postmenopausal women with osteoporosis or osteopenia.
Methods:
Postmenopausal women with primary osteoporosis or osteopenia were randomly assigned to the weekly group or daily group (n=145 for each) that received oral risedronate 35 mg once a week or 5 mg daily, respectively, for 1 year. The subjects' bone mineral densities (BMDs), bone turnover markers (P1NP and β-CTX), new vertebral fractures, and adverse events were assessed at baseline and during the treatments.
Results:
All subjects in the weekly group and 144 subjects in the daily group completed the study. The primary efficacy endpoint after 1 year, ie the mean percent changes in the lumbar spine BMD (95% CI) were 4.87% (3.92% to 5.81%) for the weekly group and 4.35% (3.31% to 5.39%) for the daily group. The incidences of clinical adverse events were 48.3% in the weekly group and 54.2% in the daily group.
Conclusion:
The weekly 35-mg and daily 5-mg risedronate dosing regimens during 1 year of follow-up show similar efficacy in improving BMDs and biochemical markers of bone turnover in Chinese postmenopausal women with osteoporosis or osteopenia. Moreover, the two dosing regimens exhibit similar safety and tolerability.
Similar content being viewed by others
Introduction
Risedronate is a pyridinyl bisphosphonate that has been shown in prospective studies to reduce the risk of vertebral, nonvertebral, and hip fractures1,2,3. Like other bisphosphonates, risedronate remains active on the surface of bone for long periods after dosing, providing the opportunity to develop a range of dosing schedules. The original risedronate dosing regimen for postmenopausal osteoporosis was an oral dose of 5 mg daily1,2,3. It was later demonstrated that regimens of 35 mg of risedronate, taken once a week, and 150 mg, taken once a month, provided similar efficacy and safety compared to the daily regimen in Caucasian subjects with osteoporosis4,5. However, the effects of 35 mg of risedronate once weekly have not been compared with those of 5 mg daily in Chinese patients. This study was conducted in a double-blind manner in Chinese subjects with involutional osteoporosis to compare the efficacy and safety of oral risedronate 35 mg once a week to 5 mg daily over a one-year period.
Materials and methods
Study design
This randomized, multicenter, double-blind, active-controlled, parallel-group, non-inferiority study was conducted at seven locations in China. A multicenter clinical evaluation recruited subjects at seven investigational sites: 1) Shanghai Jiao Tong University Affiliated Sixth People's Hospital; 2) Peking Union Medical College Hospital; 3) The Affiliated Drum Tower Hospital of Medical School, Nanjing University; 4) West China Hospital, Sichuan University; 5) General Hospital of People's Liberation Army Chengdu Military Region; 6) Tianjin Hospital; and 7) Beijing Shunyi Hospital, all located in China.
In this phase II clinical trial, the test drug and control drug were administered in the ratio of 1:1 based on the number of cases. Validity, non-inferiority, and one-sided tests [α=0.025, β=0.2 (efficacy=80%)] were used according to the literature 4. Risedronate Sodium tablets 5 mg and 35 mg were administered for the treatment of osteoporosis in postmenopausal women for 12 months. The main therapy lumbar spine bone mineral density (BMD) degree index increased by 4.00%±3.94% and 3.94%±3.96% in the 5-mg and 35-mg groups, respectively. The default public standard deviation (S) was 4%, and non-inferiority criteria was δ=1.5%, which indicates a public standard deviation of 1/3. The estimated sample size for each group to obtain appropriate results was 112. Based on the follow-up loss, the appropriate sample size for recruitment was 135 cases in the treatment group and 135 cases in the control group (a total of 270 cases).
The first subject was screened in July 2010, and the last subject observation occurred in July 2011. The study was performed in accordance with good clinical practices and the ethical principles from the Declaration of Helsinki. The protocol was approved by the appropriate institutional review boards or ethics committees, and the subjects gave written, informed consent to participate.
Patients
Inclusion criteria
Eligible subjects who gave consent were randomly assigned in a 1:1 ratio to the two treatment groups. Women were eligible to enroll in the study if they were between 50 and 80 years of age, ambulatory, in generally good health, and postmenopausal (at least 1 year since last menses). Their body mass indices (BMIs) were between 18 and 30. They had no severe lumbar anatomical abnormalities that could affect DXA bone densitometry, such as severe scoliosis.
BMD inclusion criteria were the following. (1) Osteopenia (a femoral neck, lumbar spine 1–4, or total hip BMD T-score between −1 and −2.5SD). They also had to meet at least one of the following two risk factors: advanced age (≥65 years) or more than 10 years since the last menses. The number of cases of osteopenia comprised one-third of the total number of patients. (2) Osteoporosis: a femoral neck, lumbar spine 1–4, or total hip BMD T-score of less than −2.5; a T-score of less than −1.0 at any of the three sites above and with at least one fragility fracture. If lumbar spine 1–4 fractures were present, BMD was calculated from the mean of the two adjacent, unfractured vertebral bones. Specific details of the inclusion criteria and methods have been previously published6,7.
Exclusion criteria
Study subjects who had serious heart disease, such as myocardial infarction, unstable angina pectoris, cardiac insufficiency, severe arrhythmia, or serious gastrointestinal diseases, such as reflux esophagitis or peptic ulcer, were excluded. A history of diabetes uncontrolled with medications and fasting blood glucose >7.0 mmol/L were also causes for exclusion. Moreover, serious organic diseases of the nervous and endocrine systems, disorders of the bones and joints, and other chronic diseases were disqualifiers. Additional exclusion criteria included high blood pressure >160/95 mmHg, even with antihypertensive drugs; liver enzyme levels 1.5 times the upper limits of normal for serum alanine transaminase (ALT) or serum aspartate aminotransferase (AST); serum creatinine >133 μmol/L; white blood cell count <3.5×109/L, or hemoglobin <100 g/L. Subjects who had used bisphosphonates, fluoride, or glucocorticoids in the preceding 12 months; estrogen, calcitonin, ipriflavone, selective estrogen receptor modulators, strontium salt, or active vitamin D in the preceding 6 months; Xianlinggubao, Gusongkang, or Qianggujiaonang in the preceding 3 months; or were allergic to bisphosphonates were not included.
Treatments
All subjects, in accordance with the table generated by software, were randomly assigned to the experimental group (35 mg of oral risedronate once a week) or control group (5 mg of oral risedronate daily). This method was used at all seven study locations. The study drug and the comparator drug were both produced by Kunming Jida Pharmaceutical Co, Ltd, Kunming, China. The weekly-group members took a single 35-mg tablet on the same calendar day each week and a placebo tablet daily; the daily-group members took a 5-mg tablet daily and a placebo tablet on the same calendar day each week; all the tablets were identical in appearance. The tablets were taken on an empty stomach in the morning at least 30 min before the first food or drink of the day, with at least 200 mL of plain water. The subjects were instructed to remain in an upright position for at least 30 min after administration. Subjects were considered compliant if they took at least 80% of the study tablets. One tablet per day of Calcichew D (GE Pharmaceutical Shanghai Co, Ltd), which contains 500 mg of element calcium and 200 IU of vitamin D3, was supplied to all the subjects. These supplements were taken with a meal other than breakfast and not with the study medication.
Efficacy assessments
DXA measurements of the lumbar spine and proximal femur were obtained at baseline and at 6 and 12 months using the following instruments: manufactured by GE, Madison, WI at site 1 (44 subjects); Hologic4500-W at site 2 (24 subjects); GE Lunar iDXA at site 3 (60 subjects); GE Lunar iDXA at site 4 (36 subjects); Hologic Discover at site 5 (26 subjects); GE Lunar Prodigy at site 6 (68 subjects); and GE Lunar Prodigy at site 7 (32 subjects). Lateral thoracic and lumbar spine radiographs were collected at screening and at 0 and 12 months and were then analyzed for vertebral fractures by semi-quantitative analysis8. Biochemical markers of bone turnover were assessed at baseline, 6, and 12 months. Serum N-terminal procollagen of type l collagen (P1NP) and beta C-terminal cross-linked telopeptides of type I collagen (β-CTX)9 were measured using an automated Roche electro-chemiluminescence system (Roche Diagnostic Gmbh). The intra- and interassay coefficients of variation (CVs) were 2.5% and 3.5% for β-CTX and 2.3% and 2.8% for P1NP, respectively. These bone-turnover-marker assays were stored at −80 °C and were performed at a central laboratory (ADICON Clinical Laboratory, China).
Safety assessments
The safety of the study drugs was assessed using reported adverse events (AEs) and abnormal laboratory test values. Physical examinations were performed at baseline and at 3, 6, 9, and 12 months. The subjects' vital signs, concomitant medications, and adverse event reports were recorded at regular clinic visits throughout the study. The following laboratory tests were performed at baseline and at 6 and 12 months of treatment in each center: hematology (red blood cell count, white blood cell count, hemoglobin, and platelet count), blood chemistry [fasting blood glucose (FBG), AST, ALT, total bile acid (T-BIL), alkaline phosphatase (ALP), blood urea nitrogen (BUN), serum creatinine (Cr), serum calcium (Ca), and serum phosphorus (P)], serum parathyroid hormone (PTH), and urinalysis (protein and glucose). Additionally, we performed an electrocardiogram (ECG) at baseline and at 12 months. Fractures in the upper or lower extremities reported by site investigators were also included.
Statistical analysis
The primary analysis comparing the efficacy of the two regimens (35 mg of risedronate once a week and 5 mg once daily) used the full analysis set (FAS) and the per protocol set (PPS). In the FAS analysis, the population is a trial population, which is as close as possible to the general population for which a test treatment is intended. The FAS population can include individuals who fail to comply with the treatment protocol. In the PPS analysis, patients with important protocol deviations were excluded from the analyses. A list of protocol violators was issued before unblinding the database. No missing data were imputed. Safety was evaluated in patients who received at least one dose of study drug in the treatment period. The statistical analyses were performed using SAS 9.2 software, except for the inferiority tests. Two-tailed tests were performed, and P values ≤0.05 were considered statistically significant. Changes in bone mineral density of lumbar vertebrae treatment rate of 12 months, baseline lumbar spine bone mineral density, height, and past medical history were entered in a covariate analysis of covariance (ANCOVA) and compared between groups. The calculation of the test group and the control group (LSMEAN) between the least square mean difference of bilateral 95% confidence intervals was conducted with a δ=1.5% non-inferiority test.
The primary endpoint analysis was a test of non-inferiority, comparing the least squares mean percent change from baseline in the lumbar spine BMD in the 35-mg once-a-week and 5-mg-daily groups after 12 months. This test employed a predefined non-inferiority margin of 1.5% and a one-sided type I error of 2.5%. The secondary endpoints included the percent changes from baseline in the BMDs of the total hip and the femoral neck at 12 months and the percent changes from baseline in biochemical markers of bone turnover (β-CTX and P1NP) at 6 and 12 months. All the data reported here are based on cumulative data collected over the entire 1-year treatment period.
Results
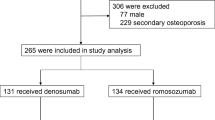
Subjects
The program enrolled 270 patients initially, and 290 patients for the actual enrollment. Of the 145 subjects in the weekly group (50%), the PPS analysis included 119 patients, and the FAS analysis included 145 patients. Of the 145 subjects in the daily group (50%), the PPS analysis included 115 patients, and the FAS analysis included 144 patients. One patient from the daily group did not take any study drugs, so she was not included in the statistical analysis. A total of 56 patients did not enter the PPS (26 patients from the weekly group and 30 patients from the daily group). The main reasons were AEs, lost medications, bad absorptiometry results (causing a missed primary efficacy endpoint), patients choosing to quit the study, exceeded BMI, ALT and AST levels outside of the inclusion criteria, and poor compliance. The two groups were not significantly different (P>0.05) in the numbers of cases that were disqualified for PPS. Concomitant medications were not significantly different between the two groups (P>0.05). High percentages of the subjects in both groups (82.8% of the subjects in the 35-mg-weekly group and 82.6% of the subjects in the 5-mg-daily group) took 80% to 120% of the study tablets. Overall, the baseline characteristics were similar in both treatment groups (Table 1).
Efficacy assessments
The mean percent changes from baseline in the lumbar spine BMD were statistically significant in both treatment groups. In the PPS analysis, the mean percent changes at 12 months (95% CI) were 4.87% (3.92%–5.81%) in the 35-mg-weekly group and 4.35% (3.31%–5.39%) in the 5-mg-daily group. The mean percent changes from baseline in the femoral neck BMD were also statistically significant in both treatment groups; in the PPS analysis, the mean percent changes at 12 months (95% CI) were 1.67% (0.79%–2.55%) in the 35-mg-weekly group and 2.74% (1.97%–3.51%) in the 5-mg-daily group. The mean percent changes from baseline in the total hip BMD were statistically significant in both treatment groups; in the PPS analysis, the mean percent changes at 12 months (95% CI) were 2.07% (1.38%–2.76%) in the 35-mg-weekly group and 2.26% (1.54%– 2.97%) in the 5-mg-daily group (Table 2). There were no statistically significant differences between the two treatment groups in terms of mean percent changes in BMD at the lumbar spine and total hip at any time point.
Significant decreases from baseline in P1NP and β-CTX were observed at 6 and 12 months in both treatment groups (P<0.05) (Figure 1). In the PPS analysis, the geometric mean percent changes at 6 months in the 35-mg-weekly group and 5-mg-daily groups were −55.3% and −59.7% for β-CTX (Figure 1A) and −55.6% and −59.5% for P1NP (Figure 1B), respectively. In general, changes from baseline in these biochemical markers were similar in both treatment groups. There was no significant difference between the treatment groups at the endpoint for any of the biochemical markers of bone turnover in either PPS or FAS.
Mean percent changes from baseline in (A) β-CTX and (B) P1NP for the PPS results. There were no statistically significant differences between the treatment groups at any time point at any of these sites. Mean±SEM. n=145 in 35 mg once weekly group. n=144 in 5 mg once daily group.
Safety assessments
The incidences of clinical AEs were 48.3% (70/145 patients) in the weekly group and 54.2% (78/144 patients) in the daily group, with no significant difference between the treatment groups (Table 3). The discontinuation rates due to clinical drug-related AEs in the weekly and daily groups were 6.9% (10/145 patients) and 5.6% (8/144 patients), respectively, with no significant difference between the treatment groups. Serious AEs were reported in 7 patients in the weekly group and in 5 patients in the daily group. Among these cases, two patients had serious AEs that were judged to be drug-related. One patient in the weekly group was hospitalized for a penetrating ulcer with esophageal hematoma formation after conservative treatment. An endoscopy showed light esophagitis and superficial gastritis with erosion. When she left the hospital, the symptoms disappeared without discomfort. Her case was not unblinded. A patient from the daily group was hospitalized for partial necrosis of the left mandible after a tooth extraction, and the symptoms disappeared after dental treatment without discomfort. Her case was unblinded. No patient had new fractures in either treatment group. No drug-related laboratory AEs occurred. No remarkable differences were observed between the two groups with regard to any of the safety parameters.
Discussion
This study was a prospective, 1-year study that compared two dosing regimens: 35 mg of risedronate once a week versus 5 mg daily. These 1-year data show that the 35-mg once-a-week dose produces clinical effects that are similar to those observed with the 5-mg-daily dose.
Risedronate, a third-generation pyridine bisphosphonate, acts primarily by inhibiting osteoclast-mediated bone resorption. Compared with the first and second generation bisphosphonates, this class of drug inhibits bone loss more effectively and plays a role in increasing bone mineral content. Regarding upper gastrointestinal AEs, which have been a major issue in the safety of bisphosphonate alendronate (and other related drugs), the incidence of gastrointestinal side effects in risedronate is significantly reduced compared with the previous two generations, and the weekly oral mode of administration has greatly improved patient compliance, making this medication truly safe, effective, and convenient10. The risk of developing a GI AEs was lower in patients who switched to risedronate compared with those who remained on alendronate11. In our study, the risk of developing a GI adverse event was similar between the two groups (12.4% in the 35-mg-weekly group and 11.8% in the 5-mg-daily group) and was lower compared with the findings of studies conducted in Western countries. In Brown's study, the risk of developing a GI AEs was 18.4% in the 35-mg-weekly group and 17.5% in the 5-mg-daily group4.
Specifically, the mean percent change in the lumbar spine BMD at 12 months in the monthly group was non-inferior to the mean percent change in the lumbar spine BMD in the daily group. In the PPS analysis, the mean percent changes at 12 months (95% CI) were 4.87% (3.92%–5.81%) in the 35-mg-weekly group and 4.35% (3.31%–5.39%) in the 5-mg-daily group. These results parallel Brown's research4, which revealed mean percent changes in the lumbar spine BMD of 3.9% in the 35-mg group and 4.0% in the 5-mg-daily group at 12 months.
Changes in the secondary efficacy parameters, including the BMD at the hip and the serum levels of bone turnover markers at the endpoint, were also similar in both groups. The mean percent changes from baseline in the total hip and the femoral neck BMD were statistically significant in both treatment groups. In the PPS analysis, the mean percent changes at 12 months (95% CI) were 1.67% (0.79%–2.55%) in the 35-mg-weekly group and 2.74% (1.97%–3.51%) in the 5-mg-daily group. This outcome is also similar to Brown's work4. In their research, the mean percent changes in BMD at 12 months, measured at the total hip and the femoral neck, were 2.35% and 1.98% in the 35-mg-weekly group and 2.51% and 2.05% in the 5-mg-daily group, respectively. Statistically significant differences between the treatment groups were observed for the two bone turnover markers at month 6 but did not persist to month 12. No significant differences between the groups were observed for any marker at either month 6 or month 12.
The risedronate 35-mg once-a-week dose was well tolerated over 1 year, with a safety profile similar to that observed with the 5-mg-daily regimen. No patient had new fractures in either of the treatment groups. The low incidences of subjects with vertebral and nonvertebral clinical fractures were similar between groups and were consistent with rates previously observed with the 5-mg-daily dose1,2,3.
Additionally, these results are consistent with the favorable tolerability and efficacy profiles observed in large placebo-controlled clinical trials of the risedronate 5-mg-daily regimen1,2,3. The findings are also consistent with previous studies of less frequent dosing with risedronate. Such studies demonstrated that the treatment effects of risedronate 35 mg taken weekly, of 75 mg taken on two consecutive days each month, and of 150 mg taken once a month were similar to the effects of daily dosing4,5,12.
A limitation of this study was the open-label design which may have introduced bias. Additionally, although BMD was measured by either Hologic (HOLOGIC Corporation) or GE Lunar (GE Medical Systems) DXA machines and individual sites followed quality-control procedures recommended by the manufacturers, there was no independent central BMD quality-control/quality-assessment program. However, because the study was not large enough to compare fracture incidence, the central adjudication of events such as fractures was not performed by either an internal or an external committee.
Risedronate 35 mg once a week taken for 1 year is non-inferior in efficacy and tolerability to the 5-mg-daily dosing regimen that had previously been proven to reduce the incidence rates of vertebral and nonvertebral fractures. The addition of this dosing regimen to the therapeutic armamentarium will provide Chinese women with postmenopausal osteoporosis with a greater variety of risedronate oral dosing options, from daily to weekly.
Author contribution
Zhen-lin ZHANG, Li WANG, Hua LIN, De-cai CHEN, Hai TANG, Xiao-lan JIN, and Wei-bo XIA designed research; Jiemei GU, Li WANG, Hua LIN, De-cai CHEN, Hai TANG, Xiaolan JIN, Wei-bo XIA, Yun-qiu HU, Wen-zhen FU, Jin-wei HE, Hao ZHANG, Chun WANG, Hua YUE, Wei-wei HU, Yujuan LIU, and Zhen-lin ZHANG performed research; Zhen-lin ZHANG contributed analytical tools and reagents; Jie-mei GU analyzed data; Jie-mei GU wrote the paper.
References
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA 1999; 282: 1344–52.
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 2000; 11: 83–91.
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 2001; 344: 333–40.
Brown JP, Kendler DL, McClung MR, Emkey RD, Adachi JD, Bolognese MA, et al. The efficacy and tolerability of risedronate once a week for the treatment of postmenopausal osteoporosis. Calcif Tissue Int 2002; 71: 103–11.
McClung MR, Zanchetta JR, Racewicz A, Roux C, Benhamou CL, Man Z, et al. Efficacy and safety of risedronate 150-mg once a month in the treatment of postmenopausal osteoporosis: 2-year data. Osteoporos Int 2013; 24: 293–9.
Kanis JA . Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int 1994; 4: 368–81.
Yue H, He JW, Zhang H, Wang C, Hu WW, Gu JM, et al. Contribution of myostatin gene polymorphisms to normal variation in lean mass, fat mass and peak BMD in Chinese male offspring. Acta Pharmacol Sin 2012; 33: 660–7.
Genant HK, Wu CY, van Kuijk C, Nevitt MC . Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993; 8: 1137–48.
Zhang H, Huang QR, Gu JM, Hu WW, Liu YJ, Hu YQ, et al. Comparison of the effects of cholecalciferol and calcitriol on calcium metabolism and bone turnover in Chinese postmenopausal women with vitamin D insufficiency. Acta Pharmacol Sin 2012; 33: 490–5.
Thomson AB, Marshall JK, Hunt RH, Provenza JM, Lanza FL, Royer MG, et al. Forteen day endoscopy study comparing risedronate and alendronate in postmenopausal women stratified by Helicobacter pylori status. J Rheumatol 2002; 29: 1965–74.
Ralston SH, Kou TD, Wick-Urban B, Steinbuch M, Masud T . Risk of upper gastrointestinal tract events in risedronate users switched to alendronate. Calcif Tissue Int 2010; 87: 298–304.
Delmas PD, Benhamou CL, Man Z, Tlustochowicz W, Matzkin E, Eusebio R, et al. Monthly dosing of 75 mg risedronate on 2 consecutive days a month: efficacy and safety results. Osteoporos Int 2008; 19: 1039–45.
Acknowledgements
This study was sponsored by Kunming Jida Pharmaceutical Co, Ltd, Kunming, China.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Gu, Jm., Wang, L., Lin, H. et al. The efficacy and safety of weekly 35-mg risedronate dosing regimen for Chinese postmenopausal women with osteoporosis or osteopenia: 1-year data. Acta Pharmacol Sin 36, 841–846 (2015). https://doi.org/10.1038/aps.2015.30
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2015.30
Keywords
This article is cited by
-
Development of UV Spectrophotometric Methods for the Determination of Risedronate Sodium in Different Solutions
Journal of Applied Spectroscopy (2021)