Abstract
The current study evaluated the efficacy and safety of a denosumab biosimilar, QL1206 (60 mg), compared to placebo in postmenopausal Chinese women with osteoporosis and high fracture risk. At 31 study centers in China, a total of 455 postmenopausal women with osteoporosis and high fracture risk were randomly assigned to receive QL1206 (60 mg subcutaneously every 6 months) or placebo. From baseline to the 12-month follow-up, the participants who received QL1206 showed significantly increased bone mineral density (BMD) values (mean difference and 95% CI) in the lumbar spine: 4.780% (3.880%, 5.681%), total hip :3.930% (3.136%, 4.725%), femoral neck 2.733% (1.877%, 3.589%) and trochanter: 4.058% (2.791%, 5.325%) compared with the participants who received the placebo. In addition, QL1206 injection significantly decreased the serum levels of C-terminal crosslinked telopeptides of type 1 collagen (CTX): −77.352% (−87.080%, −66.844%), and N-terminal procollagen of type l collagen (P1NP): −50.867% (−57.184%, −45.217%) compared with the placebo over the period from baseline to 12 months. No new or unexpected adverse events were observed. We concluded that compared with placebo, QL1206 effectively increased the BMD of the lumbar spine, total hip, femoral neck and trochanter in postmenopausal Chinese women with osteoporosis and rapidly decreased bone turnover markers. This study demonstrated that QL1206 has beneficial effects on postmenopausal Chinese women with osteoporosis and high fracture risk.
Similar content being viewed by others
Introduction
Osteoporosis is a well-known risk factor for brittle fracture, which is a major cause of mortality and morbidity in elderly people [1, 2]. Postmenopausal osteoporosis is a major health problem that has a prevalence of 40.1% in the Chinese population [3]. Gao et al. reported that the prevalence of vertebral fracture among elderly females in Shanghai, China, was 17.3% and that the prevalence increased with age [4]. Xia et al. [5] observed that, from 2002 to 2006, hip fracture rates increased 58% among women over the age of 50 years in Beijing, China. There is an urgent need to find better anti-osteoporotic drugs to treat postmenopausal women in China.
Clinical evidence indicates that receptor activator of nuclear factor κB ligand (RANKL) is closely related to bone loss that results in skeletal fragility and fracture [6]. Denosumab, a fully human monoclonal antibody against RANKL, is an agent that is widely used to decrease the number and activity of osteoclasts [7]. In the pivotal 3-year-Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Months (FREEDOM) study, a subcutaneous injection of 60 mg denosumab every 6 months significantly increased bone mineral density (BMD); reduced bone turnover markers; and reduced new vertebral fractures by 68%, hip fractures by 40%, and non‑vertebral fractures by 20% compared with placebo [8]. After the extension of the 7-year-FREEDOM trial, denosumab treatment for up to 10 years was found to be related to steadily continuing increases in BMD, decreased fracture incidence and low rates of adverse events [9].
To date, there have been no reports on the efficacy and safety of denosumab in postmenopausal Chinese women. The current study (ClinicalTrials.gov identifier: NCT04128163; study number: QL1206-004) compared the efficacy and safety of the denosumab biosimilar QL1206 (60 mg) to that of placebo in postmenopausal Chinese women with osteoporosis and high fracture risk.
Materials and methods
Study design
This is a multicentre, randomized, double-blind, placebo-controlled Phase III clinical study. Qualified subjects were randomly divided between the experimental group and the control group at a ratio of 3:1. Subjects entered the study phase after being enrolled and randomized. This study was a double-blind design, in which all subjects, study supervisors and data analysts remained blind. Central randomization was adopted in the experiment. The researcher logged into the random system to input the basic information of qualified subjects and obtain the random number and drug number of the subjects to complete the grouping. The QL1206 and placebo have the same inner and outer packaging, and the appearance of the two is basically the same in order to maintain blind state. A total of 455 postmenopausal women from 31 study centers in China were randomly assigned to receive denosumab (60 mg subcutaneously every 6 months) or placebo from April 2019 to July 2021 (ClinicalTrials.gov identifier: NCT04128163; study number: QL1206-004). All subjects took daily oral supplements containing elemental calcium (500 mg) and vitamin D (400 IU). The primary endpoint was the percentage change in the BMD of the lumbar spine at 12 months. The secondary endpoint was the BMD of the lumbar spine at 6 months; the 6- and 12-month percentage changes in the BMD of the total hip, femoral neck, and trochanter were also assessed, as were the serum levels of serum C-terminal crosslinked telopeptides of type 1 collagen (CTX) and N-terminal procollagen of type l collagen (P1NP). All X-rays and BMD measurements were reviewed independently by Paraxel China Jingding Pharmaceutical Research & Development (Shanghai) Limited Company. The measurement of the bone turnover markers CTX and P1NP was performed centrally by a third-party laboratory (Guangzhou Jinyu Medical Laboratory Group Co. Ltd), and the samples were sent through-cold chain transportation. CTX was measured using a Cross Laps kit (from Immunodiagnostic Systems Limited) and a Tecan Sunrise microplate reader and detected by an enzyme-linked immunosorbent assay. P1NP was measured using a total P1NP kit (from Roche Diagnostics) and a Roche automatic biochemical immunity analyser (Cobas 8000 e602) and detected by electrochemiluminescence. The intra-assay coefficients of variation were 7.9% and 1.7% for CTX and P1NP, respectively.
The date when the first subject signed informed consent was June 21, 2019, and the last subject visit took place on June 22, 2021. The study was conducted according to Good Clinical Practice and the ethical principles of the Declaration of Helsinki. The study protocol was approved by the institutional review boards of all the study sites, and written informed consent was obtained from all subjects.
Study participants
Inclusion criteria
Postmenopausal Chinese women aged 50–85 years (inclusive) were eligible if they could walk on their own and had a BMD T score of −2.5 to less than −4.0 (−4.0 < T ≤ −2.5) at the lumbar spine or total hip. Menopause was defined as spontaneous amenorrhoea or bilateral ovariectomy occurring after 40 years of age; postmenopause was considered to begin 2 years after menopause. Subjects were eligible only if they were postmenopausal on the date when they signed informed consent. If bilateral ovariectomy status was unknown, follicle-stimulating hormone (FSH) levels greater than 40 mIU/mL were used to confirm surgical menopause status. In this study, a high risk of fracture was defined as applying to postmenopausal women with low BMD (−4.0 < T ≤ −2.5) in the lumbar spine or total hip and at least one of the following risk factors: (1) a previous history of brittle fracture (occurring after 40 years of age); (2) a history of hip fracture in either parent; (3) a low body mass index (BMI), i.e., ≤19 kg/m2; (4) advanced age (≥65 years old); or (5) current smoking.
Exclusion criteria
Exclusion criteria included diseases that may affect bone metabolism, such as osteomalacia, osteogenesis imperfecta, Paget’s disease of bone, Cushing syndrome, hyperprolactinaemia; current hyperparathyroidism or hypoparathyroidism, hyperthyroidism or hypothyroidism; rheumatoid arthritis; malabsorption syndrome or any of the gastrointestinal disorders associated with malabsorption; severe renal impairment (creatinine clearance (Ccr) <30 mL/min); liver disease, such as cirrhosis, unstable liver disease, or biliary tract abnormalities known or determined by the investigator to be clinically significant; vitamin D deficiency: 25(OH) D concentration <20 ng/mL; oral and dental diseases, including past or current evidence of osteomyelitis or osteonecrosis of the mandible; active or uncontrollable infections requiring systematic treatment within 14 days prior to initial administration; and type 1 diabetes or type 2 diabetes beyond the control of drug therapy (patients using treatment drugs such as insulin, glucagon-like peptide (GLP) − 1 and thiazolidinedione were not eligible). Other exclusion criteria included the use of intravenous bisphosphonates, fluoride or strontium within the last 5 years; oral bisphosphonates (used for at least 3 years, or used for less than 3 years but more than 3 months, with the last use occurring <1 year before the signing of informed consent); use of drugs affecting bone metabolism in the last 6 weeks [parathyroid hormone (PTH) or PTH derivatives, such as teriparatide; anabolic hormones or testosterone; glucocorticoids (equivalent to more than 5 mg of prednisone daily for more than 10 days); sex hormone replacement therapy; selective oestrogen receptor modulators (SERMs), such as raloxifene; calcitonin, calcitriol and other active vitamin D (for calcitriol and other active vitamin D, no use within 4 weeks prior to signing informed consent was permitted)]; use of other bone-active drugs, such as anticonvulsants (other than benzodiazepines) or heparin; and long-term systemic use of ketoconazole, adrenocorticotropic hormone (ACTH), cinacalcet, aluminum, lithium, protease inhibitors, methotrexate, gonadotropin-releasing hormone agonists, insulin, GLP-1 receptor agonists, or thiazolidinediones. Additional exclusion criteria included abnormal blood calcium [current hypocalcaemia or hypercalcaemia, with calcium or albumin-corrected serum calcium ≤2.0 mmol/L (8.0 mg/dL) or ≥2.9 mmol/L (11.5 mg/dL)]; serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) ≥2.0 times the upper limit of normal (ULN); alkaline phosphatase or total bilirubin ≥1.5 ULN; a case in which lumbar BMD could not be accurately measured; a very high risk of fracture determined by the investigator to require active drug treatment; previous or current malignancy (other than completely excised cutaneous basal cell in situ or cutaneous squamous cell carcinoma, cervical carcinoma in situ or ductal carcinoma in situ of the breast); biological abnormalities (a variety of physical or mental diseases and clinically significant laboratory abnormalities that the investigator believes will affect the subjects’ ability to complete the study or interfere with the study results); drug or alcohol abuse; participation in other medical device or drug trials concurrently or within the last 30 days or 5 times the drug half-life; and allergy to mammalian cell-derived products or denosumab.
Study procedures
Subjects underwent a screening period from 2.5 months before drug administration to 1 day before drug administration (D-1). The main screening tests included disease history, medication history, drug allergy history, smoking history, demographic data, medical examination (including oral cavity), vital signs (blood pressure, heart rate), a 12-lead electrocardiogram (ECG) and clinical laboratory examination, blood biochemistry, blood routine, urine routine and coagulation routine, four blood transfusion tests, detection of parathyroid hormone, thyroid function, 25(OH)D levels, and spine vertebral fractures were assessed by lateral X-ray. Measurements of BMD of the lumbar spine, total hip, trochanter and femoral neck were performed by dual-energy X-ray absorptiometry (DXA) (GE Lunar or Hologic) at baseline and at 6 and 12 months. Since the data are expressed as percentage changes from every patient’s baseline, cross calibration of the DXA machines was unnecessary. This is standard practice for BMD examination in protocols [8, 10, 11]. During the research process, instrument quality control (IQC) was performed using independent review committee (IRC) for all instruments in the research center. The permissible range of IQC scanner is that the coefficient of variance could be more or less than 1.5%.
Eligible subjects will be randomly assigned to the QL1206 or placebo group and given QL1206 1 mL (60 mg) or 1 mL placebo subcutaneously at D1 based on the randomized results, followed by 1 injection at intervals of 6 months. Serum CTX, P1NP, immunogen and QL1206 blood samples were collected according to the protocol requirements. Serum CTX and P1NP blood samples were collected at baseline and at 1, 6 and 12 months.
Immunogenicity blood samples were collected at baseline and at 6, 9, and 12 months. Blood samples will be tested for anti-drug antibodies (ADAs), and those who are ADA-positive will be tested for neutralizing antibodies (Nabs). In this study, ADA positivity was defined as follows. A signal value greater than or equal to the critical point defined for screening was considered a positive ADA screen. An inhibition rate greater than or equal to the confirmatory critical point was considered a confirmatory positive ADA test. However, McClung et al. [7] defined a positive ADA test as one in which the signal value after administration is greater than 2 times the signal value before administration. Denosumab pharmacokinetics (PK) of the blood sample were collected to support population pharmacokinetic and exposure–response (dose–response) analysis. Blood samples were collected at baseline and at 1, 3, 9, and 12 months.
During the trial, necessary efficacy and safety evaluations should be carried out according to the protocol. The investigator considers it necessary to decide whether the subjects were terminated from the study from the perspective of medical ethics, for example (not limited to the following situations): (1) Osteoporosis-related fractures (vertebral fractures, hip fractures, etc.); (2) A significant decrease in BMD requiring a change of treatment: a confirmed decrease in the BMD of the femoral neck by >7% after treatment, or in the BMD of the total hip or lumbar vertebrae by >6%; and any new malignancy (other than basal cell carcinoma, cervical carcinoma in situ or ductal carcinoma of the breast).
Statistical analysis
We hypothesized that QL1206 was more effective than placebo in postmenopausal women with osteoporosis who were at increased risk of fracture. We assumed that the difference in the rate of change in lumbar BMD from baseline between the QL1206 group and the placebo group at 12 months of treatment is 4.4%, the standard deviation (SD) is 4, and the certainty is 90%; we selected α = 0.05 (bilateral), and the ratio of patients assigned to the QL1206 group and the placebo group is 3:1. Based on these assumptions, we calculated the necessary sample size using PASS16.0; we found that the minimum sample sizes of the QL1206 group and the placebo group are 39 cases and 13 cases, respectively. Assuming a dropout rate of approximately 10%, a minimum of 60 cases were needed to meet the statistical requirements of efficacy. According to the requirements of regulatory authorities and the number of cases required for therapeutic biologics in the Drug Registration Administration Measures, at least 300 subjects are required for a Phase III trial group. As the size ratio between the QL1206 group and the placebo group was 3:1 and a 10% dropout rate was assumed, 330 subjects in the QL1206 group and 110 in the placebo group were required to be enrolled, and a total of 440 subjects were required for the two groups. The study was a merit design, so the experimental group (QL1206) was considered superior to the control group (placebo) as long as the lower limit of the bilateral 95% CI of the result-control difference was greater than 0.
Normally distributed data are shown as the mean ± SD. Data that were not normally distributed are shown as the median (interquartile range). Student’s t test was used for normal data, the Wilcoxon rank sum test was used for non-normal data, and the chi-square test was used for percentages. The primary endpoint analysis was performed using the percentage change in lumbar BMD between the two groups from baseline to 12 months using an analysis of covariance model that adjusted for BMD at baseline. Based on the model, the least-squares mean, least-squares median difference, and 95% CI of the corresponding P value, standard error, and difference were estimated for the two groups.
Secondary endpoints were percentage changes in lumbar BMD from baseline to 6 months in both groups and percentage changes in hip, femoral neck, and trochanteric bone mineral density from baseline to 6 and 12 months in both groups using covariance identical to primary outcome measures. The percentage changes in secondary endpoints of serum CTX and P1NP from baseline to 6 and 12 months were analysed by the Wilcoxon rank sum test. The Hodges–Lehmann estimator was used to estimate the median and 95% CI. In addition, we analysed the percentage changes in serum calcium and phosphorus concentrations from baseline to 1, 6, and 12 months using the same statistical method.
Adverse events (AEs) will be coded and graded using the Regulatory Activity Medical Dictionary (MedDRA). The incidence, number and incidence of all AEs, drug-related AEs, severe AEs (SAEs), and AEs causing dropout were summarized and described. The group description summarizes vital sign data at each time point, including the values of each visit and their changes from baseline.
All completed examinations and descriptive statistics were compiled in the form of a cross-tabulation that listed physical examination, electrocardiogram, and laboratory examination indicators (according to the clinician’s judgment) at each visit before and after treatment. Immunogenicity was defined in terms of the incidence of ADA and Nab positivity.
Results
Subjects
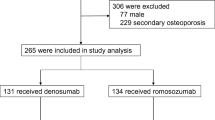
Data were collected from April 2019 to July 2021. Four hundred eighty (480) of the 935 subjects failed screening. The reasons for screen failures were failure to meet the inclusion/exclusion criteria (339 subjects), subject withdrawal of consent (139 subjects), and other reasons (2 subjects). A total of 455 subjects were enrolled, and 425 (93.4%) completed 12 months of treatment. A total of 337 subjects were in the QL1206 group, including 324 (96.1%) subjects who completed the study and 13 (3.9%) subjects who withdrew/terminated the study. The main reasons for loss to follow-up included withdrawal of informed consent (7 subjects, 2.1%). A total of 118 subjects were in the control group, including 101 (85.6%) subjects who completed the study and 17 (14.4%) subjects who withdrew/terminated the study. The main reasons for loss to follow-up included decreased BMD meeting the withdrawal criteria specified in the study (9 subjects, 7.6%) and withdrawal of informed consent (3 subjects, 2.5%). As 1 subject in QL1206 group and 3 subjects of the placebo group dropped out of the study after randomization without receiving the investigational product. These 4 subjects lacked post-dosing safety and efficacy data and were excluded from the safety data set. So QL1206 included 336 subjects who received investigational products, of which 329 (97.92%) completed two doses and 7 (2.08%) completed one dose. In the placebo group, 115 subjects received investigational products, of which 102 (88.70%) completed two doses and 13 (11.30%) received one dose. The overall compliance was good.
Baseline demographics were similar in the two treatment groups (Table 1). Demographic information of the two groups was similar in age, ethnicity, weight, height and BMI. Additionally, history of alcohol abuse, drug abuse, smoking, duration of menopause, brittle fractures after 40 years of age, parental hip fractures, baseline lumbar bone mineral density, baseline 25(OH)D concentration, were similar between the two groups (Table 1). Although the age and the duration of menopause in QL1206 group were statistically significant less compared with the control group, the actual data were similar and there was no significant difference in BMD, so the clinical significance was not significant. The concomitant diseases including diabetes and osteoarthritis in QL1206 group were statistically significant less compared with the control group. However, these two diseases have little relation with the efficacy of drugs for osteoporosis, nor are they stratified factors for drug treatment of osteoporosis, so their clinical significance is not significant either.
Efficacy
As 1 subject in QL1206 group and 3 subjects of the placebo group dropped out of the study after randomization without receiving the investigational product, another 1 patient in QL1206 group who received investigational product but baseline independent review committee data were missing for efficacy evaluation was excluded from the efficacy analysis, there were a total of 335 subjects in the full analysis set (FAS). QL1206 (n = 335) treatment was associated with a mean increase in BMD at the lumbar spine of 5.298% at 12 months, compared with a 0.518% in the placebo group (n = 115), and a statistically significant treatment difference of 4.780% (95% CI: 3.880%, 5.681%) (P < 0.001) was seen between the QL1206 and placebo groups for the primary endpoint (Fig. 1).
For the secondary endpoints, QL1206 treatment increased BMD levels at all sites measured at months 6 and 12 and reduced CTX and P1NP at months 1, 6, and 12. At month 6, QL1206 demonstrated a treatment-related difference compared with placebo for the mean percent change in BMD for the lumbar spine [median difference: 3.299% (95% CI: 2.440%, 4.158%)], total hip [2.822% (95% CI, 2.097%, 3.546%)], femoral neck [2.102% (95% CI, 1.296%, 2.907%)], and trochanter [3.171% (95% CI, 2.004%, 4.338%)] (all; P < 0.001), respectively. At month 12, QL1206 demonstrated a treatment difference compared with placebo for the mean percent change in BMD for the total hip [3.930% (95% CI, 3.136%, 4.725%)], femoral neck [2.733% (95% CI, 1.877%, 3.589%)] and trochanter [4.058% (95% CI, 2.791%, 5.325%)] (all P < 0.001) (Fig. 2). At months 1, 6, and 12, QL1206 demonstrated a treatment-related difference compared with placebo for the median percent change in CTX [−82.901% (95% CI, −89.945%, −76.844%)], [−72.566% (95% CI, −80.978%, −64.174%)], [−77.352% (95% CI, −87.080%, −66.844%)] (all P < 0.001), respectively; and P1NP [−21.017% (95% CI, −24.747%, −17.333%)], [−53.345% (95% CI, −58.765%, −48.369%)], [−50.867% (95% CI, −57.184%, −45.217%)] (all P < 0.001), respectively (Fig. 3).
Adverse events and safety
QL1206 was well tolerated throughout the 12 months. There were no events of death, atypical femoral fracture (AFF) or osteonecrosis of the jaws (ONJ), and no unexpected safety signals. A total of 1074 treatment-emergent adverse events (TEAEs) occurred in 273 subjects (81.3%), including 9 severe TEAEs that occurred in 8 subjects (2.4%) in the QL1206 group, and 93 subjects (80.9%) in the placebo group had 362 TEAEs, including six severe TEAEs that occurred in five subjects (4.3%). No significant differences were observed between the profiles of TEAEs in the QL1206 group and those in the placebo group (Table 2). All severe TEAEs were unrelated to the study drug, and the outcome of all SAEs was recovery, improvement, or follow-up to a stable state. The incidence of moderate TEAEs associated with the investigational drug was slightly higher in the QL1206 group than in the placebo group. A total of 20 subjects in the study had 27 moderate TEAEs related to the study drug (none of them severe), with an incidence rate of 4.4%. There were 18 subjects (5.4%) in QL1206 and 2 subjects (1.7%) in placebo who had 23 episodes of moderate TEAEs related to the study drug. The common types and incidence rates are recorded in Table 2.
As denosumab causes a decrease in serum calcium and phosphorus, we compared the changes in serum calcium and phosphorus in the QL1206 group and the control group. As shown in Fig. 3, serum calcium and phosphorus were lowest in the first month after the use of QL1206, with significant decreases of median percent change [−3.3% (95% CI, −4.2%, −2.5%)] and [−11.2% (95% CI, −13.5%, −8.9%)], respectively, compared with the control group (all P < 0.001). At month 6, serum calcium and phosphorus returned to [−1.8% (95% CI, −2.7%, −0.9%)] and [−6.5% (95% CI, −9.1%, −3.8%)], respectively, compared with the control group (all P < 0.001) and remained relatively stable thereafter. In TEAEs, the incidence of hypocalcaemia and hypophosphataemia was 4.8% and 3.9% in the QL1206 group and 1.7% and 0.9% in the placebo group, respectively. As determined by the investigators, the incidence of hypocalcemia and hypophosphatemia associated with the study drug was 4.5% and 3.3% in the QL1206 group and 1.7% and 0.9% in the placebo group, respectively. There were no SAEs related to hypocalcaemia and hypophosphataemia in this study.
A total of 36 subjects were tested positive for ADA in the QL1206 group (10.7%). There were 3 (0.9%), 11 (3.3%), 17 (5.1%) and 9 (2.7%) ADA-positive patients in the QL1206 group at baseline and 6, 9 and 12 months, respectively. Only 2 (0.6%) ADA-positive subjects at the 9th month were Nab-positive, and all other ADA-positive subjects were Nab-negative. There was no ADA positivity at any visit in the placebo group. Three treatment-emergent SAEs (TESAEs) occurred in three ADA-positive subjects (8.3%) in the QL1206 group, including posterior circulation ischemia due to insufficient vertebrobasilar artery supply, an age-related cataract in the left eye and a comminution fracture of the left lateral malleolus. The investigators judged that these SAEs might not be related to the drug. None of the ADA-positive patients developed TEAEs that resulted in permanent discontinuation of the study drug or TEAEs that resulted in death. Data analysis and population pharmacokinetics (PopPK) model analysis were conducted on the safety, PK and pharmacodynamics (PD) of the antibody-positive subjects and demonstrated that ADA had no effect on the subjects; thus, ADA positivity had no obvious clinical significance.
Discussion
This study was a prospective, 1-year, multicentre, randomized, double-blind, placebo-controlled study reported on the effects of the denosumab biosimilar QL1206 in postmenopausal Chinese women with osteoporosis. These 1-year data showed that QL1206 was safe and effective in increasing BMD at the lumbar spine and hip and decreasing bone turnover markers (CTX and P1NP) in postmenopausal Chinese women.
Denosumab is a novel drug that blocks the formation, function, and survival of osteoclasts because it prevents the interaction of RANKL with RANK, the receptor on osteoclasts and their precursors [12]. In a 3-year FREEDOM trial, denosumab showed broad-spectrum antifracture efficacy, including a reduced risk of new radiographic vertebral fracture, hip fracture and non-vertebral fracture of 68%, 40%, and 20%, respectively [8]. Studies of denosumab treatment with a duration extended to 10 years showed that the incidence of new-onset vertebral fractures per year remained low during extension, while non-vertebral fractures further significantly decreased from year 4 and remained stable thereafter [9, 13]. Denosumab also significantly reduced the risk of new or worsening vertebral fracture by 65.7% in postmenopausal Japanese women and Japanese men with osteoporosis after 24 months of treatment [14]. Denosumab has been regarded as one of the most commonly used agents and could be considered an initial option for most osteoporosis patients in many guidelines for the diagnosis and treatment of postmenopausal osteoporosis [15, 16]. In 2014, a multicentre randomized placebo-controlled trial of denosumab was conducted in China (NCT02014467, https://www.clinicaltrials.gov/ct2/show/study/NCT02014467?term=A+twelve-month+randomized%2C+double-blind%2C+placebo-controlled%2C+parallel-group%2C+multicenter+study+to+evaluate+the+efficacy+and+safety+of+denosumab+in+Chinese+postmenopausal+women+with+osteoporosis+at+increased+risk+of+fracture&draw=2&rank=1), but for a variety of reasons, this study has not been reported in the literature.
Therefore, there is an urgent need to report the efficacy and safety of denosumab or denosumab biosimilar for osteoporosis in postmenopausal women in China.
Previously, QL1206 was found to exhibit similar PK and PD characteristics to Xgeva® (denosumab 120 mg) in a Phase I, randomized, single-dose study [17]. The present study in postmenopausal Chinese women with low BMD and high fracture risk demonstrated that the treatment of QL1206 was associated with a mean 12-month increase in the BMD of the lumbar spine by 5.298% compared with baseline, and a 4.780% increase versus placebo was seen for the primary endpoint. This result is similar to that of a study in South Korea showing a continuing increase in the BMD of the lumbar spine for up to 12 months, reaching 5.6% [11]. Likewise, the Japanese study suggested that 60 mg denosumab treatment produced a significant 6.73% increase in lumbar spine BMD from baseline to 12 months [18], similar to the results of the study by McClung et al. in which denosumab treatment was associated with a mean lumbar spine BMD increase of 3.0% to 6.7% at 12 months [7]. In fact, there was a significant increase in lumbar BMD as early as 6 months in our study. QL1206 treatment was associated with a mean increase in the BMD of the lumbar spine, with a statistically significant treatment-related difference of 3.299% compared with the placebo group. These results are similar to many other trials including other Asian subjects as well as Caucasians subjects [7, 11, 18, 19]. The mean percent changes from baseline in the total hip, femoral neck and trochanter BMD in our study were also statistically significant. At month 6, our study demonstrated a treatment difference compared with placebo for the mean percent change in BMD for the total hip 2.822%, femoral neck 2.102% and trochanter 3.171%. In a Korean study [11], at month 6, denosumab was associated with the following BMD differences compared with placebo: 1.7% for the total hip, 1.4% for the femoral neck, and 2.0% for the trochanter. And in an Indian study [19], the denosumab group had median differences of 1.7%, 2.3% and 1.8% from the placebo group in terms of total hip, femoral neck, and trochanter BMD, respectively. In our study, the median differences of percentage BMD change between the QL1206 group and the placebo group at month 12 in the total hip, femoral neck and trochanter were 3.930%, 2.733%, and 4.058%, respectively. Similarly, the mean percent increase in the BMD of the total hip from baseline to 12 months was 3.09% for 60 mg denosumab in a study from Japan [18], and McClung et al. [7] observed that the BMD of the total hip at 12 months increased by a mean of 1.9% to 3.6% in the denosumab groups.
Our results showed that the bone turnover marker CTX decreased 82.901% in the QL1206 group at 1 month, which was the greatest decline at any of our timepoints; similarly, in the FREEDOM study, bone resorption was reduced by a median of 86% at 1 month [8]. McClung et al. [7] discovered that the denosumab groups showed decreases in serum CTX levels as early as 3 days and reached the maximum decline at 1 month. Although we did not examine CTX at 3 days, the rapid decline at one month indicates the rapid action of the drug. The decrease in CTX was sustained at months 6 and 12. Our study showed that the P1NP levels of the QL1206 group were significantly decreased at month 6, when this variable reached its maximum decline compared to the placebo group. The delayed decrease in P1NP concentration suggests that denosumab acts primarily to inhibit bone resorption, after which coupling between bone formation and resorption secondarily reduces bone formation. A similar time difference was observed in other Asian populations as well as Caucasian populations [7, 8, 11, 18, 20, 21]. Eastell et al. [21] discovered a significant correlation between CTX reduction with denosumab and the increase in BMD. The postmenopausal women with osteoporosis who received denosumab in the FREEDOM extension trial, for up to 10 years remained consistent over time, with sustained reduction of bone turnover, continued gains in BMD and low fracture incidence [9].
A 1-year course of treatment of QL1206 was well tolerated among postmenopausal Chinese women in this study. The overall detection rates of AEs and SAEs were similar between the QL1206 group and the placebo group, and none of the SAEs was related to treatment. The incidence of moderate TEAEs was slightly elevated in the QL1206 group, including upper respiratory tract and urinary tract infections and allergic dermatitis; these observations were consistent with previous research [9, 18]. The decreases in serum calcium, alkaline phosphatase and phosphorus were mild and consistent with known effects of QL1206 on bone, as in a previous study [8, 18]. In the FREEDOM trial, the incidence of some low-frequency events (rash and cellulitis, SAEs associated with infection) was slightly elevated in the denosumab group [8]. In the 10-year extended FREEDOM trial [9], 2 atypical femoral fractures occurred, and 13 cases of osteonecrosis of the jaw were reported. In the present study, cellulitis, atypical femoral fracture and osteonecrosis of the jaw were not found.
In this study, we reported that a total of 10% of subjects were tested positive for ADAs, and 2 (0.6%) subjects in the QL1206 who were ADA-positive at the 9th month were positive for Nabs. These results reflect much a higher ADA positivity rate than other studies have reported [7, 11, 18]. The most likely reason is that the definition of ADA positivity in this trial differs from that in other studies. The threshold set for the original drug was much higher than the threshold set in this study. If positivity was determined in this study according to the threshold of the original drug, all participants would be considered negative for ADAs except for 3 subjects who were positive before the first drug administration. Then, the incidence of ADA positivity in this study would be lower than 1%, as in previous studies. The results of immunogenicity tests are highly correlated with the sensitivity and specificity of detection methods and may be affected by many factors, such as the test system, study population and drug combination.
The present study is limited by its duration, which was insufficient to evaluate long-term fracture risk. Data are needed on long-term efficacy and safety in the Chinese population.
In conclusion, QL1206 can effectively increase the BMD of the lumbar spine, total hip, femoral neck and trochanter in postmenopausal Chinese women with osteoporosis and rapidly decrease bone turnover markers compared with placebo. This study demonstrated that QL1206 has beneficial effects on postmenopausal Chinese women with osteoporosis and high fracture risk.
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–95.
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393:364–76.
Wang Y, Tao Y, Hyman ME, Li J, Chen Y. Osteoporosis in China. Osteoporos Int. 2009;20:1651–62.
Gao C, Xu Y, Li L, Gu WQ, Yi CT, Zhu Q, et al. Prevalence of osteoporotic vertebral fracture among community-dwelling elderly in Shanghai. Chin Med J. 2019;132:1749–51.
Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, et al. Rapidly increasing rates of hip fracture in Beijing, China. J Bone Min Res. 2012;27:125–9.
Hofbauer LC, Schoppet M. Clinical implications of the osteoprotegerin/RANKL/RANK system for bone and vascular diseases. JAMA. 2004;292:490–5.
McClung MR, Lewiecki EM, Cohen SB, Bolognese MA, Woodson GC, Moffett AH, et al. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354:821–31.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65.
Bone HG, Wagman RB, Brandi ML, Brown JP, Chapurlat R, Cummings SR, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017;5:513–23.
Orwoll E, Ettinger M, Weiss S, Miller P, Kendler D, Graham J, et al. Alendronate for the treatment of osteoporosis in men. N Engl J Med. 2000;343:604–10.
Koh JM, Chung DJ, Chung YS, Kang MI, Kim IJ, Min YK, et al. Assessment of denosumab in Korean postmenopausal women with osteoporosis: randomized, double-blind, placebo-controlled trial with open-label extension. Yonsei Med J. 2016;57:905–14.
Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–42.
Ferrari S, Adachi JD, Lippuner K, Zapalowski C, Miller PD, Reginster JY, et al. Further reductions in nonvertebral fracture rate with long-term denosumab treatment in the FREEDOM open-label extension and influence of hip bone mineral density after 3 years. Osteoporos Int. 2015;26:2763–71.
Nakamura T, Matsumoto T, Sugimoto T, Hosoi T, Miki T, Gorai I, et al. Clinical Trials Express: fracture risk reduction with denosumab in Japanese postmenopausal women and men with osteoporosis: denosumab fracture intervention randomized placebo controlled trial (DIRECT). J Clin Endocrinol Metab. 2014;99:2599–607.
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, et al. American association of clinical endocrinologists/American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract. 2020;26:1–46.
Kanis JA, Cooper C, Rizzoli R, Reginster JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30:3–44.
Zhang H, Wu M, Zhu X, Li C, Li X, Sun J, et al. A phase I, randomized, single-dose study to evaluate the biosimilarity of QL1206 to denosumab among Chinese healthy subjects. Front Pharmacol. 2020;11:01329.
Nakamura T, Matsumoto T, Sugimoto T, Shiraki M. Dose-response study of denosumab on bone mineral density and bone turnover markers in Japanese postmenopausal women with osteoporosis. Osteoporos Int. 2012;23:1131–40.
Pitale S, Thomas M, Rathi G, Deshmukh V, Kumar P, Reddy S, et al. A randomized placebo-controlled trial of the efficacy of denosumab in Indian postmenopausal women with osteoporosis. Indian J Endocrinol Metab. 2015;19:148–54.
Miller PD, Bolognese MA, Lewiecki EM, McClung MR, Ding B, Austin M, et al. Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone. 2008;43:222–9.
Eastell R, Christiansen C, Grauer A, Kutilek S, Libanati C, McClung MR, et al. Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. J Bone Min Res. 2011;26:530–7.
Acknowledgements
We thank the study participants for their invaluable cooperation. The study was sponsored by Qilu Pharmaceutical Co. Ltd, Jinan, China.
Author information
Authors and Affiliations
Contributions
ZLZ, AJC, QC, DHT, JMY, BWW, YNH, LM, QZ, HY, SGY, KQZ, XLZ, HL, YP, ZY, RCD, LH, LC, YFS, ZLD, LY, BB, MZ, YLC, YKZ, ZJL, ZZ, CQY, YBL, GW, and CCH conceived and designed research; HZ, JMG, ZLZ, AJC, QC, DHT, JMY, BWW, YNH, LM, QZ, HY, SGY, KQZ, XLZ, HL, YP, ZY, RCD, LH, LC, YFS, ZLD, LY, BB, MZ, YLC, YKZ, ZJL, ZZ, CQY, YBL, and GW collected data and conducted research; HZ, JMG, ZLZ, AJC, QC, DHT, JMY, BWW, YNH, LM, QZ, HY, SGY, KQZ, XLZ, HL, YP, ZY, RCD, LH, LC, YFS, ZLD, LY, XXL, and ZJW analysed and interpreted data; HZ, JMG, ZLZ, AJC, and QC wrote the initial paper; HZ, JMG, ZLZ, AJC, QC, DHT, JMY, BWW, YNH, LM, QZ, HY, SGY, KQZ, XLZ, HL, YP, ZY, RCD, LH, LC, YFS, ZLD, LY, BB, MZ, YLC, YKZ, ZJL, ZZ, CQY, YBL, and GW revised the paper; ZLZ was primarily responsible for the final content. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
CCH, ZJW, and XXL are employees of the study sponsor (Qilu Pharmaceutical Co., Ltd) at the time of study. The other authors declare that they have no competing interests.
Ethics approval
This study was approved by the independent ethics committees of 31 participating sites.
Rights and permissions
About this article
Cite this article
Zhang, H., Gu, Jm., Chao, Aj. et al. A phase III randomized, double-blind, placebo-controlled trial of the denosumab biosimilar QL1206 in postmenopausal Chinese women with osteoporosis and high fracture risk. Acta Pharmacol Sin 44, 446–453 (2023). https://doi.org/10.1038/s41401-022-00954-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00954-y