Abstract
Sarcomas, or tumors of connective tissue, represent roughly 20% of childhood cancers. Although the cure rate for sarcomas in general has significantly improved in the last 10 years, there continue to be subgroups that are difficult to treat. High-grade or metastatic soft-tissue sarcomas and rhabdomyosarcomas (RMS) of the extremities remain therapeutic challenges and their prognosis is often poor. The future of sarcoma therapy will likely include molecular approaches including gene/protein expression profiling and gene-based therapy. Most sarcomas harbor defects in the p53 or pRb pathways. The tumor suppressor p53 is central to regulation of cell growth and tumor suppression and restoring wild-type p53 function in pediatric sarcomas may be of therapeutic benefit. Studies with adenoviral-mediated p53 gene transfer have been conducted in many cancer types including cervical, ovarian, prostatic and head and neck tumors. Studies of this approach, however, remain limited in pediatric cancers, including sarcomas. Using three viral constructs containing cDNA for wild-type p53, mutant p53 (C135S) and lacZ, we studied the effect of adenoviral-mediated gene therapy in four pediatric sarcoma cell lines, RD and Rh4 (RMS), Rh1 (Ewing's sarcoma) and A204 (undifferentiated sarcoma). Using the MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) assay, we have shown a dose-dependent decrease in cell viability 72 h post-treatment that occurs with Ad-wtp53 but not with Ad-mutp53. Cells treated with Ad-wtp53 show upregulation of the p53 downstream targets, p21CIP1/WAF1 and bax. Growth curves demonstrate suppression of cell growth over a period of 4 days and cells treated with Ad-wtp53 demonstrate a significant increase in sensitivity to the chemotherapeutic agents, cisplatin and doxorubicin. Our results indicate that restoration of wild-type p53 function in pediatric sarcoma cells could provide a basis for novel approaches to treatment of this disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Mackall CL, Meltzer PS, Helman LJ . Focus on sarcomas. Cancer Cell. 2002;2:175–178.
Gonzalez-Crussi F, Black-Schaffer S . Rhabdomyosarcoma of infancy and childhood. Problems of morphologic classification. Am J Surg Pathol. 1979;3:157–171.
Grier H, Krailo M, Link M, et al. Improved outcome in nonmetastatic Ewing's sarcoma and PNET of bone with the addition of ifosfamide and etoposide to vincristine, Doxorubicin, cyclophosphamide, and actinomycin: a Children's Cancer Group and Pediatric Oncology Group report. Proc Am Soc Clin Oncol. 1994;13:421.
Pawel BR, Hamoudi AB, Asmar L, et al. Undifferentiated sarcomas of children: pathology and clinical behavior — an Intergroup Rhabdomyosarcoma study. Med Pediatr Oncol. 1997;29:170–180.
McDowell HP . Update on childhood rhabdomyosarcoma. Arch Dis Child. 2003;88:354–357.
Wexler LH, Helman LJ . Soft tissue sarcomas of childhood. In: Holland JF, Kufe DW, Pollock RE, et al, eds. Holland-Frei Cancer Medicine. 5th edn. Hamilton, ON: BC Decker Inc. Publisher; 2000.
NCI. Cancer Incidence and Survival among Children and Adolescents: United States SEER Program 1975–1995. Bethesda, MD: National Cancer Institute.
Barr FG, Galili N, Holick J, Biegel JA, Rovera G, Emanuel BS . Rearrangement of the PAX3 paired box gene in the paediatric solid tumour alveolar rhabdomyosarcoma. Nat Genet. 1993;3:113–117.
Galili N, Davis RJ, Fredericks WJ, et al. Fusion of a fork head domain gene to PAX3 in the solid tumour alveolar rhabdomyosarcoma. Nat Genet. 1993;5:230–235.
Davis RJ, D'Cruz CM, Lovell MA, Biegel JA, Barr FG . Fusion of PAX7 to FKHR by the variant t(1;13)(p36;q14) translocation in alveolar rhabdomyosarcoma. Cancer Res. 1994;54:2869–2872.
Sorensen PH, Lynch JC, Qualman SJ, et al. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: a report from the children's oncology group. J Clin Oncol. 2002;20:2672–2679.
Barr FG . Gene fusions involving PAX and FOX family members in alveolar rhabdomyosarcoma. Oncogene. 2001;20:5736–5746.
Diller L, Sexsmith E, Gottlieb A, Li FP, Malkin D . Germline p53 mutations are frequently detected in young children with rhabdomyosarcoma. J Clin Invest. 1995;95:1606–1611.
Pulciani S, Santos E, Lauver AV, Long LK, Aaronson SA, Barbacid M . Oncogenes in solid human tumours. Nature. 1982;300:539–542.
Chardin P, Yeramian P, Madaule P, Tavitian A . N-ras gene activation in the RD human rhabdomyosarcoma cell line. Int J Cancer. 1985;35:647–652.
Ferracini R, Olivero M, Di Renzo MF, et al. Retrogenic expression of the MET proto-oncogene correlates with the invasive phenotype of human rhabdomyosarcomas. Oncogene. 1996;12:1697–1705.
Dagher R, Helman L . Rhabdomyosarcoma: an overview. Oncologist. 1999;4:34–44.
Koscielniak E, Rodary C, Flamant F, et al. Metastatic rhabdomyosarcoma and histologically similar tumors in childhood: a retrospective European multi-center analysis. Med Pediatr Oncol. 1992;20:209–214.
Raney Jr RB, Tefft M, Maurer HM, et al. Disease patterns and survival rate in children with metastatic soft-tissue sarcoma. A report from the Intergroup Rhabdomyosarcoma Study (IRS)-I. Cancer. 1988;62:1257–1266.
Delattre O, Zucman J, Melot T, et al. The Ewing family of tumors — a subgroup of small-round-cell tumors defined by specific chimeric transcripts. N Engl J Med. 1994;331:294–299.
Scotlandi K, Serra M, Manara MC, et al. Immunostaining of the p30/32MIC2 antigen and molecular detection of EWS rearrangements for the diagnosis of Ewing's sarcoma and peripheral neuroectodermal tumor. Hum Pathol. 1996;27:408–416.
West DC . Ewing sarcoma family of tumors. Curr Opin Oncol. 2000;12:323–329.
Weber KL, Sim FH . Ewing's sarcoma: presentation and management. J Orthop Sci. 2001;6:366–371.
Denny CT . Gene rearrangements in Ewing's sarcoma. Cancer Invest. 1996;14:83–88.
Massey GV, Dunn NL, Heckel JL, Davis EC, Jackson-Cook C, Russell EC . Unusual presentation of Ewing sarcoma with t(21;22) in a 3-year-old boy. J Pediatr Hematol Oncol. 1996;18:198–201.
Bertolotti A, Lutz Y, Heard DJ, Chambon P, Tora L . hTAF(II)68, a novel RNA/ssDNA-binding protein with homology to the pro-oncoproteins TLS/FUS and EWS is associated with both TFIID and RNA polymerase II. EMBO J. 1996;15:5022–5031.
Bertolotti A, Melot T, Acker J, Vigneron M, Delattre O, Tora L . EWS, but not EWS-FLI-1, is associated with both TFIID and RNA polymerase II: interactions between two members of the TET family, EWS and hTAFII68, and subunits of TFIID and RNA polymerase II complexes. Mol Cell Biol. 1998;18:1489–1497.
May WA, Lessnick SL, Braun BS, et al. The Ewing's sarcoma EWS/FLI-1 fusion gene encodes a more potent transcriptional activator and is a more powerful transforming gene than FLI-1. Mol Cell Biol. 1993;13:7393–7398.
Abudu A, Mangham DC, Reynolds GM, et al. Overexpression of p53 protein in primary Ewing's sarcoma of bone: relationship to tumour stage, response and prognosis. Br J Cancer. 1999;79:1185–1189.
de Alava E, Antonescu CR, Panizo A, et al. Prognostic impact of P53 status in Ewing sarcoma. Cancer. 2000;89:783–792.
Lopez-Guerrero JA, Pellin A, Noguera R, Carda C, Llombart-Bosch A . Molecular analysis of the 9p21 locus and p53 genes in Ewing family tumors. JA Lab Invest. 2001;81:803–814.
Wilkins RM, Pritchard DJ, Burgert Jr EO, Unni KK . Ewing's sarcoma of bone. Experience with 140 patients. Cancer. 1986;58:2551–2555.
Cotterill SJ, Ahrens S, Paulussen M, et al. Prognostic factors in Ewing's tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing's Sarcoma Study Group. J Clin Oncol. 2000;18:3108–3114.
Burgert Jr EO, Nesbit ME, Garnsey LA, et al. Multimodal therapy for the management of nonpelvic, localized Ewing's sarcoma of bone: intergroup study IESS-II. J Clin Oncol. 1990;8:1514–1524.
Arndt CA, Crist WM . Common musculoskeletal tumors of childhood and adolescence. N Engl J Med. 1999;341:342–352.
Chung EB . Current classification of soft tissue tumors. In: Fletcher CDM, McKee PH eds. Pathobiology of Soft Tissue Tumors. New York, NY: Churchill; 1991.
Hamada K, Alemany R, Zhang WW, et al. Adenovirus-mediated transfer of a wild-type p53 gene and induction of apoptosis in cervical cancer. Cancer Res. 1996;56:3047–3054.
Kigawa J, Sato S, Shimada M, et al. p53 gene status and chemosensitivity in ovarian cancer. Hum Cell. 2001;14:165–171.
Sweeney P, Pisters LL . Ad5CMVp53 gene therapy for locally advanced prostate cancer — where do we stand? World J Urol. 2000;18:121–124.
Swisher SG, Roth JA . Clinical update of Ad-p53 gene therapy for lung cancer. Surg Oncol Clin N Am. 2002;11:521–535.
Shimada H, Matsubara H, Ochiai T . p53 gene therapy for esophageal cancer. J Gastroenterol. 2002;37:87–91.
Liu FF . Novel gene therapy approach for nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12:505–515.
Frank DK . Gene therapy for head and neck cancer. Surg Oncol Clin N Am. 2002;11:589–606.
Delatte SJ, Hazen-Martin DJ, Re GG, Kelly JR, Sutphin A, Tagge EP . Restoration of p53 function in anaplastic Wilms' tumor. J Pediatr Surg. 2001;36:43–50.
Shetty S, Taylor AC, Harris LC . Selective chemosensitization of rhabdomyosarcoma cell lines following wild-type p53 adenoviral transduction. Anticancer Drugs. 2002;13:881–889.
Kawashima H, Ogose A, Yoshizawa T, et al. Expression of the coxsackievirus and adenovirus receptor in musculoskeletal tumors and mesenchymal tissues: efficacy of adenoviral gene therapy for osteosarcoma. Cancer Sci. 2003;94:70–75.
Marcellus RC, Teodoro JG, Charbonneau R, Shore GC, Branton PE . Expression of p53 in Saos-2 osteosarcoma cells induces apoptosis which can be inhibited by Bcl-2 or the adenovirus E1B-55 kDa protein. Cell Growth Differ. 1996;7:1643–1650.
Laffon B, Pasaro E, Mendez J . Effects of styrene-7,8-oxide over p53, p21, bcl-2 and bax expression in human lymphocyte cultures. Mutagenesis. 2001;16:127–132.
Hodges NJ, Chipman JK . Down-regulation of the DNA-repair endonuclease 8-oxo-guanine DNA glycosylase 1 (hOGG1) by sodium dichromate in cultured human A549 lung carcinoma cells. Carcinogenesis. 2002;23:55–60.
Webb JL . Effect of more than one inhibitor. In: Webb JL, ed. Enzymes and Metabolic Inhibitors. Vol. 1. New York, NY: Academic Press; 1963: 66–79, 487–512.
Yeh YA, Herenyiova M, Weber G . Quercetin: synergistic action with carboxyamidotriazole in human breast carcinoma cells. Life Sci. 1995;57:1285–1292.
Zhang L, Hung MC . Sensitization of HER-2/neu-overexpressing non-small cell lung cancer cells to chemotherapeutic drugs by tyrosine kinase inhibitor emodin. Oncogene. 1996;12:571–576.
Chang EH, Pirollo KF, Bouker KB . Tp53 gene therapy: a key to modulating resistance to anticancer therapies? Mol Med Today. 2000;6:358–364.
Ganjavi H, Gee M, Narendran A, et al. Adenovirus-mediated p53 gene therapy in osteosarcoma cell lines: Sensitisation to cisplatin and doxorubicin. Hum Gene Ther. (under review). 2004.
Levine AJ . p53, the cellular gatekeeper for growth and division. Cell. 1997;88:323–331.
Greenblatt MS, Bennett WP, Hollstein M, Harris CC . Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res. 1994;54:4855–4878.
Hollstein M, Sidransky D, Vogelstein B, Harris CC . p53 mutations in human cancers. Science. 1991;253:49–53.
Nigro JM, Baker SJ, Preisinger AC, et al. Mutations in the p53 gene occur in diverse human tumour types. Nature. 1989;342:705–708.
Smith ND, Rubenstein JN, Eggener SE, Kozlowski JM . The p53 tumor suppressor gene and nuclear protein: basic science review and relevance in the management of bladder cancer. J Urol. 2003;169:1219–1228.
Donehower LA, Harvey M, Slagle BL, et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature. 1992;356:215–221.
Jacks T, Remington L, Williams BO, et al. Tumor spectrum analysis in p53-mutant mice. Curr Biol. 1994;4:1–7.
Purdie CA, Harrison DJ, Peter A, et al. Tumour incidence, spectrum and ploidy in mice with a large deletion in the p53 gene. Oncogene. 1994;9:603–609.
Malkin D, Li FP, Strong LC, et al. Germ line p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms. Science. 1990;250:1233–1238.
Varley JM . Germline TP53 mutations and Li-Fraumeni syndrome. Hum Mutat. 2003;21:313–320.
Srivastava S, Zou ZQ, Pirollo K, et al. Germ-line transmission of a mutated p53 gene in a cancer-prone family with Li-Fraumeni syndrome. Nature. 1990;348:747–749.
Tsuchiya T, Sekine K, Hinohara S, et al. Analysis of the p16INK4, p14ARF, p15, TP53, and MDM2 genes and their prognostic implications in osteosarcoma and Ewing sarcoma. Cancer Genet Cytogenet. 2000;120:91–98.
Nielsen LL, Dell J, Maxwell E, et al. Efficacy of p53 adenovirus-mediated gene therapy against human breast cancer xenografts. Cancer Gene Ther. 1997;4:129–138.
Bookstein R, Demer W, Gregory R, et al. p53 gene therapy in vivo of hepatocellular and liver metastatic colorectal cancer. Semin Oncol. 1996;23:66–77.
Kock H, Harris MP, Anderson SC, et al. Adenovirus-mediated p53 gene transfer suppresses growth of human glioblastoma cells in vitro and in vivo. Int J Cancer. 1996;67:808–815.
Mujoo K, Maneval DC, Anderson SC, et al. Adenoviral-mediated p53 tumor suppressor gene therapy of human ovarian carcinoma. Oncogene. 1996;12:1617–1623.
Tursz T, Le Cesne A, Baldeyrou P, et al. Phase I study of a recombinant adenovirus-mediated gene transfer in lung cancer patients. J Natl Cancer Inst. 1996;88:1857–1863.
Clayman GL, el-Naggar AK, Lippman SM, et al. Adenovirus-mediated p53 gene transfer in patients with advanced recurrent head and neck squamous cell carcinoma. J Clin Oncol. 1998;16:2221–2232.
Clayman GL, Frank DK, Bruso PA, et al. Adenovirus-mediated wild-type p53 gene transfer as a surgical adjuvant in advanced head and neck cancers. Clin Cancer Res. 1999;5:1715–1722.
Reid T, Warren R, Kirn D . Intravascular adenoviral agents in cancer patients: lessons from clinical trials. Cancer Gene Ther. 2002;9:979–986.
Neyns B, Noppen M . Intratumoral gene therapy for non-small cell lung cancer: current status and future directions. Monaldi Arch Chest Dis. 2003;59:287–295.
Asaoka K, Tada M, Sawamura Y, Ikeda J, Abe H . Dependence of efficient adenoviral gene delivery in malignant glioma cells on the expression levels of the Coxsackievirus and adenovirus receptor. J Neurosurg. 2000;92:1002–1008.
Hutchin ME, Pickles RJ, Yarbrough WG . Efficiency of adenovirus-mediated gene transfer to oropharyngeal epithelial cells correlates with cellular differentiation and human coxsackie and adenovirus receptor expression. Hum Gene Ther. 2000;11:2365–2375.
Turturro F, Seth P, Link Jr CJ . In vitro adenoviral vector p53-mediated transduction and killing correlates with expression of coxsackie-adenovirus receptor and alpha(nu)beta5 integrin in SUDHL-1 cells derived from anaplastic large-cell lymphoma. Clin Cancer Res. 2000;6:185–192.
Li D, Duan L, Freimuth P, O'Malley Jr BW . Variability of adenovirus receptor density influences gene transfer efficiency and therapeutic response in head and neck cancer. Clin Cancer Res. 1999;5:4175–4181.
Pearson AS, Koch PE, Atkinson N, et al. Factors limiting adenovirus-mediated gene transfer into human lung and pancreatic cancer cell lines. Clin Cancer Res. 1999;5:4208–4213.
Croyle MA, Walter E, Janich S, Roessler BJ, Amidon GL . Role of integrin expression in adenovirus-mediated gene delivery to the intestinal epithelium. Hum Gene Ther. 1998;9:561–573.
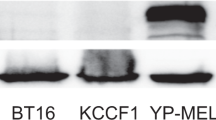
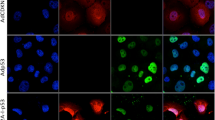
Hemmi S, Geertsen R, Mezzacasa A, Peter I, Dummer R . The presence of human coxsackievirus and adenovirus receptor is associated with efficient adenovirus-mediated transgene expression in human melanoma cell cultures. Hum Gene Ther. 1998;9:2363–2373.
Takayama K, Ueno H, Pei XH, Nakanishi Y, Yatsunami J, Hara N . The levels of integrin alpha v beta 5 may predict the susceptibility to adenovirus-mediated gene transfer in human lung cancer cells. Gene Ther. 1998;5:361–368.
Hamilton TE, McClane SJ, Baldwin S, et al. Efficient adenoviral-mediated murine neonatal small intestinal gene transfer is dependent on alpha(v) integrin expression. J Pediatr Surg. 1997;32:1695–1703.
Acknowledgements
HG is supported by funds from the Canadian Institutes of Health Research. MG was funded by a Restracomp Studentship (Research Institute, The Hospital for Sick Children). AN is supported by a Research Scientist award from the Kids Cancer Care Foundation of Alberta. DM is a Research Scientist of the National Cancer Instititute of Canada/Canadian Cancer Society. This work was supported in part by a Seed Grant of the Research Institute, The Hospital for Sick Children, the Andrew Mizzoni Cancer Research Fund, and the Harry and Hannah Fisher Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganjavi, H., Gee, M., Narendran, A. et al. Adenovirus-mediated p53 gene therapy in pediatric soft-tissue sarcoma cell lines: sensitization to cisplatin and doxorubicin. Cancer Gene Ther 12, 397–406 (2005). https://doi.org/10.1038/sj.cgt.7700798
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cgt.7700798
Keywords
This article is cited by
-
miR-125b develops chemoresistance in Ewing sarcoma/primitive neuroectodermal tumor
Cancer Cell International (2013)
-
KiSS1 mediates platinum sensitivity and metastasis suppression in head and neck squamous cell carcinoma
Oncogene (2011)
-
Heterogeneous in vitro effects of doxorubicin on gene expression in primary human liposarcoma cultures
BMC Cancer (2008)
-
Role of hypoxia inducible factor-1 alpha in modulation of apoptosis resistance
Oncogene (2007)
-
Effects of standard chemotherapy on tumor growth and regulation of multidrug resistance genes and proteins in childhood rhabdomyosarcoma
Pediatric Surgery International (2007)