Abstract
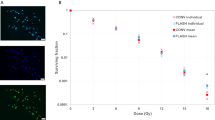
The combined therapeutic effect of cytokine-producing cancer cell vaccines and local radiotherapy was studied in a mouse glioma 261 (Gl261) brain tumor model. Brain tumor–bearing mice were treated with cytokine (IL-4, IL-6, IL-7, GM-CSF, TNF-α, LIF, LT) producing vaccines made by in vitro transduction of Gl261 cells with the corresponding adenoviral vectors. Vaccines producing either IL-4 or GM-CSF cured 20–40% of mice. The antitumor effect strongly depended on the secreted cytokine level. Vaccination therapy induced specific activation of cytotoxic T lymphocytes measured by cell-mediated cytotoxicity assay. Brain tumors were heavily infiltrated by CD4+ lymphocytes after treatment with IL-4– or GM-CSF–secreting cells. GM-CSF vaccination induced moderate CD8+ infiltration, as well. Depleting either CD4+ or CD8+ lymphocyte subsets abolished the anticancer effect of GM-CSF–expressing cells. Strong synergism was observed by combining cytokine vaccination (GM-CSF, IL-4, IL-12) with local tumor irradiation: about 80–100% of the glioma-bearing mice was cured. The high efficiency of combined treatment was maintained even under suboptimal conditions when neither of the modalities cured any of the mice alone. This suggests that vaccination therapy might open a new potential in the clinical treatment of high-grade gliomas when applied as adjuvant to existing treatment modalities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Shoenberg BS . In: Walker MD, ed. Oncology of the Nervous System Boston: Martinus Nijhoff 1983 1–30
Mahaley MS, Mettlin C, Natarajan N et al. National survey of patterns of care for brain-tumor patients J Neurosurg 1989 71: 826–836
Shawler DL, Fakhrai H, Van Beveren C et al. Gene therapy approaches to enhance antitumor immunity Adv Pharmacol 1997 40: 309–37
Forni G, Foa R, Santoni A, Frati L eds. Cytokine-Induced Tumor Immunogenicity San Diego, CA, USA: Academic Press 1994
Dranoff G, Jaffee E, Lazenby A et al. Vaccination with irradiated tumor cells engineered to secrete murine granulocyte–macrophage colony-stimulating factor stimulates potent, specific, and long-lasting anti-tumor immunity Proc Natl Acad Sci USA 1993 90: 3539–3543
Allione A, Consalvo M, Nanni P et al. Immunizing and curative potential of replicating and nonreplicating murine mammary adenocarcinoma cells engineered with interleukin (IL)-2, IL-4, IL-6, IL-7, IL-10, tumor necrosis factor alpha, granulocyte–macrophage colony-stimulating factor, and gamma-interferon gene or admixed with conventional adjuvants Cancer Res 1994 54: 6022–6026
Inoue M, Plautz GE, Shu S . Treatment of intracranial tumors by systemic transfer of superantigen-activated tumor-draining lymph node T cells Cancer Res 1996 56: 4702–4708
Désaknai Sz, Lumniczky K, Hidvégi EJ et al. Brain tumor treatment with IL-2 and IL-12 producing autologous cancer cell vaccines Adv Exp Med Biol 2001 495: 369–372
Shapiro WR, Ausman JI, Rall DP . Studies on the chemotherapy of experimental brain tumors: evaluation of 1,3-bis(2-chloroethyl)-1-nitrosourea, cyclophosphamide, mithramycin and methotrexate Cancer Res 1970 30: 2401–2413
Nakamura Y, Wakimoto H, Abe J et al. Adoptive immunotherapy with murine tumor-specific T lymphocytes engineered to secrete interleukin 2 Cancer Res 1994 54: 5757–5760
Coligen JE, Kruisbeek AM, Marguiles DH et al, eds. Current Protocols in Immunology USA: Wiley 1996 2.6.1–2.8.1
Nakayama E, Shiku H, Takahashi T et al. Definition of a unique cell surface antigen of mouse leukemia RL1 by cell-mediated cytotoxicity Proc Natl Acad Sci USA 1979 76: 3486–3490
Saito S, Bannerji R, Gansbacher B et al. Immunotherapy of bladder cancer with cytokine gene-modified tumor vaccines Cancer Res 1994 54: 3516–3520
Parney IF, Hao C, Petruk KC . Glioma immunology and immunotherapy Neurosurgery 2000 46: 778–792
Wakimoto H, Abe J, Tsunoda R et al. Intensified antitumor immunity by a cancer vaccine that produces granulocyte–macrophage colony-stimulating factor plus interleukin 4 Cancer Res 1996 56: 1828–1833
Sampson JH, Archer GE, Ashley DM et al. Subcutaneous vaccination with irradiated, cytokine-producing tumor cells stimulates CD8+ cell-mediated immunity against tumors located in the immunologically privileged central nervous system Proc Natl Acad Sci USA 1996 93: 10399–10404
Yu JS, Burwick JA, Dranoff G, Breakefield XO . Gene therapy for metastatic brain tumors by vaccination with granulocyte–macrophage colony-stimulating factor-transduced tumor cells Hum Gene Ther 1997 8: 1065–1072
Benedetti S, Bruzzone MG, Pollo B et al. Eradication of rat malignant gliomas by retroviral-mediated, in vivo delivery of the interleukin 4 gene Cancer Res 1999 59: 645–652
Giezeman KM, Okada H, Brisette-Storkus CS et al. Cytokine gene therapy of gliomas: induction of reactive CD4 + T cells by interleukin-4–transfected 9L gliosarcoma is essential for protective immunity Cancer Res 2000 60: 2449–2457
Chen B, Timiryasova TM, Andres ML et al. Evaluation of combined vaccinia virus-mediated antitumor gene therapy with p53, IL-2, and IL-12 in a glioma model Cancer Gene Ther 2000 7: 1437–1447
Chen B, Timiryasova TM, Haghighat P et al. Low-dose vaccinia virus–mediated cytokine gene therapy of gliomas J Immunother 2001 24: 46–57
Saleh M, Jonas NK, Wiegmans A, Stylli SS . The treatment of established intracranial tumors by in situ retroviral IFN-gamma transfer Gene Ther 2000 7: 1715–1724
Iwadate Y, Tagawa M, Namba H et al. Immunological responsiveness to interleukin-2–producing brain tumors can be restored by concurrent subcutaneous transplantation of the same tumors Cancer Gene Ther 2000 7: 1263–1269
DiMeco F, Rhines LD, Hanes J et al. Paracrine delivery of IL-12 against intracranial 9L gliosarcoma in rats J Neurosurg 2000 92: 419–427
Okada H, Giezeman-Smits KM, Tahara H et al. Effective cytokine gene therapy against an intracranial glioma using a retrovirally transduced IL-4 plus HSVtk tumor vaccine Gene Ther 1999 6: 219–226
Saleh M, Wiegmans A, Malone Q et al. Effect of in situ retroviral interleukin-4 transfer on established intracranial tumors J Natl Cancer Inst 1999 91: 438–445
Aoki T, Tashiro K, Miyatake SI et al. Expression of murine interleukin 7 in a murine glioma cell line results in reduced tumorigenicity in vivo Proc Natl Acad Sci USA 1992 89: 3850–3854
Herrlinger U, Kramm CM, Johnston KM et al. Vaccination for experimental gliomas using GM-CSF–transduced glioma cells Cancer Gene Ther 1997 4: 345–352
Natsume A, Tsujimura K, Mizuno M et al. IFN-beta gene therapy induces systemic antitumor immunity against malignant glioma J Neuro-Oncol 2000 47: 117–124
Herrlinger U, Jacobs A, Quinones A et al. Helper virus-free herpes simplex virus type 1 amplicon vectors for granulocyte–macrophage colony-stimulating factor-enhanced vaccination therapy for experimental glioma Hum Gene Ther 2000 11: 1429–1438
Glick RP, Lichtor T, de Zoeten E et al. Prolongation of survival of mice with glioma treated with semiallogeneic fibroblasts secreting interleukin-2 Neurosurgery 1999 45: 867–874
Natsume A, Mizuno M, Ryuke Y, Yoshida J . Antitumor effect and cellular immunity activation by murine interferon-beta gene transfer against intracerebral glioma in mouse Gene Ther 1999 6: 1626–1633
Donson AM, Foreman NK . Adenovirus mediated gene therapy in a glioblastoma vaccine model; specific antitumor immunity and abrogation of immunosuppression J Neuro-Oncol 1998 40: 205–214
Thomson AW ed. The Cytokine Handbook New York, NY: Academic Press 1994
Griscelli F, Li H, Cheong C et al. Combined effects of radiotherapy and angiostatin gene therapy in glioma tumor model Proc Natl Acad Sci USA 2000 97: 6698–6703
Gridley DS, Andres ML, Li J et al. Evaluation of radiation effects against C6 glioma in combination with vaccinia virus–p53 gene therapy Int J Oncol 1998 13: 1093–1098
Broaddus WC, Liu Y, Steele GT et al. Enhanced radiosensitivity of malignant glioma cells after adenoviral p53 transduction J Neurosurg 1999 91: 997–1004
Badie B, Goh CS, Klaver J et al. Combined radiation and p53 gene therapy of malignant glioma cells Cancer Gene Ther 1999 6: 155–162
Li J, Andres ML, Fodor I et al. Evaluation of pGL1–TNF-alpha therapy in combination with radiation Oncol Res 1998 10: 379–387
Staba MJ, Mauceri HJ, Kufe DW et al. Adenoviral TNF-alpha gene therapy and radiation damage tumor vasculature in a human malignant glioma xenograft Gene Ther 1998 5: 293–300
Acknowledgements
This work was supported by an international collaborative ICGEB (CRP/HUN98-02-t2) Grant and Hungarian National Founds: ETT 6100/1/2000, ETT 247/1996, OTKA T-025810, OTKA T-032499, OMFB 96-97-65-1201 to GS, and OTKA T-025333, AKP-96/2-654-3.2 to EH. The authors thank Maria Frigyesi and Erzsebet Fekete for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lumniczky, K., Desaknai, S., Mangel, L. et al. Local tumor irradiation augments the antitumor effect of cytokine-producing autologous cancer cell vaccines in a murine glioma model. Cancer Gene Ther 9, 44–52 (2002). https://doi.org/10.1038/sj.cgt.7700398
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cgt.7700398
Keywords
This article is cited by
-
Overcoming blood brain barrier with a dual purpose Temozolomide loaded Lactoferrin nanoparticles for combating glioma (SERP-17-12433)
Scientific Reports (2017)
-
Cytokines: shifting the balance between glioma cells and tumor microenvironment after irradiation
Journal of Cancer Research and Clinical Oncology (2015)
-
The effect of ionizing radiation on the homeostasis and functional integrity of murine splenic regulatory T cells
Inflammation Research (2013)
-
Activation of a glioma-specific immune response by oncolytic parvovirus Minute Virus of Mice infection
Cancer Gene Therapy (2012)
-
Adenoviral vector transduction of the human deoxycytidine kinase gene enhances the cytotoxic and radiosensitizing effect of gemcitabine on experimental gliomas
Cancer Gene Therapy (2008)