Abstract
Purpose
To report short-term results of intravitreal bevacizumab (IVB) injection for macular oedema (ME) associated with branch retinal vein occlusion (BRVO).
Methods
Retrospective interventional case series of 12 eyes of 12 consecutive patients. IVB injections (1.25 mg/0.05 ml) were given as needed based on the presence of ME on optical coherence tomography. Changes in Snellen visual acuity (VA) and central macular thickness (CMT) were analysed using the Student's paired t-test.
Results
At a mean follow-up of 9.8 months (range: 6–17 months), the mean number of IVB injections given was 4 (range: 1–6). No ocular or systemic side effects were noted. The differences in logMAR VA between baseline and 1 month, between baseline and 6 months, and between baseline and final follow-up were statistically significant (P<0.05). The differences in CMT between baseline and 1 month, baseline and 6 months, and between baseline and final follow-up were also statistically significant (P<0.05).
Conclusion
Short-term results indicate that IVB is useful in decreasing ME and improving VA in eyes with BRVO.
Similar content being viewed by others
Introduction
Intravitreal bevacizumab (IVB) (Avastin®, Genentech, San Francisco, CA, USA) is used off-label for the treatment of VEGF-mediated ocular diseases such as choroidal neovascularization, proliferative diabetic retinopathy, retinal vein occlusions, and pseudophakic macular oedema.1, 2, 3, 4, 5 The purpose of this study is to describe short-term visual and anatomic outcomes following IVB for macular oedema (ME) due to branch retinal vein occlusion (BRVO).
Materials and methods
After institutional review board (IRB) approval, a retrospective review of 12 eyes of 12 consecutive patients with ME due to BRVO, treated with IVB, was performed. Informed consent about the benefits, risks, off-label nature, and alternatives to treatment was obtained from all the patients.
Each patient underwent complete ocular examination and optical coherence tomography (OCT) measurement of central macular thickness (CMT) at baseline and follow-up examinations. Ten of 12 patients had fluorescein angiography immediately prior to the first IVB treatment. After topical anaesthesia, using sterile technique, 0.05 ml (1.25 mg) bevacizumab was given intravitreally, 3.5 mm posterior to the limbus.
The patients were initially followed up at 4-week intervals. IVB was given as needed based on the presence of ME on OCT. The interval of follow-up examinations was increased to longer periods once the ME resolved. The patients were advised to call back sooner as needed.
The Snellen visual acuities (VA) were converted into LogMAR for statistical analysis, then back to Snellen. The differences in visual acuity and CMT were analysed using the Student's paired t-test.
Results
The mean age of the 12 patients was 69.8 years (range: 42–95 years, 10 female, 3 male). Two patients had a prior diagnosis of glaucoma. Systemic associations included hypertension in five patients, hypertension and diabetes mellitus in one patient, hypertension and hypercholesterolemia in one patient, and hypertension and anaemia in one patient. Table 1 depicts the visual acuity and CMT at initial examination, at 1 month, 6 months, and at the final examination, and the follow-up and time interval(s) for IVB injections in 12 eyes with BRVO and ME.
Prior ocular treatment included focal laser treatment and posterior subtenon triamcinolone in four eyes (nos. 2, 7, 8, 11), focal laser treatment and intravitreal triamcinolone in one eye (no. 1), intravitreal triamcinolone in one eye (no. 6), and posterior subtenon triamcinolone in one eye (no. 4). The ME associated with BRVO either did not respond to or recurred after these treatments. These treatments were performed at least 3 months prior to IVB. There was some macular ischaemia in 4 of 10 patients by fluorescein angiography (nos. 3–6).
All patients had at least 6 months of follow-up. The mean number of IVB injections given over the 6-month interval was 2.8 (range: 1–5). At a mean follow-up of 9.8 months (range: 6–17 months), the mean number of IVB injections given was 4 (range: 1–6). Three patients (nos. 5, 6, 9) did well at follow-ups of 8–9 months after the initial one or two injections (Figures 1 and 2). Patient no. 10 required five subsequent injections at 1-month intervals for persistent ME. The other patients had recurrent ME at a mean follow-up of 3.4 months (range: 2–6 months) after the last IVB injection. No ocular or systemic side effects were noted.
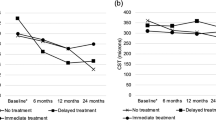
The mean logMAR VA was 0.91 (Snellen equivalent: 20/163) at baseline, 0.66 (Snellen equivalent: 20/91) at 1 month, 0.58 (Snellen equivalent: 20/76) at 6 months, and 0.48 (Snellen equivalent: 20/60) at the final follow-up (Figure 3). The mean CMT was 506.6 μm at baseline, 270.1 μm at 1 month, 321.8 μm at 6 months, and 267.5 μm at the final follow-up (Figure 4). The differences in logMAR VA between baseline and 1 month, between baseline and 6 months, and between baseline and final follow-up were statistically significant (P=0.040, 0.028, and 0.004, respectively). The differences in CMT between baseline and 1 month, baseline and 6 months, and between baseline and final follow-up were also statistically significant (P=0.003, 0.038, and 0.003, respectively).
Discussion
The cause of BRVO is usually a localized thrombus formation in a branch retinal vein due to arteriosclerosis adjacent to a branch retinal arteriole. Complications of BRVO include disc and retinal neovascularization as well as ME. Results of the branch vein occlusion study (BVOS) showed that if ME persists beyond 3 months and visual acuity is reduced below 20/40, the patient may be treated with focal laser photocoagulation.6 Intravitreal triamcinolone acetonide (IVTA) and intravitreal ranbizumab are currently in clinical trials for the treatment of ME due to BRVO. However, intravitreal injections have a short half-life (bevacizumab 4.32 days, ranibizumab 2.88 days, and triamcinolone 18.6 days)7, 8, 9 and require repeated injections. Repeated IVTA injections are associated with cataract and glaucoma in up to 50% of the cases.10, 11 Long-acting steroid implants such as the Posurdex biodegradable dexamethasone implant are also currently in clinical trials for the treatment of ME due to vein occlusions.
Our results point out that with longer follow-up the need for IVB injections may increase due to recurrent ME. The mean time for recurrence of ME was 3.4 months in our series. Other reports also disclosed similar periods ranging from 2 to 3 months from the last IVB to recurrence of ME.11, 12, 13
In conclusion, this short-term study shows that IVB was useful in decreasing ME and improving visual acuity in patients with BRVO with no side effects. Most eyes will require multiple injections for persistent or recurrent ME.
References
Rosenfeld PJ, Mosfeghi AA, Puliafito CA . Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging 2005; 36: 331–335.
Avery RL, Pieramici D, Rabena M, Castellarin AA, Nasir MA, Giust MJ . Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology 2006; 113: 363–372.
Avery RL, Pearlman J, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology 2006; 113: 1695–1705.
Iturralde D, Spaide RF, Meyerle CB, Klancnik JM, Yannuzzi LA, Fisher YL et al. Intravitreal bevacizumab (Avastin) treatment of macular edema in central retinal vein occlusion. A short term study. Retina 2006; 26: 279–284.
Mason JO, Albert Jr MA, Vail R . Intravitreal bevacizumab (Avastin) for refractory pseudophakic cystoid macular edema. Retina 2006; 26: 356–357.
The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984; 98: 271–282.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ . Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 2007; 114 (5): 855–859.
Beer PM, Bakri SJ, Singh RJ, Liu W, Peters III GB, Miller M . Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 2003; 110 (4): 681–686.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Ezzat MK, Singh RJ . Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology 2007; 114: 2179–2182.
Çekiç O, Chang S, Tseng JJ, Bairle GR, Del Priore LV, Weisman H et al. Intravitreal triamcinolone injection for treatment of macular edema secondary to branch retinal vein occlusion. Retina 2005; 25: 851–858.
Chen SD, Sundaram V, Lochhead J, Patel CK . Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol 2006; 141: 876–883.
Rabena MD, Pieramici DJ, Castellarin AA, Nasir MA, Avery RL . Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina 2007; 27: 419–425.
Pai SA, Shetty R, Vijayan PB, Venkatasubramaniam G, Yadav NK, Shetty BK et al. Clinical, anatomic, and electrophysiologic evaluation following intravitreal bevacizumab for macular edema in retinal vein occlusion. Am J Ophthalmol 2007; 143: 601–606.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors have any proprietary interest in any of the products mentioned in this paper
Rights and permissions
About this article
Cite this article
Gündüz, K., Bakri, S. Intravitreal bevacizumab for macular oedema secondary to branch retinal vein occlusion. Eye 22, 1168–1171 (2008). https://doi.org/10.1038/sj.eye.6703040
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703040
This article is cited by
-
Three intravitreal bevacizumab versus two intravitreal triamcinolone injections in recent-onset branch retinal vein occlusion
Graefe's Archive for Clinical and Experimental Ophthalmology (2012)
-
Intravitreal bevacizumab for macular oedema secondary to branch retinal vein occlusion: more data required
Eye (2010)
-
Blood pressure changes after intravitreal bevacizumab in patients grouped by ocular pathology
Eye (2010)
-
Intravitreal triamcinolone acetonide vs bevacizumab for treatment of macular oedema secondary to branch retinal vein occlusion
Eye (2009)
-
Combined intravitreal triamcinolone injection and laser photocoagulation in eyes with persistent macular edema after branch retinal vein occlusion
Graefe's Archive for Clinical and Experimental Ophthalmology (2008)