Abstract
Background
Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) are first-line therapy for macular oedema in retinal vein occlusion (RVO). Appropriate management for RVO with good visual acuity at diagnosis has not been evaluated. The purpose of this study is to analyse the visual and anatomic outcomes from anti-VEGF treatment among RVO patients with good vision at baseline.
Methods
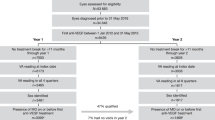
This retrospective cohort study evaluated patients diagnosed with macular oedema secondary to RVO from January 2012 to February 2021 at a tertiary ophthalmic centre. Patients had a Snellen acuity of 20/32 or better at diagnosis. Three cohorts were compared: patients with no anti-VEGF treatment, delayed anti-VEGF treatment (initial injection >30 days post-diagnosis) and immediate anti-VEGF treatment (initial injection ≤30 days post-diagnosis). Central subfield thickness (CST) and best visual acuity (BVA) were collected at diagnosis and 6-, 12- and 24-month follow-up appointments.
Results
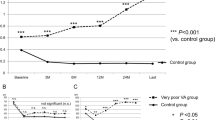
Among 131 eyes, mean BVA values among treatment groups did not differ at 6-, 12- or 24-month follow up visits (P = 0.521, 0.426, 0.356, respectively). The percentage of eyes with at least a 5-letter BVA decrease at 24 months was 24.1%, 65.0% and 30.8% in the no treatment, delayed and immediate treatment groups respectively (P = 0.010). There was no significant difference in the percentage of eyes with at least a 10% decrease in CST at 24 months among groups (P = 0.095).
Conclusions
Close observation with initiation of treatment in patients with good visual acuity with macular oedema secondary to RVO as indicated has similar outcomes in the setting of routine clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data available on request from the authors.
References
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010: https://doi.org/10.1016/j.ophtha.2009.07.017.
Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, et al. Ranibizumab for macular edema following central retinal vein occlusion. Six-month primary end point results of a phase III study. Ophthalmology. 2010: https://doi.org/10.1016/j.ophtha.2010.02.022.
Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC, et al. Ranibizumab for macular edema following branch retinal vein occlusion. Six-month primary end point results of a phase III study. Ophthalmology. 2010: https://doi.org/10.1016/j.ophtha.2010.02.021.
Heier JS, Clark WL, Boyer DS, Brown DM, Vitti R, Berliner AJ, et al. Intravitreal aflibercept injection for macular edema due to central retinal vein occlusion: two-year results from the COPERNICUS study. Ophthalmology. 2014: https://doi.org/10.1016/j.ophtha.2014.01.027.
Ogura Y, Roider J, Korobelnik JF, Holz FG, Simader C, Schmidt-Erfurth U, et al. Intravitreal aflibercept for macular edema secondary to central retinal vein occlusion: 18-month results of the phase 3 GALILEO study. Am J Ophthalmol. 2014: https://doi.org/10.1016/j.ajo.2014.07.027.
Baker CW, Glassman AR, Beaulieu WT, Antoszyk AN, Browning DJ, Chalam KV, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. J Am Med Assoc. 2019: https://doi.org/10.1001/jama.2019.5790.
Ying G, Maguire M, Daniel E, Ferris F, Jaffe G, Grunwald J, et al. Association of baseline characteristics and early vision response with 2-year vision outcomes in the Comparison of AMD Treatments Trials (CATT). Ophthalmology. 2015;122:2523–31.e1.
Bressler N, Odia I, Maguire M, Glassman A, Jampol L, MacCumber M, et al. Association between change in visual acuity and change in central subfield thickness during treatment of diabetic macular edema in participants randomized to aflibercept, bevacizumab, or ranibizumab. JAMA Ophthalmol. 2019;137:977.
Ye P, Zhu T, Zheng F, Zhou M, Fang X, Yao K. Microvascular comparison in younger and older patients with retinal vein occlusion analyzed by OCT angiography. BMC Ophthalmol. 2021: https://doi.org/10.1186/s12886-021-01931-5.
Clarkson, JG, Chuang E, Gass D, Pedroso M, Cubillas T, Duria ES, et al. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion: the central vein occlusion study group M report. Ophthalmology. 1995: https://doi.org/10.1016/S0161-6420(95)30849-4.
Gao X, Obeid A, Adam M, Hyman L, Ho A, Hsu J. Loss to follow-up in patients with retinal vein occlusion undergoing intravitreal anti-VEGF injections. Ophthalmic Surg, Lasers Imaging Retina. 2019;50:159–66.
Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, et al. Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology. 2012: https://doi.org/10.1016/j.ophtha.2011.12.005.
Thach AB, Yau L, Hoang C, Tuomi L. Time to clinically significant visual acuity gains after ranibizumab treatment for retinal vein occlusion: BRAVO and CRUISE trials. Ophthalmology. 2014: https://doi.org/10.1016/j.ophtha.2013.11.022.
Sangroongruangsri S, Ratanapakorn T, Wu O, Anothaisintawee T, Chaikledkaew U. Comparative efficacy of bevacizumab, ranibizumab, and aflibercept for treatment of macular edema secondary to retinal vein occlusion: a systematic review and network meta-analysis. Expert Rev Clin Pharmacol. 2018: https://doi.org/10.1080/17512433.2018.1507735.
Funding
The authors report no additional funding for this research.
Author information
Authors and Affiliations
Contributions
JCL was responsible for conducting the search, screening patients, analysing data and writing. TV contributed to conducting the search and analysing data. KS contributed to analysing data. CCSV contributed to the study design, interpreting results and editing. AR and RPS contributed to the study design and editing.
Corresponding author
Ethics declarations
Competing interests
RPS reports personal fees from Genentech/Roche, Alcon/Novartis, Zeiss, Bausch + Lomb, Regeneron Pharmaceuticals, Inc, Gyroscope, Asceplix and Apellis. AR reports personal fees from Alcon, Allergan, Regeneron, Samsara and Zeiss as well as research and personal fees from Genentech and Novartis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, J.C., Vatti, T., Seth, K. et al. Outcomes in patients with retinal vein occlusion with good baseline visual acuity. Eye 37, 3203–3208 (2023). https://doi.org/10.1038/s41433-023-02488-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02488-x