Abstract
Aim
To evaluate the effects of phacoemulsification on intraocular pressure (IOP) and ultrasound biomicroscope (UBM) images of filtering bleb in eyes with cataract and a previous functioning filtering bleb.
Methods
The IOPs and UBM images of filtering bleb of 24 patients (27 eyes) who underwent phacoemulsification after successful trabeculectomy were recorded at each follow-up examination and at the 12 months after phacoemulsification, respectively. Preoperative IOP and two parameters of the UBM images, including visibility of a route under the scleral flap and reflectivity inside the bleb were evaluated for an association with postoperative success rate using Kaplan–Meier survival analysis.
Results
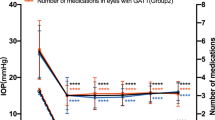
The mean IOP increased 5.50, 3.85, 3.11, 3.05, 2.79, and 2.58 mmHg after 1 day, 1 week, 1, 3, 6, and 12 months, and it was significantly higher than the preoperative IOP (P=0.000, 0.000, 0.000, 0.000, 0.000, and 0.000 respectively). There was no statistically significant difference in visibility of the route under the scleral flap and reflectivity inside the bleb before and after phacoemulsification (P=0.398, 0.096). An IOP greater than 10 mmHg, a bleb with an invisible route under the scleral flap and stronger intrableb reflectivity before phacoemulsification were associated with postoperative antiglaucomatous failure (P=0.025, 0.000, and 0.000 respectively).
Conclusions
Phacoemulsification significantly increased IOP, but had less effect on intrableb features in UBM image. Eyes with higher IOP, invisible route under scleral flap and stronger intrableb reflectivity in UBM image before phacoemulsification had greater postoperative antiglaucomatous failure.
Similar content being viewed by others
Introduction
A well-functioning filtering bleb is a successful symbol of trabeculectomy. Previous studies mostly focused on the size, height, vascularisation, vessels, and encapsulation of filtering bleb.1, 2 The recent development by Pavlin and Foster3, 4 of an ultrasound biomicroscope (UBM) makes it possible to observe the internal structure of filtering bleb and to study the relationship between its internal structure and the control of intraocular pressure (IOP).
The present study observed structural changes before and after phacoemulsification in cataract eyes that had undergone trabeculectomy. We evaluated the effects of phacoemulsification on IOP and internal structure of filtering bleb, and analysed if the features of filtering bleb in UBM image before phacoemulsification could influence the success rate of trabeculectomy after phacoemulsification.
Patients and methods
Patients
Patients were included who had undergone a previous trabeculectomy and were admitted for planned phacoemulsification combined intraocular lens implantation between October 2004 and December 2005 at the Tongren Eye Center, Tongren Hospital, Capital University of Medical Science, Beijing, People's Republic of China. The interval between trabeculectomy and phacoemulsification is longer than six months. The type of glaucoma is primary angle-closure glaucoma or primary open-angle glaucoma. The Medical Ethics Committee of the Beijing Tongren Hospital had approved the study protocol and all participants had given written informed consent.
We evaluated 27 eyes of 24 patients for whom the duration of postoperative follow up was at least 12 months. Among the 27 eyes, 19 (70.4%) were diagnosed as primary angle-closure glaucoma; eight (29.6%) were primary open-angle glaucoma. No patient required glaucoma medication. The interval between trabeculectomy and phacoemulsification ranged from 11 months to 29 months. Of the 27 eyes, antifibrosis agent was used in 22 eyes. Before phacoemulsification, IOP (measured by Goldmann tonometry) and filtering bleb ultrasound biomicroscopic image were noted. The IOP before phacoemulsification ranged from 4.0 to 19.7 mmHg and the mean IOP was 12.5±4.8 mmHg. After phacoemulsification combined intraocular lens (IOL) implantation, patients were examined at 24 h, 1 week, and 1, 3, 6, 12 months. Intraocular pressure was noted at each follow-up visit and filtering bleb ultrasound biomicroscopic image was noted at 12 months after phacoemulsification.
We defined success as the absence of glaucoma medications, bleb needling, or further glaucoma surgery to maintain IOP control after phacoemulsification.
Phacoemulsification combined IOL implantation
All phacoemulsification procedures were performed by the same surgeon. The technique and general protocol were similar for all patients. Phacoemulsification was performed with all patients under topical anaesthesia. A clear corneal incision was made away from the edge of the filtering bleb with a 3.2 mm keratome. Posterior synechiolysis and/or pupil stretching were performed as needed. Continuous circular capsulotomy was performed with capsulorhexis forceps. After hydrodissection, the nucleus was removed by phacoemulsification. The cortical remnants were irrigated and aspirated. A foldable acrylic posterior chamber IOL (AcrySof natural, Alcon laboratories, Fort Worth, TX, USA) was inserted into the capsular bag. Viscoelastic was removed as much as possible from the eye. The routine postoperative treatment included a combination of dexamethasone and tobramycin six times a day for two weeks and then the dosage was tapered until the discontinuation after six weeks.
Ultrasound biomicroscopy (UBM)
Ultrasound biomicroscopy was conducted with the UBM 840 system (Humphrey–Zeiss, San Leandro, CA, USA) at 12 months after phacoemulsification. For our measurements, the ultrasound biomicroscope was set at a 5.0 × 5.0 mm field of view with 80 dB of gain, 5 dB of gain compensation, and a 2.24–3.76 mm delay. The patients maintained a supine position during the examination. With the aid of an eyecup filled with 1.5% ethylcellulose (Scopisol) and physiologic saline, the probe scanned over the entire region of the filtering bleb in parallel with the meridian. During the scanning procedure, we evaluated: (1) visibility of a route under the scleral flap and (2) reflectivity inside the bleb. If a route could be identified under the scleral flap and could be followed along the entire scleral flap, the route was classified as visible. The reflectivity of the bleb was classified according to its similarity to the scleral reflectivity of the same ultrasound biomicroscopic image and a standard intrableb image for low reflectivity (Figure 1). The image was classified into type low, medium, and high according to the method of Yamamoto.5 All ultrasound biomicroscopy was conducted by the same researcher and UBM reading was conducted in a masked fashion.
Statistical analysis
Longitudinal comparisons of IOPs were made using the two-tailed Student's t-test for paired samples. Comparisons of routes under scleral flap and reflectivity inside the bleb before and after phacoemulsification were performed using the χ2 test. The probability of success after phacoemulsification was estimated with Kaplan–Meier survival analysis. The distribution of survival rates for preoperative factors was compared with the log-rank test. A statistics programme (SPSS 10.0 for Windows, SPSS Inc., Chicago, IL, USA) was used for analysis. A P-value of 0.05 or less was considered statistically significant.
Results
The mean IOPs before and after phacoemulsification at each followup interval are shown in Table 1. The mean IOP before phacoemulsification was 12.5±4.8 mmHg. After phacoemulsification, the mean IOP increased significantly compared with the mean IOP before phacoemulsification: by 5.5 mmHg on postoperative day 1 (P=0.000), by 3.9 mmHg after 1 week (P=0.000), by 3.1 mmHg after 1 month (P=0.000), by 3.1 mmHg after 3 months (P=0.000), by 2.8 mmHg after 6 months (P=0.000), by 2.6 mmHg after 12 months (P=0.000).
Table 2 lists the preoperative and postoperative visibility of the route under the scleral flap. There was no statistically significant difference in visibility of the route under the scleral flap before and after phacoemulsification (P=0.398).
Table 3 lists the preoperative and postoperative reflectivity inside the bleb. There was no statistically significant difference in reflectivity inside the bleb before and after phacoemulsification (P=0.096).
We defined success as the absence of glaucoma medications, bleb needling, or further glaucoma surgery to maintain IOP control after phacoemulsification. The Kaplan–Meier success rate after phacoemulsification was 77.8% at 12 months. The IOP before phacoemulsification had a statistically significant effect on the possibility of failure. A preoperative IOP greater than 10 mmHg was associated with the need for glaucoma medications or bleb needling after phacoemulsification (P=0.025). Preoperative visibility of the route under the scleral flap and reflectivity inside the bleb had effects on the propensity for failure (P=0.000, P=0.000, respectively). Invisible route under the scleral flap and/or higher reflectivity inside the bleb before phacoemulsification were associated with antiglaucomatous failure after phacoemulsification (Table 4).
Discussion
There are many studies on IOP changes after phacoemulsification in glaucoma-filtered eyes, ranging from a decrease of 0.8 mmHg to an increase of 6.6 mmHg (follow up ranging from 8 to 70 months).2, 6, 7, 8, 9 Rebolleda et al6 reported that there is a mean IOP increase of 2.04 mmHg 12 months after phacoemulsification. Klink et al2 found a statistically significant mean IOP increase of 2.05 mmHg one year after phacoemulsification. Our study showed a mean IOP increase of 2.6 mmHg 12 months after phacoemulsification, and it is slightly higher than that in above mentioned studies.
Ultrasound biomicroscopy is an important tool to observe internal structure of filtering bleb. Visibility of the route under the scleral flap and reflectivity inside the bleb are two important aspects, which evaluate the UBM image of filtering bleb. Some studies5, 10 showed that the features of the ultrasound biomicroscopic image were significantly associated with filtering bleb function. Visibility of a route under the scleral flap and reflectivity inside the bleb were highly associated with IOP control. The invisible route under scleral flap and the high-reflective bleb were found mostly in eyes with poor IOP control. The studies by Avitabile et al11, 12 showed that blebs with lower reflectivity and a visible route under the scleral flap had a lower IOP. They believed that UBM could be a useful method to study and explain the mechanisms of filtering structures and, together with IOP control, to evaluate the bleb function. In the current study, we found that before phacoemulsification the route under scleral flap is visible and reflectivity inside bleb is low in all the 11 eyes with IOP less than 10 mmHg. But in 16 eyes with IOP more than 10 mmHg, visible route under scleral flap was found in eight eyes and low reflectivity inside bleb was found in four eyes. These findings were in accordance with that by Yamamoto et al.5
The structures of filtering bleb in UBM images before and after phacoemulsification were both observed and compared in our study. Though the visible route under scleral flap became invisible or became narrower and the low reflectivity inside the bleb became high in most eyes, the changes before and after phacoemulsification did not have a statistical significance. We think the techniques of phacoemulsification, which is minimally invasive now, have less effect on the route under the scleral flap and reflectivity inside the bleb. Because filtering bleb has its own natural evolutional course, so larger sample size and control study are needed to specify the features of filtering bleb before and after phacoemulsification.
Many preoperative and perioperative factors, including preoperative IOP, time from trabeculectomy, intraoperative iris manipulation, antimetabolism use and so on were evaluated for an association with postoperative success in some previous studies.6, 7, 13, 14 But the factors such as visibility of the route under the scleral flap and reflectivity inside the bleb in UBM image before phacoemulsification were not evaluated to estimate postoperative success rate before. In our study, eyes with an IOP greater than 10 mmHg before phacoemulsification more often required medication to control IOP than eyes with an IOP of 10 mmHg or less. Our outcome were in accordance well with studies by several authors.6, 13 Eyes with visible route under scleral flap before phacoemulsification had higher success rate at 12 months after phacoemulsification than eyes with invisible route under scleral flap (P=0.000). Eyes with lower reflectivity inside bleb before phacoemulsification had less failure rate at 12 months after phacoemulsification than eyes with higher reflectivity inside bleb (P=0.000). The success of trabeculectomy after phacoemulsification was highly correlated with IOP level, visibility of the route under the scleral flap and reflectivity inside the bleb in UBM image before phacoemulsification.
Our results indicate that performing phacoemulsification after trabeculectomy may increase the IOP. Though phacoemulsification, which has the tendency to become the minimally invasive operation, has less effect on the route under the scleral flap and reflectivity inside the bleb, we can estimate the fate of glaucoma after phacoemulsification according to features of filtering bleb before phacoemulsification. In order to observe the long-term effects of phacoemulsification on filtering bleb, a longer follow-up is needed.
References
Picht G, Grehn F . Classification of filtering blebs in trabeculectomy: biomicroscopy and functionality. Curr Opin Ophthalmol 1998; 9: 2–8.
Klink J, Schmitz B, Lieb WE, Klink T, Grein HJ, Sold-Darseff J et al. Filtering bleb function after clear cornea phacoemulsification: a prospective study. Br J Ophthalmol 2005; 89: 597–601.
Pavlin CJ, Harasiewicz K, Sherar MD, Foster FS . Clinical use of ultrasound biomicroscopy. Ophthalmology 1991; 98: 287–295.
Pavlin CJ, Foster FS . Ultrasound Biomicroscopy of the Eye. Springer–Verlag: New York, 1995.
Yamamoto T, Sakuma T, Kitazawa Y . An ultrasound biomicroscopic study of filtering blebs after mitomycin C trabeculectomy. Ophthalmology 1995; 102: 1770–1776.
Rebolleda G, Munoz-Negrete FJ . Phacoemulsification in eyes with functioning filtering blebs: a prospective study. Ophthalmology 2002; 109: 2248–2255.
Chen PP, Weaver YK, Budenz DL, Feuer WJ, Parrish RK II . Trabeculectomy function after cataract extraction. Ophthalmology 1998; 105: 1928–1935.
Wygnanski-Jaffe T, Barak A, Melamed S, Glovinsky Y . Intraocular pressure increments after cataract extraction in glaucomatous eyes with functioning filtering blebs. Ophthalmic Surg Lasers 1997; 28: 657–661.
Derbolav A, Vass C, Menapace R, Schmetterer K, Wedrich A . Long-term effect of phacoemulsification on intraocular pressure after trabeculectomy. J Cataract Refract Surg 2002; 28: 425–430.
Jinza K, Saika S, Kin K, Ohnishi Y . Relationship between formation of a filtering bleb and an intrascleral aqueous drainage route after trabeculectomy: evaluation using ultrasound biomicroscopy. Ophthalmic Res 2000; 32: 240–243.
Avitabile T, Russo V, Uva MG, Marino A, Castiglione F, Reibaldi A . Ultrasound-biomicroscopic evaluation of filtering blebs after laser suture lysis trabeculectomy. Ophthalmologica 1998; 212 (Suppl 1): 17–21.
Avitabile T, Uva MG, Russo V, Ott JP, Paulick B, Reibaldi A . Evaluation of the filtering bleb using ultrasound biomicroscopy. Klin Monatsbl Augenheilkd 1998; 212: 101–105.
The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol 2000; 130: 429–440.
Crichton AC, Kirker AW . Intraocular pressure and medication control after clear corneal phacoemulsification and AcrySof posterior chamber intraocular lens implantation in patients with filtering blebs. J Glaucoma 2001; 10: 38–46.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, X., Zhang, H., Li, S. et al. The effects of phacoemulsification on intraocular pressure and ultrasound biomicroscopic image of filtering bleb in eyes with cataract and functioning filtering blebs. Eye 23, 112–116 (2009). https://doi.org/10.1038/sj.eye.6702981
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702981
Keywords
This article is cited by
-
Effect of phacoemulsification surgery on intraocular pressure and function of bleb after trabeculectomy
International Ophthalmology (2021)
-
MIGS: therapeutic success of combined Xen Gel Stent implantation with cataract surgery
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)
-
Long-term effect of phacoemulsification on trabeculectomy function
Eye (2015)
-
The effects of phacoemulsification on intraocular pressure and the ultrasound biomicroscopic image of filtering bleb in eyes with cataract and functioning filtering blebs: comparison of the Tongren Eye Center and Peking University Eye Center data
Eye (2010)