Abstract
Purpose
Open-sky cataract extraction during triple procedure can be associated with higher risk of complications owing to the missing counterbalance by the cornea. Herein, we present a fast and easy technique for visualization of the anterior chamber and the lens in eyes with opaque corneas planed for triple procedure.
Materials and methods
Four patients with corneal oedema due to Fuchs' endothelial dystrophy and cataract underwent triple procedure. As the anterior chamber view was limited, the central 7.0 mm of the cornea was marked. Then, 60–80% of the corneal thickness was removed by lamellar dissection and filled with hydroxypropylmethylcellulose. Continuous curvilinear capsulorhexis (CCC) and phacoemulsification with intraocular lens implantation through a corneoscleral tunnel were then performed and at the end the remaining corneal tissue was excised and the donor tissue fixed with a single running continuous suture.
Results
Lamellar corneal dissection enhances the anterior chamber view and CCC can be performed under stable anterior chamber condition. Phacoemulsification via sclerocorneal tunnel could be easily performed under good anterior chamber view in all cases. The operation time was 60–75 min in all cases.
Conclusion
Lamellar corneal dissection in opaque corneas before cataract extraction is a useful technique for enhancing anterior chamber view in cases of triple procedure.
Similar content being viewed by others
Introduction
In 1981, Richard Lindstrom1 performed penetrating keratoplasty with extracapsular cataract extraction and intraocular lens (IOL) implantation in a combined procedure. After the continuous curvilinear capsulorhexis (CCC) was introduced in phacoemulsification, it was adopted in triple procedure.2 A well-performed CCC increases the safety and efficacy of cataract surgery, especially phacoemulsification.
Several authors perform cataract extraction via sclerocorneal tunnel phacoemulsification before trepanation. This technique can only be performed in eyes with sufficient corneal clarity.3, 4, 5
In cases of corneal opacity without sufficient anterior chamber view and planed triple procedure, open-sky CCC must be performed. The disadvantage of the open-sky technique is the missing counterbalance by the cornea and a higher risk for complications, including radial tear, posterior capsule rupture, choroidal effusion, and even expulsive haemorrhage.4, 6 Caporossi et al7 suggest to perform counterpressure to the centre of the lens with a large spatula during CCC to oppose the posterior pressure.
Herein, we describe an easy technique to visualize anterior chamber even in cases with severe corneal oedema using lamellar corneal dissection. Phacoemulsification can be easily performed under good conditions in combination with penetration keratoplasty.
Materials and methods
Four patients with corneal oedema owing to Fuchs Endothelial Dystrophy and cataract underwent triple procedure (cataract extraction, IOL implantation, and penetrating keratoplasty) for visual rehabilitation. All patients were operated by one surgeon (NA).
Surgical technique
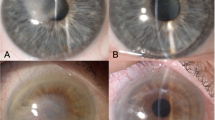
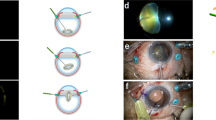
The central cornea was marked with a 7.0 mm marker. A stab knife (Sharpoint, USA) was then used to perform a corneal incision of approximately 60–80% (Figure 1). The length of the incision was 40°. Thereafter, a small pocket was created and then a Maloney–Dart lamellar dissector (Duckworth-Kent, UK) used for anterior corneal stroma dissection (Figure 2). This procedure took about 10–15 min. Once the stromal tissue was removed (Figure 3), hydroxypropylmethylcellulose (HPMC, Visicrom, Croma Pharma, Austria) was applied into the recipient bed (Figure 4).
Then, a 2.5 mm corneoscleral tunnel was performed at the 11 o'clock position, vision blue® was injected into the anterior chamber, and washed out 45 s later with BSS. Provisc (Alcon) was then injected into the anterior chamber and a 28-G needle used to perform CCC (Figure 5). After finishing CCC, uncomplicated phacoemulsification was performed, IOL implanted into the bag, one 10-0 nylon suture was used to close the tunnel, and then the remaining corneal recipient tissue was excised with a stab knife and keratoplasty scissors. At the end, a 7.25 mm donor tissue was fixed to the recipient bed using one single continuous running suture (10-0 nylon).
Results
The lamellar dissection of the cornea takes 10–15 min and is an easy procedure, as a stromal removal down to Descemets' membrane is not necessary. Corneal perforation or any other intraoperative complication did not occur during lamellar dissection.
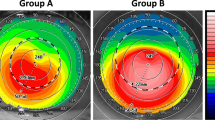
Anterior chamber and capsular view is very good after the application of HPMC into the corneal bed throughout the entire operation, which took between 60 and 75 min in all four cases.
Discussion
Triple procedures have been performed for the last 40 years.8, 9, 10, 11 The advantage of such a procedure is the faster visual rehabilitation after only one procedure.
CCC and phacoemulsification have been used for more than 15 years in cataract surgery, as they are associated with less intraoperative complications than can-opener capsulotomy,12 especially in combination with triple procedures and posterior chamber IOL implantation.7
Visualization of the anterior capsule and the lens can be difficult, if the corneal clarity is not sufficient. Vision blue has been introduced recently for better visualization in cases of corneal opacities and open-sky CCC.13
The disadvantage of open-sky CCC is the instable situation of the globe including a higher risk for radial tear during capsulorhexis, posterior capsule tear leading to vitreous loss, as the counterpressure from the cornea is missing.4, 6
Senoo introduced deep lamellar keratoplasty in clear corneas with healthy endothelium in combination with posterior chamber IOL implantation.14 In clear corneas, the surgeon can start with the phacoemulsification first and then perform lamellar keratoplasty or vice versa.
Herein, we present a similar technique of lamellar dissection for better visualization during triple procedure to enable a good anterior chamber view, even in very opaque corneas. Capsulorhexis and phacoemulsification with a stable anterior chamber could be both performed under good view and no intraoperative complications were observed. As the cornea is oedematous and a depth of 60–80% is targeted, lamellar preparation is easy and the risk of perforation low and did not exceed an additional time of 15 min in all cases. A microkeratome as used for automated lamellar keratoplasty might be useful in reducing the operation time and creating a smooth wound edge.15
In contrast to the closed system for triple procedure presented by Nardi et al,16 who transplanted a donor tissue before cataract extraction and then replaced the first graft by a second transplant, the surgery time is shorter and a second corneal tissue is not necessary.
Caporossi et al describe good success rates for open-sky CCC in triple procedures using a large spatula for performing counterpressure at the centre of the lens, but the technique has the disadvantage that it cannot be combined with phacoemulsification, as the globe is not closed.
In summary, stromal dissection in cases of opaque corneas can give better anterior chamber view, stable intraocular situation, and eventually reduce intraocular complications in eyes undergoing phacoemulsification and penetrating keratoplasty.
References
Lindstrom RL, Harris WS, Doughman DJ . Combined penetrating keratoplasty, extracapsular cataract extraction, and posterior chamber lens implantation. J Am Intraocular Implant Soc 1981; 7: 130–132.
Hofbauer JD, Levenson J . Capsulorhexis for cataract extraction during keratoplasty. Cornea 1992; 11: 273–274.
Malbran ES, Malbran E, Buonsanti J, Adrogue E . Closed-system phacoemulsification and posterior chamber implant combined with penetrating keratoplasty. Ophthalmic Surg 1993; 24: 403–406.
Robin H, Hannouche D, Hoang-Xuan T . Triple procedure with phacoemulsification prior to grafting. J Fr Ophthalmol 1997; 20: 701–703.
Groden LR . Continuous tear capsulotomy and phacoemulsification cataract extraction combined with penetrating keratoplasty. Refract Corneal Surg 1990; 6: 458–459.
McKillop BR . Continuous tear capsulotomy and phacoemulsification during penetrating keratoplasty. Refract Corneal Surg 1991; 7: 329–330.
Caporossi A, Traversi C, Simi C, Tosi GM . Closed-system and open-sky capsulorhexis for combined cataract extraction and corneal transplantation. J Cataract Refract Surg 2001; 27: 990–993.
Katzin HM, Meltzer JF . Combined surgery for corneal transplantation and cataract extraction. Am J Ophthalmol 1966; 62: 556–560.
Taylor DM . Keratoplasty and intraocular lenses. Ophthalmic Surg 1976; 7: 31–42.
Taylor DM, Khaliq A, Maxwell R . Keratoplasty and intraocular lenses: current status. Ophthalmology 1979; 86: 242–255.
Taylor DM, Khaliq A . Keratoplasty and intraocular lenses: follow-up study. Ophthalmic Surg 1977; 8: 49–57.
Neuhann T . Theory and surgical technic of capsulorhexis. Klin Monatsbl Augenheilkd 1987; 190: 542–545.
Ozkiris A, Arslan O, Cicik E, Koyluoglu N, Evereklioglu C . Open-sky capsulorrhexis in triple procedure: with or without trypan blue? Eur J Ophthalmol 2003; 13: 764–769.
Senoo T . Combined surgery with deep lamellar keratoplasty. Semin Ophthalmol 2001; 16: 126–136.
Lyle WA, Jin GJ . Hyperopic automated lamellar keratoplasty: complications and visual results. Arch Ophthalmol 1998; 116: 425–428.
Nardi M, Giudice V, Marabotti A, Alfieri E, Rizzo S . Temporary graft for closed-system cataract surgery during corneal triple procedures. J Cataract Refract Surg 2001; 27: 1172–1175.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial interest in any product or technique presented in this study
Presented at the XXIII annual meeting of the European Society of Cataract and Refractive Surgery on 12th September 2005 in Lisbon
Rights and permissions
About this article
Cite this article
Ardjomand, N., Fellner, P., Moray, M. et al. Lamellar corneal dissection for visualization of the anterior chamber before triple procedure. Eye 21, 1151–1154 (2007). https://doi.org/10.1038/sj.eye.6702409
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702409