Abstract
Purpose
To compare the effectiveness of limbus- and fornix-based conjunctival flaps in patients undergoing trabeculectomy with mitomycin-C augmentation.
Methods
A retrospective review of the records of 71 consecutive eyes of 59 patients who underwent trabeculectomy with mitomycin C. All the patients had at least 6 months of follow-up. The first 35 eyes underwent surgery with a limbal-based flap, whereas all subsequent surgeries were by fornix-based procedures.
Results
No significant difference was detected between the groups with regard to patient demographics, preoperative visual field and intraocular pressure parameters, postoperative intraocular pressures at day 1, months 1, 3, and 6 postoperatively, need for intervention, need for supplementary glaucoma medication, and final visual acuity. There were four cases of overdrainage and hypotony in the limbal-based group, whereas none occurred in the fornix-based group. In all 83% percent of eyes in the limbal-based group achieved intraocular pressures off medication of less than 18 mmHg, whereas 94% of the fornix based group obtained such IOP control. One patient in the limbal-based group developed late postoperative endophthalmitis.
Conclusion
Trabeculectomy with MMC augmentation is a safe and effective procedure for reduction of IOP and visual rehabilitation whether a fornix- or a limbal-based conjunctival flap is utilised. In this series, there was a greater risk of excessive drainage with subsequent hypotonous complications when surgery was undertaken by a limbal-based procedure.
Similar content being viewed by others
Introduction
The surgical management of glaucoma has progressed and evolved throughout the years. With advances in surgical technique, such as the use of adjunctive antifibrotic or antimetabolic agents and the placement of releasable sutures, glaucoma surgery has become a more reliable and predictable undertaking.1, 2, 3 Several studies have previously compared the use of fornix vs limbal-based conjunctival flaps in pure trabeculectomy cases,4, 5, 6, 7, 8 cases undergoing concurrent extracapsular cataract extraction surgery,9 and trabeculectomy combined with phacoemulsification procedures (phaco-trabeculectomy).10, 11, 12, 13 We aim to present outcome data comparing the two flap designs in trabeculectomy procedures carried out under the care of one glaucoma surgeon.
Methods
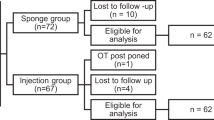
All trabeculectomies performed by an experienced glaucoma surgeon (AWK) or by a trainee surgeon under the direct supervision of the consultant between 23rd November 2000 and 28th August 2002 were included in the study.
All the clinical records of patients who had had a trabeculectomy procedure during the study period were reviewed. Data collection was carried out by two of the authors (AA and VP). Pre- and postoperative data were retrieved on the patients including patient demographics, preoperative glaucoma status (visual fields parameters, intra ocular pressures, medications), visual acuities, and postoperative progress. Patients with a follow-up of less than 6 months were excluded.
In the first 43 eyes (group LB), the procedure was carried out utilising a limbal-based flap and subsequently all cases were carried out with a fornix-based flap procedure (group FB). The change from limbal- to fornix- based flaps represented an alteration in surgical technique by the surgeon.
Operative procedure
Anaesthetic was by either general anaesthesia or by a peribulbar technique. The eye was sterily prepared and draped with an occlusive dressing to isolate lash follicles. A Clarks lid speculum and a 7/0 silk corneal traction suture was placed for ocular stabilisation. For a fornix-based procedure the incision was made in the conjunctiva from 1100 to 0100 hours at the limbus with wide blunt dissection to free Tenons and conjunctiva from sclera posteriorly to a distance of approximately 8–10 mm. For a limbus-based operation a 10 mm incision was made through conjunctiva and Tenon capsule approximately 10 mm from the limbus. The conjunctiva and Tenons were dissected anterior to the limbus being careful to avoid a conjunctival button hole, and posteriorly to enlarge the potential area of drainage and encourage posterior aqueous drainage.
With both techniques meticulous haemostasis was undertaken by monopolar diathermy. A cellulose sponge soaked in mitomycin-C (concentration varying between 0.05 and 0.4 mg/ml) was then applied over the area of the proposed scleral flap and underneath the conjunctiva and Tenons capsule for a time varying between 30 s and 4 min. The concentration and duration of mitomycin C application were based upon the preoperative assessment of patient risk factors and the peroperative condition of the conjunctiva and Tenons capsule (eg thickness and friability). Care was taken to avoid contact with the free edges of the conjunctiva. Copious irrigation with balanced salt solution was then applied to wash out any residual MMC solution.
A paracentesis was created and a partial thickness 4 mm × 3 mm rectangular trapezoid scleral flap was fashioned using a diamond blade initially and then a crescent blade. The anterior chamber was then entered with a diamond blade at the base of the scleral flap incision.
An incision was made in the base of the scleral flap into the anterior chamber and a Kelly-Descemet punch was used to create a sclerectomy. An iridectomy was performed using Vannas scissors. The scleral flap was closed with two releasable 10/0 nylon sutures and one fixed suture central to the posterior lip of the flap. Tension on the individual sutures was tailored to each individual case to allow fluid flow through the flap on reformation of the anterior chamber via the paracentesis.
For fornix-based procedures the conjunctiva was closed with two 10/0 nylon purse string sutures with or without placement of mattress sutures. For limbal-based procedures the conjunctival incision was closed with a single running 10/0 vicryl suture. ‘Water tightness’ of wound closure was checked by the application of topical 2% fluorescein to the eye and insufflation of the anterior chamber with balanced salt solution.
A subconjunctival injection of 3 mg Zinacef® and 2 mg Betnesol® was given at the end of the procedure distant to the site of the trabeculectomy and a pad and patch was applied.
Postoperative management
All patients were treated with topical Maxidex® six times daily for at least 3 months in addition to topical chloramphenicol 1% four times daily for the first 2 weeks. The steroid regimen was altered appropriately to encourage satisfactory bleb morphology.
Postoperatively, if the bleb was seen to be shallow or the intraocular pressure raised, ocular massage was applied to increase flow of aqueous into the bleb and reduce intraocular pressure. If conservative measures did not achieve good aqueous outflow, one or both of the releasable sutures was removed under topical anaesthesia.
Postoperative subconjunctival injection of 5-fluorouracil was given if the bleb appeared excessively vascularised or inflamed. Topical glaucoma medications were given if the IOP was deemed to be too high with a significant risk of glaucomatous progression and if no further bleb modification strategies were feasible. If, despite the removal of both releasable sutures and ocular massage, the bleb was felt to be under draining (compromised aqueous outflow) with associated flat bleb morphology a needling with 5-fluorouracil subconjunctival injection was undertaken.
Patients were reviewed on the first postoperative day and follow-up appointments were made for 1 week, 2 weeks, 1 month, 2 months, 3 months, and 6 months postoperatively in the routine cases and at other times if deemed clinically necessary. Data were collected for the day one postoperative visit and for the 1-week, 1-month, 3-months and 6-month visit. Data were collected beyond this time if available.
Statistics
All statistics were carried out utilising SPSS® for Windows 9.0.
Complication and intervention rates were compared by x2 analysis while other data were compared by t-test.
Results
In Group LB there were 35 eyes of 27 patients, 13 male and 14 female. In Group FB there were 36 eyes of 32 patients, 15 male and 17 female. The mean age in Group LB was 69.74 years (range 23–85). The mean age in Group FB was 69.83 years (range 23–85). There was no significant difference between the ages of the two groups (P=0.943).
There was no statistically significant difference in the preoperative Humphreys visual field parameters or other patient characteristics between the two groups.
Table 1 displays and statistically compares the pre and postoperative intraocular pressure data between the two groups at each time point.
There was no statistical difference between the preoperative intraocular pressures of the two groups (P=0.163). Comparing postoperative intraocular pressures there was no statistical difference between groups LB and FB at day 1 (P=0.486), day 7 (P=0.069), 1 month (P=0.229), 3 months (P=0.683), and 6 months (P=0.747).
Comparing Humphreys 24-2 visual fields at 6 months postoperatively, there was no statistically significant difference between the two groups with regards to their mean deviation or the pattern standard deviation (P=0.163 and 0.255, respectively).
Interventions
In all, 22 eyes (62.9%). of Group LB required intervention whereas 24 eyes (66.7%) in Group FB required postoperative intervention (Table 2).
Group LB
Three cases experienced leaks from the conjunctival closure. Two of these cases settled conservatively with tamponade from a bandage contact lens while one case required return to theatre for suture of the conjunctival leak.
In 11 cases underdrainage into the bleb required removal of releasable sutures. Of these, two cases needed removal of both sutures whereas in nine cases only one suture was removed.
In four cases the bleb was overdraining, leading to complications related to hypotony. In all cases the over drainage occurred within the first postoperative month. In one case the anterior chamber (AC) was excessively shallow requiring return to theatre for reformation of AC with viscoelastic under topical anaesthesia. One case of overdrainage resolved with conservative measures utilising a pressure pad and dental roll to exert external tamponade. In the remaining two cases autologous blood was injected, one of these cases requiring three injections.
One case developed infective blebitis and endophthalmitis 2 years after initial surgery with a poor visual recovery (Snellen vision at final follow-up 6/60).
Group FB
Four cases experienced leaks from the conjunctival closure. All these cases settled conservatively with tamponade from a bandage contact lens.
There were no cases of overdrainage.
In 12 cases underdrainage into the bleb required removal of releasable sutures. Of these, eight cases needing removal of both sutures whereas in four cases only one suture was removed.
There was no statistically significant difference between the two groups with regard to the need for postoperative intervention or complication rate (P=0.901 and 0.882, respectively).
Reduction in IOP
There was a significant reduction in IOP when comparing preoperative IOPs with IOPs at each time scale (Tables 3 and 4).
Group LB achieved a mean reduction of IOP of 53.2% (standard deviation 20.12, standard error of mean 3.40). Group FB achieved a mean reduction of IOP of 48.2% (standard deviation 19.59, standard error of mean 3.31). There was no statistically significant difference between the two groups with regard to percentage of IOP reduction (P=0.302).
Success rates as classified by various criteria are shown in Table 5. There was no statistical difference between the two groups with regard to success (P=0.761).
In both groups there was a significant reduction in IOP from preoperative levels at 6 month follow-up. The mean IOP reduction in group LB was 14.22 mmHg (95% confidence interval 11.46–16.98) (P<0.001). The mean reduction in group FB was 11.71 mmHg (95% confidence interval 9.52–13.89) (P<0.001).
Mitomycin-C
Dosages of MMC used were arbitrarily calculated by multiplying the concentration of MMC (mg/ml) applied by time of application (minutes). The mean MMC dosage in group LB was 0.253 mg/ml/min, while the mean MMC dosage in group FB was 0.206 mg/ml/min. There were no statistically significant differences between the MMC usage between the groups (P=0.682).
There was no statistically significant difference between the total MMC dosage when comparing the patients who experienced leaks to those who did not (P=0.523). There was no statistically significant difference between the total MMC dosage when comparing the patients who experienced overdrainage to those who did not (P=0.226).
Discussion
This study reports on the results of a moderately sized series of trabeculectomy procedures with mitomycin-C augmentation. It offers a retrospective, nonrandomised comparison of consecutive fornix- and limbal-based conjunctival flaps. All the surgeries were performed under the care of one surgeon and on a mainly Caucasian population; thus, our results may not be applicable to patient populations consisting of other ethnic backgrounds.
In all the eyes studied both the limbal and fornix-based conjunctival flap trabeculectomies had significant improvements in IOP throughout the postoperative period up to their 6-month follow-up (P<0.001 for both groups). In total, 83% of eyes in the limbal-based group achieved intraocular pressures off medication of less than 18 mmHg whereas 94% of the fornix-based group obtained such IOP control.
We found no significant differences between the two groups with regard to any of the parameters measured. Intraocular pressures and the success rates were equivalent between groups. This finding is in agreement with previous studies of trabeculectomy and combined cataract surgery and isolated trabeculectomy that also found no difference between the two methods of conjunctival flap.5, 8, 9, 10, 11, 12, 13 Most of these studies addressed unaugmented procedures5, 9, 11 or procedures with supplementary subconjunctival 5-fluorouracil injection.8, 13 To the best of our knowledge, only three previous studies have compared fornix- vs limbal-based surgery with MMC augmentation.10, 12, 14 One small study by Brinker and Kessing6 found that unaugmented fornix-based trabeculectomy was statistically superior to limbal-based trabeculectomy with regards to success rate, bleb morphology, and the need for supplementary medical treatment.
Murchison and Shields9 presented the results of fornix- vs limbal-based conjunctival flaps in 47 eyes. The patients in their series underwent extracapsular cataract extraction and trabeculectomy without any 5-FU or MMC. They found no difference with regard to visual acuity, final IOP, or number of medications at the end of follow-up. They did, however, find a few minor differences between their two groups, describing a slightly increased rate of pressure spikes on postoperative days 1 and 2 in those patients who had a fornix-based flap.
Shingleton and colleagues13 prospectively assessed the effectiveness of limbus- and fornix-based conjunctival flaps of the fellow eyes of the same patients undergoing combined trabeculectomy with phacoemulsification and subconjunctival 5-FU injection. They found that both techniques were equally efficacious at improving visual acuity and lowering IOP.
Care must be taken when attempting to extrapolate data from studies addressing combined cataract and trabeculectomy procedures to trabeculectomy procedures alone. The stimulus for wound healing is thought to be very different in eyes having combined procedures.15 In addition, the construction of the internal sclerostomy and stresses placed on the scleral flap and tunnel during the combined procedure will inevitably be different.
In our series there was no difference between the two groups with regard to the incidence of leakage from the conjunctival incision, the need for postoperative subconjunctival 5-FU injection, or the need for needling. We did find, however, that an overdraining filtering bleb occurred in four cases in the limbal-based group whereas this did not occur in the fornix-based group. Three of these cases developed significant hypotonous complications with visual loss; two developed maculopathy and one developed ‘kissing’ ciliochoroidal detachments.
This finding has not been noted before in the literature and the authors are unsure as to its exact significance but it may represent the increased area of dissection and MMC application when the initial conjunctival incision was distant from the limbus. This increased drainage area may allow excessive aqueous outflow to occur with subsequent hypotony. The dissection space associated with the fornix-based flap may not extend as far as posteriorly and thus limit drainage, thereby facilitating controlled filtration and pressure reduction.
Previous studies have also reported a difference in wound leaks between fornix- and limbal-based procedures with MMC utilisation; however, their results have been contradictory. Tezel et al16 found more leaks in their fornix-based group whereas Lemon et al10 reported a higher incidence in the limbal-based group. A recent study by Wells et al14 found a greater risk of cystic bleb formation, late hypotony, and bleb-related infection among patients undergoing limbal-based procedures.
Patients with both limbus- and fornix-based surgeries achieved excellent reductions in IOP, with approximately 83% of patients achieving an IOP off medication of less than 18 mmHg and in the limbal-based group and 94% reaching this level in the fornix-based group.
Fornix-based procedures may be technically less challenging particularly when operating on a patient with scarred conjunctiva. They may also facilitate better visualisation of the operative field with subsequently greater ease of scleral flap formation. Furthermore, it may be easier to dissect the subconjunctival/sub-Tenons space in a posterior direction (as with a fornix-based flap) rather than anteriorly towards the limbus (as with a limbal-based flap) thus potentially reducing the risks of conjunctival ‘button-holing’. A limbal incision may, however, be detrimental in that it may lead to more exposure of the cornea to potentially toxic effects of any applied MMC than if the incision was placed distant to the limbus.17, 18, 19
With a relatively short follow-up of 6 months, it is difficult to comment on late complications and the potential for any difference manifesting between the two groups after more extended data collection. One patient in the limbal-based group developed endophthalmitis after 2 years of follow-up; however, as follow-up in our series is limited, interpretation of this isolated finding is impossible.
One criticism of this study is that it is retrospective; however, the use of serial consecutive cases to compare the two techniques of conjunctival flap formation should eliminate bias with regard to selection criteria and choice of operation for each case. A further concern is that there were some patients included in the data analysis who had both eyes operated upon, thus potentially resulting in some degree of bias due to the presence of nonindependent samples. It is also important to acknowledge that there may have been other subtle alterations to technique, such as increased attention to detail of wound closure with the change in surgical approach that may have had some effect on postoperative course.
In conclusion, it appears that in this study trabeculectomy with MMC augmentation is a safe and effective procedure for reduction of IOP and visual rehabilitation whether a fornix- or limbal-based conjunctival flap is utilised. There may, however, be a greater risk of excessive drainage with subsequent hypotonous complications when surgery is undertaken by a limbal-based procedure. Fornix-based surgery may be technically easier; however, equivalent results between the two study groups suggest that individual surgeon's comfort is a key factor in dictating as to which method is adopted.
References
Palmer SS . Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology 1991; 98: 317–321.
Skuta GL, Beeson CC, Higginbotham EJ, Lichter PR, Musch DC, Bergstrom TJ et al. Intraoperative mitomycin vs post-operative 5-Fluorouracil in high risk glaucoma filtering surgery. Ophthalmology 1992; 99: 438–444.
Kitazawa Y, Kawase K, Matsushita H, Minabe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch. Ophthalmol 1993; 77: 693–697.
Shuster JN, Krupin T, Kolker AE, Becker B . Limbus- v fornix-based conjunctival flap in trabeculectomy. A long-term randomized study. Arch Ophthalmol 1984; 102: 361–362.
Traverso CE, Tomey KF, Antonios S . Limbal- vs fornix-based conjunctival trabeculectomy flaps. Am J Ophthalmol 1987; 104: 28–32.
Brincker P, Kessing SV . Limbus-based versus fornix-based conjunctival flap in glaucoma filtering surgery. Acta Ophthalmol (Copenh) 1992; 70: 641–644.
Khan AM, Jilani FA . Comparative results of limbal based versus fornix based conjunctival flaps for trabeculectomy. Indian J Ophthalmol 1992; 40: 41–43.
el Sayyad F, el-Rashood A, Helal M, Hisham M, el-Maghraby A . Fornix-based versus limbal-based conjunctival flaps in initial trabeculectomy with postoperative 5-fluorouracil: four-year follow-up findings. J Glaucoma 1999; 8: 124–128.
Murchison Jr JF, Shields MB . Limbal-based vs fornix-based conjunctival flaps in combined extracapsular cataract surgery and glaucoma filtering procedure. Am J Ophthalmol 1990; 109: 709–715.
Lemon LC, Shin DH, Kim C, Bendel RE, Hughes BA, Juzych MS . Limbus-based vs fornix-based conjunctival flap in combined glaucoma and cataract surgery with adjunctive mitomycin C. Am J Ophthalmol 1998; 125: 340–345.
Stewart WC, Crinkley CM, Carlson AN . Fornix- vs limbus-based flaps in combined phacoemulsification and trabeculectomy. Doc Ophthalmol 1994; 88: 141–151.
Berestka JS, Brown SV . Limbus- versus fornix-based conjunctival flaps in combined phacoemulsification and mitomycin C trabeculectomy surgery. Ophthalmology 1997; 104: 187–196.
Shingleton BJ, Chaudhry IM, O'Donoghue MW, Baylus SL, King RJ, Chaudhry MB . Phacotrabeculectomy: limbus-based versus fornix-based conjunctival flaps in fellow eyes. Ophthalmology 1999; 106: 1152–1155.
Wells AP, Cordeiro MF, Bunce C, Khaw OT . Cystic bleb formation and related complications in limbus-versus fornix-based conjunctival flaps in paediatric and young adult trabeculectomy with mitomycin C. Ophthalmology 2003; 110: 2192–2197.
Siriwardena D, Kotecha A, Minassian D, Dart JK, Khaw PT . Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol 2000; 84: 1056–1057.
Tezel G, Kolker AE, Kass MA, Wax MB . Comparative results of combined procedures for glaucoma and cataract: limbus-based versus fornix-based conjunctival flaps. Ophthalmic Surg Lasers 1997; 28: 551–557.
Wu KY, Hong SJ, Huang HT, Lin CP, Chen CW . Toxic effects of mitomycin-C on cultured corneal keratocytes and endothelial cells. J Ocul Pharmacol Ther. 1999; 15: 401–411.
Morrow GL, Stein RM, Heathcote JG, Ikeda-Douglas JV, Feldman F . Ocular toxicity of mitomycin C and 5-fluorouracil in the rabbit. Can J Ophthalmol. 1994; 29: 268–273.
Manche EE, Afshari MA, Singh K . Delayed corneal epitheliopathy after antimetabolite-augmented trabeculectomy. J Glaucoma 1998; 7: 237–239.
Author information
Authors and Affiliations
Corresponding author
Additional information
No research funding. No proprietary interests.
Rights and permissions
About this article
Cite this article
Alwitry, A., Patel, V. & King, A. Fornix vs limbal-based trabeculectomy with mitomycin C. Eye 19, 631–636 (2005). https://doi.org/10.1038/sj.eye.6701587
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701587
Keywords
This article is cited by
-
Analysis of risk factors and ocular hypotony characteristics in choroidal detachment after penetrating glaucoma surgery
International Ophthalmology (2022)
-
The effect of trabeculectomy on contrast sensitivity, corneal topography and aberrations
International Ophthalmology (2019)
-
Persistent hypotony after trabeculectomy: incidence and associated factors in the Collaborative Bleb-Related Infection Incidence and Treatment Study
Japanese Journal of Ophthalmology (2016)
-
Limbus- Versus Fornix-Based Trabeculectomy for Open-Angle Glaucoma Eyes with Prior Ocular Surgery: The Collaborative Bleb-Related Infection Incidence and Treatment Study
Scientific Reports (2015)
-
Early bleb leak after trabeculectomy and prognosis for bleb failure
Eye (2009)