Abstract
Germinomas constitute 0.1–3.4% of all intracranial tumours1 and 90% affect patients less than 20 years old. Although they are relatively aggressive tumours, which commonly invade the surrounding tissue and seed within the central nervous system, they are very radiosensitive and carry a favourable prognosis. We describe a 19-year-old man who presented with bilateral visual failure secondary to a germinoma with synchronous involvement of the pineal gland and the suprasellar region. Radiotherapy restored his vision almost back to normal.
Similar content being viewed by others
Main
Case report
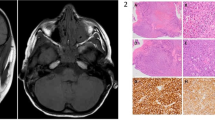
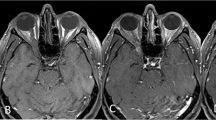
A 19-year-old man presented with a 5-month history of progressive bilateral visual impairment. He did not complain of any other symptoms. There was no family history of visual failure and no history of drug abuse or exposure to toxins. Visual acuity was counting fingers on the right and 6/24 on the left. There was a right afferent pupillary defect. Eye movements were normal. Dilated fundus examination revealed bilateral pale optic disks but normal macula and retina. Slit lamp examination was normal. Intraocular pressures were within the normal range. General clinical examination was unremarkable and there were no other abnormal neurological signs. An MRI scan of the brain with gadolinium showed abnormal contrast enhancement of the suprasellar region and pineal gland (Figure 1). The radiological findings were consistent with intracranial germinoma. An MRI scan of the spinal cord was normal, and ultrasound of the scrotum and abdomen were unremarkable. His routine bloods and chest X-ray were normal. Serum angiotensin-converting enzyme (ACE) was normal, and autoantibody screen was negative. His alpha-fetoprotein (AFP) and human chorionic gonadotrophin (HCG) in the blood and cerebrospinal fluid (CSF) were normal. His CSF was acellular with normal opening pressure, protein and glucose. Visual evoked potentials were reduced in amplitude, but not delayed, that is, compatible with bilateral optic neuropathy. An electroretinogram was normal.
He received cranio-spinal radiotherapy to a dose of 30 Gy in 20 fractions, with a further 24 Gy in 15 fractions to the tumour bed. His visual acuity improved gradually and 12 months later was 6/6 (right) and 6/9 (left). Two repeated MRI scans—2 and 8 months after radiotherapy—of the brain and spinal cord with gadolinium were normal. There has been no recurrence of his symptoms after 15 months follow-up.
Comment
Germinomas arise because of neoplastic changes of germ cells during embryonic development. They are the most common intracranial germ cell tumours and are histologically indistinct from testicular seminoma. Most germinomas arise in the midline axis from the supraseller cistern to the pineal region,2, and visual failure is a common presentation. The mechanism involved is presumably infiltrative. They usually affect young patients (< 20 years) with peak age at 10–12 years. Men are more likely to develop a geminoma (male/female 4 : 1). MRI scan of the brain with gadolinium is the recommended imaging.3 Germinoma is usually so small that it is hard to see on unenhanced MRI, but it brightens prominently and homogeneously with contrast. Multiple lesions are seen in almost 50% of cases.
The role of surgery, beyond biopsy for tissue diagnosis, remains controversial. Surgical resection exposes the patient to the operative risks and the possibility of regional tumour dissemination. Germinomas are exquisitely sensitive to radiotherapy. The presence of a relatively homogeneous, well-circumscribed, extra-axial, enhancing pineal region mass in a young male is so characteristic of a germinoma that diagnostic radiotherapy can be justified.4 Germinomas characteristically infiltrate locally, and spread by dissemination through the craniospinal and subarachnoid spaces. MRI scan of the entire neuraxis is necessary to search for CSF dissemination. HCG is only occasionally elevated with central nervous system germinomas, while the level of AFP is rarely elevated. Elevated levels of HCG and AFP are more closely correlated with malignant germ cell tumours such as embryonal carcinoma, endodermal sinus tumours, and choriocarcinoma. Spinal irradiation is recommended to cover for possible CSF invasion. As a consequence of improving the means of diagnosis and radiotherapy, the current survival rate of patients with germinoma is 90% after a median follow-up of 5 years, and a 20-year survival rate of 80% has been reported.5
Intracranial germinomas frequently involve the visual pathways and may thus present with visual failure in the young adult and paediatric population. They are rewarding tumours to identify, because, if properly diagnosed and managed, they can be eradicated or controlled.
References
Jennings MT, Gelman R, Hochberg F . Intracranial germ-cell tumours: natural history and pathogenesis. J Neurosurg 1985; 63: 155–167.
Horowitz MB, Hall WA . Central nervous system germinomas. Arch Neurol 1991; 48: 653–657.
Liang L, Korogi Y, Sagahara T . MRI of intracranial germ-cell tumours. Neuroradiology 2002; 44: 382–388.
Jakacki R . Central nervous system germ-cell tumours. Curr Treat Options Neurol 2002; 4: 139–145.
Hudgins RJ, Hudgins PA . Pineal region tumours in children. Contemp Neurosurg 1990; 12: 1–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hadjikoutis, S., Hughes, T. Germinoma with synchronous involvement of the pineal gland and the suprasellar region: a treatable cause of visual failure in a young adult. Eye 18, 525–526 (2004). https://doi.org/10.1038/sj.eye.6700715
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700715
Keywords
This article is cited by
-
Synchronous mixed germ cell tumor of the pineal gland and suprasellar region with a predominant angiomatous component: a diagnostic challenge
Journal of Neuro-Oncology (2009)
-
Germinoma with synchronous involvement of midline and off-midline structures associated with progressive hemiparesis and hemiatrophy in a young adult
Child's Nervous System (2007)
-
Germinoma with synchronous lesions in the pineal and suprasellar regions
Child's Nervous System (2006)