Abstract
Background:
Blood lipid levels as part of the metabolic syndrome are thought to be linked to cancer risk. Few epidemiological studies have addressed the association between serum triglyceride (STG) concentrations and cancer risk.
Methods:
Serum triglyceride concentrations were collected in a health investigation (1988–2003). The analyses included 156 153 subjects (71 693 men and 84 460 women), with 5079 incident cancers in men and 4738 cancers in women, and an average of 10.6 years of follow-up. All malignancies were ascertained from the population cancer registry. Multivariate Cox proportional hazard models stratified by age and sex were used to determine adjusted cancer risk estimates and 95% confidence interval (95% CI).
Results:
In men and women combined, higher STG concentrations were associated with increased risk of lung (4th vs 1st quartile: HR, 1.94; 95% CI, 1.47–2.54), rectal (HR, 1.56; 95% CI, 1.00–2.44), and thyroid cancer (HR, 1.96; 95% CI, 1.00–3.84). Serum triglyceride concentrations were inversely associated with non-Hodgkin's lymphoma. In men, STG concentrations were inversely associated with prostate cancer and positively with renal cancer. In women, STG concentrations were positively associated with gynaecological cancers. Stratification by BMI revealed a higher risk of gynaecological cancers in overweight than in normal weight women. No other associations were found.
Conclusions:
Our findings support the hypothesis that STG concentrations are involved in the pathogenesis of lung, rectal, thyroid, prostate, and gynaecological cancers.
Similar content being viewed by others
Main
Obesity has been identified as a major risk factor for such cancer sites as colon, renal, breast, and endometrium (Bianchini et al, 2002; Calle and Kaaks, 2004; Rapp et al, 2005), whereas hypertriglyceridemia is relevant to obesity and insulin resistance (Despres and Lemieux, 2006). Dietary fat intake is a well-established risk factor in cardiovascular diseases (CVDs), in which much investigation has involved serum triglyceride (STG) concentrations (Sarwar et al, 2007). The combination of hypertriglyceridemia and elevated waist circumference has been identified as a phenotype for higher risk of CVD (Kahn and Valdez, 2003). Usually, fasting triglyceride concentrations are measured, as they are associated with increased mortality and CVD risk (Brunzell, 2007). However, there is uncertainty with regard to the impact of STG concentrations on risk of CVD (Gotto, 1998 and also with regard to whether fasting level influences the relationship (Langsted et al, 2008). Beyond lipid metabolism there is evidence that hypertriglyceridemia is associated with frequent infections and inflammation (Khovidhunkit et al, 2004; Esteve et al, 2005).
A few cohort studies have investigated high STG concentrations as a part of the metabolic syndrome (Tulinius et al, 1997) in relation to risk of colon (Saydah et al, 2003; Ahmed et al, 2006, Tande et al, 2006), breast (Vatten and Foss, 1990; Furberg et al, 2004), and cervix cancers (Cust et al, 2007). A cohort study among Icelanders (Tulinius et al, 1997) revealed associations between high STG levels and colorectal cancers in both sexes, and also with thyroid cancer in men, as well as with cervix, endometrial, and bladder cancer in women (Tulinius et al, 1997).
We therefore investigated the associations between fasting STG concentrations and cancer risk in a large prospective cohort study.
Methods
Study population
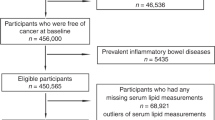
Details of the Vorarlberg Health Monitoring and Promotion Program (VHM&PP) in Vorarlberg, the most western region in Austria, are provided elsewhere (Rapp et al, 2005). In brief, the Agency of Social and Preventive Medicine annually offered to all adults living in Vorarlberg a screening examination that includes a physical examination, a blood test, and a consultation with a doctor. By 2005, ∼56% of all Vorarlberg residents underwent at least one examination in this voluntary screening programme. Between 1988 and 2003, over 156 000 adult Vorarlberg residents were enrolled in the cohort after signing an informed consent form to store and process personal data and biological samples.
For the current analysis, we used a data set with complete data on STG and covariates at baseline. Participants with follow-up <1 year (n=6188), or with prevalent cancer (other than non-melanoma skin cancer), were excluded before enrolment or within 1 year after enrolment (n=2149).
Two central laboratories, with regular internal and external quality tests, determined STG concentrations on fasting blood samples. Within 60–240 min of venous blood sample collection from a cubital vein, serum was obtained by centrifugation for 15 min at 4000 r.p.m. Subsequently, STG concentrations were measured at 37°C and were expressed as mg per 100 ml. To check calibration, three daily control samples were included. If average values of control samples of each run were not within 3% of the true value, the run was repeated. Day-by-day variation had to be within 5%. Study participants are classified according to the quartiles of STG concentrations with the following cutoff values: ⩽83, 84–119, 120–179, and ⩾180 mg 100 ml for men and ⩽69, 70–94, 95–133, and ⩾134 mg 100 ml for women. Participants in the 1st quartile were used as reference category.
Measurements of height, weight, blood pressure, total cholesterol, blood glucose, and gamma-glutamyltransferase (GGT) were obtained routinely for each participant. BMI was calculated by height and weight at baseline and was categorised on the basis of clinical guidelines (<25 kg m–2, 25 to <30 kg m−2, ⩾30.0 kg m−2) (World Health Organisation, 1998). Smoking status was classified as current, former, or non-smokers. Participants who never smoked could not be distinguished from those who did not respond to questions with regard to smoking at baseline, but baseline smoking status was verified for >70% of study participants on the basis of information provided at subsequent examinations. As a proxy for socioeconomic position, the occupational group (blue collar, white collar, or self-employed) was determined by the participant's insurance number. Retired participants were classified according to their former occupation, and housewives on the basis of the job of their spouse.
As described previously in detail (Rapp et al, 2005), cancer cases were identified by record linkage with the Vorarlberg cancer registry, which has been accepted for IARC publication since 1993 (Parkin DM et al, 2003) and has high completeness of ascertainment (Oberaigner W, 2006). In the Vorarlberg cancer registry, nearly all cancers (96.7%) were histologically verified and the Death-certificate-only (DCO) rate meets international quality criteria (5% for both sexes in 1998–2002). Cohort data were linked to the Vorarlberg Death Index to identify deaths and to calculate person-years. The current analysis makes use of the data set updated at the end of 2003. The average follow-up time was 10.6 (s.d. 4.5) years. The 10th Revision of the International Statistical Classification of Diseases, Injuries and Causes of Death (ICD) was used to code the cancers (World Health Organization, 2008).
Statistical analysis
The analytical cohort comprised 156 153 subjects (71 693 men and 84 460 women). Partial correlation coefficients were calculated to examine the relationship between STG and other clinical parameters. Cox proportional hazard models were used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for quartiles relative to the reference group (1st quartile of STG level). Models were adjusted for serum concentrations of glucose (mg per 100 ml, continuous)(Rapp et al, 2006), total cholesterol (mg per 100 ml, continuous) (Ulmer et al, 2004; Strasak et al, 2009), GGT (U l–1, continuous) (Strasak et al, 2008a,2008b), body mass index (BMI, kg m−2, continuous) (Rapp et al, 2005), occupational status, and smoking status (both in classes). Continuous risk estimates are presented for an increase in exposures of one unit log-transformed STG concentration. To test the overall significance of exposure, P-values for Wald χ2 statistics are shown. As no obvious sex differences between the estimates emerged, models were calculated for the sexes combined. All P-values are two-sided and all calculations were carried out with SAS statistical software package SAS release 9.1 (SAS Institute, Cary, NC, USA).
Results
During follow-up, 5079 incident invasive cancer cases among men and 4738 incident invasive cancer cases among women were identified (Table 1). Correlations between BMI, age, and serum concentrations of STG, total cholesterol, glucose, and GGT are shown in Table 2. STG was weakly associated with serum glucose concentrations and moderately associated with BMI, total cholesterol, and GGT concentrations.
Table 3 shows the hazard ratios for cancer type by STG concentrations in the VHM&PP cohorts. Compared with the 1st quartile, high STG concentrations (4th quartile) were associated with increased risk of lung (HR, 1.94; 95% CI, 1.47–2.54), rectal (HR, 1.56; 95% CI, 1.00–2.44), and thyroid cancer (HR, 1.96; 95% CI, 1.00–3.84). High STG concentrations were inversely associated with non-Hodgkin's lymphoma. Prostate cancer was inversely associated with STG concentrations (per log-unit HR, 0.80; 95% CI, 0.72–0.90) and was positively associated with incidence of kidney cancer in men (data not shown). High STG concentrations were associated with higher overall cancer risk (4th vs 1st quartile: HR, 1.19; 95% CI, 1.05–1.33) and with risk of gynaecological cancers (endometrium, ovar, cervix) (4th vs 1st quartile: HR, 1.62; 95% CI, 1.13–2.33).
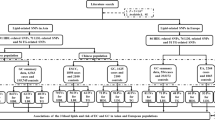
Figure 1 shows HRs for selected cancers by STG concentrations stratified by BMI. These did not reveal differential associations of STG levels with cancer overall, or with lung and colon cancer risk; however, the risk of gynaecological cancers was higher in overweight than in normal weight women. When data were stratified by smoking status (data not shown), no differential estimates emerged for overall and gynaecological cancers, but a somewhat higher risk of rectal cancer was found in current smokers (N=50 cases; per log-unit HR, 1.73; 95% CI, 1.02–2.92) than in non-smokers (N=177 cases; per log-unit HR, 1.11; 95% CI, 0.79–1.56), and a higher risk of lung cancer was found in non-smokers (N=222 cases; per log-unit HR, 1.57; 95% CI, 1.19–2.06) than in smokers (N=334 cases; per log-unit HR, 1.13; 95% CI, 0.91–1.39). However, no significant effect modification by BMI and smoking status was found. Stratification by GGT levels (⩽30 and >30 U l−1) revealed differential relationships between STG and overall cancer risk and lung cancer (data not shown).
Incidence of selected cancer sites according to sex-specific quartiles of serum triglyceride concentrations in the study population (N=156 153) by BMI*. *Adjusted for BMI (kg m−2, continuous), GGT (continuous), serum glucose (continuous), total cholesterol concentration (continuous), smoking status, occupational status, and sex (not for gynaecological cancers).
Discussion
In this large-scale cohort study, high STG concentrations were associated with higher overall cancer risk in women, but not in men. In men and women combined, STG concentrations were related to high risk of lung, thyroid, and rectal cancer. In men, STG concentrations were associated inversely with prostate cancer, and in women they were associated positively with gynaecological cancers. Our findings regarding lung, rectal, and gynaecological cancers are consistent with data using dietary fat intake levels as exposure variable (Kushi and Giovannucci, 2002; Genkinger et al, 2006).
Our observation of a positive association between STG levels and rectal cancer is in line with previous findings in a cohort study among Icelanders (Tulinius et al, 1997). Further evidence for a relationship with STG comes from case–control studies on colorectal adenoma (Kono et al, 1990; Bird et al, 1996; Otani et al, 2006; Tabuchi et al, 2006), carcinoma in situ (Yamada et al, 1998), and from an in-vitro study (Tabuchi et al, 2008). It has been suggested that total cholesterol, STG, and plasma glucose are positively associated with colorectal cancer risk (Yamada et al, 1998). In our study, the association occurred adjusted for plasma glucose and total cholesterol concentrations. In men and women combined, we observed an association between STG concentration and rectal cancer risk, whereas no association was found for colon cancer, neither was any association found in sex-stratified analyses. Consistent with a study among Japanese-American men (Tsushima et al, 2005) and US prospective studies (Saydah et al, 2003; Ahmed et al, 2006), we did not find a relationship with colorectal cancer.
Our findings of high lung cancer risk among subjects with high STG concentrations are unique. In one study, an association between total cholesterol and lung cancer risk has been observed, suggesting a relationship between lipid metabolism and lung cancer risk (Hinds et al, 1983). In the Carotene and Retinol Efficacy Trial (CARET), among the participants receiving β-carotene and retinol, higher serum triglyceride concentrations were observed (Cartmel et al, 2005), suggesting a relationship between STG and lung cancer risk. As smoking is associated with higher STG concentrations (Brunzell, 2007), residual confounding due to smoking may contribute to the association between STG concentrations and lung cancer risk. In our study, however, the association persisted when the data set was limited to non-smokers, suggesting that factors other than smoking status may contribute to the observed association. The limited differentiation between missing smoking data and non-smoking status may have resulted in misclassification of smoking status. However, smoking information from follow-up visits for most of the participants was used to complement the baseline smoking status.
The positive association with thyroid cancer risk is in line with findings in a cohort study (Tulinius et al, 1997). It may be relevant that BMI was positively associated with thyroid cancer (Renehan et al, 2008).
In our study, STG concentrations were inversely associated with prostate cancer risk, in contrast to the reverse findings in a case–control study (Wuermli et al, 2005). However, in this clinical-based study, prostate cancers were compared with benign prostate hyperplasia, in which STG levels were lower than those in cancer cases. In large cohort studies in Norway and the United States, no association between STG and prostate cancer risk was found (Lund et al, 2006; Tande et al, 2006). The application of prostate-specific antigen contributes to heterogeneity of phenotype (Etzioni et al, 2002), which may have distorted the relationship with STG. In addition, an inverse relationship for NHL was observed in our study. Previous reports on cholesterol indicted that reverse causation may substantially contribute to the risk-lowering effect of high blood lipids (Rose and Shipley, 1980; Lim et al, 2007; Strasak et al, 2009).
Our observation that STG concentrations were positively associated with kidney cancer incidence in men (data not shown) contrasts with a recently published meta-analysis on BMI and renal cancer risk (Renehan et al, 2008). However, in our study, after adjusting for diastolic blood pressure, an established risk factor for renal cancer (per log-unit HR, 1.26; 95% CI, 0.95–1.68), the association was no longer statistically significant. For men and women combined, we found no statistically significant association between STG and kidney cancer risk.
Our observation of a positive association of STG concentrations with risk of gynaecological cancers (cervix, ovary, endometrial) is consistent with other studies (Tulinius et al, 1997; Cust et al, 2007). In one study, increasing triglyceride and glucose concentrations were associated with increased endometrial cancer risk (Cust et al, 2007). Our findings on cervical cancer are in line with those in a cohort study (Tulinius et al, 1997). For breast cancer, inconsistent results have been reported from a nested case–control study (Agnoli et al, 2009) and from cohort studies (Vatten and Foss, 1990; Furberg et al, 2004).
These associations with gynaecological cancer raise a question with regard to the involvement of oestrogens, which are considered to stimulate hepatic triglyceride secretion (Sattler et al, 2005), as confirmed by studies on hormone replacement therapy (Rossouw et al, 2008; Sowers et al, 2008).
High STG concentrations may reflect other metabolic aspects that are procarcinogenic (McKeown-Eyssen, 1994). Associations between STG and plasma glucose levels are well established and hyperglycaemia is a risk factor for several cancers (Ashley and Kannel, 1974). In our study, however, we used fasting STG levels and adjusted for plasma glucose levels to control for confounding by glucose levels. Inflammation is another potential mechanism by which hypertriglyceridemia is associated with cancer risk (Esteve et al, 2005; Kundu and Surh, 2008). STG concentrations may be linked to colorectal cancer risk by bile acid excretion, circulation hormones, or energy supply to neoplastic cells (McKeown-Eyssen, 1994).
A limitation of our study is the lack of information on such potential risk factors as alcohol consumption and physical activity. However, the results of our multivariate models adjusted for GGT concentrations may be considered as a proxy variable for alcohol intake (Whitehead et al, 1978). In addition, no information on medication history (for example, on lipid-lowering drugs or hormones) was available, which may have affected the associations observed. Among women, the effect of STG may be overestimated because of residual confounding by exogenous hormones, whereas for lipid-lowering medications, the opposite could be relevant.
Undocumented measurement variation in STG concentrations during the study period may also have affected our results, but we assume that these were minor, as we used fasting STG levels. The strengths of our study are large sample size, prospective design, length of follow-up, and standardised examinations by trained physicians. It is relevant that the study population is relatively young and healthy.
Overall, STG concentrations were positively associated with the risk of lung, thyroid, and rectal cancers, but inversely with NHL risk. Prostate cancer risk was inversely associated with STG concentrations, whereas positive associations were found with renal cancer among men and with gynaecological cancers among women. Our results suggest that STG concentrations are involved in the pathogenesis of several cancer sites.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Agnoli C, Berrino F, Abagnato CA, Muti P, Panico S, Crosignani P, Krogh V (2009) Metabolic syndrome and postmenopausal breast cancer in the ORDET cohort: a nested case-control study. Nutr Metab Cardiovasc Dis (E-pub ahead of print 8 April 2009)
Ahmed RL, Schmitz KH, Anderson KE, Rosamond WD, Folsom AR (2006) The metabolic syndrome and risk of incident colorectal cancer. Cancer 107: 28–36
Ashley Jr FW, Kannel WB (1974) Relation of weight change to changes in atherogenic traits: the Framingham Study. J Chronic Dis 27: 103–114
Bianchini F, Kaaks R, Vainio H (2002) Overweight, obesity, and cancer risk. Lancet Oncol 3: 565–574
Bird CL, Ingles SA, Frankl HD, Lee ER, Longnecker MP, Haile RW (1996) Serum lipids and adenomas of the left colon and rectum. Cancer Epidemiol Biomarkers Prev 5: 607–612
Brunzell JD (2007) Clinical practice. Hypertriglyceridemia. N Engl J Med 357: 1009–1017
Calle EE, Kaaks R (2004) Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4: 579–591
Cartmel B, Dziura J, Cullen MR, Vegso S, Omenn GS, Goodman GE, Redlich CA (2005) Changes in cholesterol and triglyceride concentrations in the Vanguard population of the Carotene and Retinol Efficacy Trial (CARET). Eur J Clin Nutr 59: 1173–1180
Cust AE, Kaaks R, Friedenreich C, Bonnet F, Laville M, Tjonneland A, Olsen A, Overvad K, Jakobsen MU, Chajes V, Clavel-Chapelon F, Boutron-Ruault MC, Linseisen J, Lukanova A, Boeing H, Pischon T, Trichopoulou A, Christina B, Trichopoulos D, Palli D, Berrino F, Panico S, Tumino R, Sacerdote C, Gram IT, Lund E, Quiros JR, Travier N, Martinez-Garcia C, Larranaga N, Chirlaque MD, Ardanaz E, Berglund G, Lundin E, Bueno-de-Mesquita HB, van Duijnhoven FJ, Peeters PH, Bingham S, Khaw KT, Allen N, Key T, Ferrari P, Rinaldi S, Slimani N, Riboli E (2007) Metabolic syndrome, plasma lipid, lipoprotein and glucose levels, and endometrial cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Endocr Relat Cancer 14: 755–767
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444: 881–887
Esteve E, Ricart W, Fernandez-Real JM (2005) Dyslipidemia and inflammation: an evolutionary conserved mechanism. Clin Nutr 24: 16–31
Etzioni R, Penson DF, Legler JM, di Tommaso D, Boer R, Gann PH, Feuer EJ (2002) Overdiagnosis due to prostate-specific antigen screening: lessons from US prostate cancer incidence trends. J Natl Cancer Inst 94: 981–990
Furberg AS, Veierod MB, Wilsgaard T, Bernstein L, Thune I (2004) Serum high-density lipoprotein cholesterol, metabolic profile, and breast cancer risk. J Natl Cancer Inst 96: 1152–1160
Genkinger JM, Hunter DJ, Spiegelman D, Anderson KE, Beeson WL, Buring JE, Colditz GA, Fraser GE, Freudenheim JL, Goldbohm RA, Hankinson SE, Koenig KL, Larsson SC, Leitzmann M, McCullough ML, Miller AB, Rodriguez C, Rohan TE, Ross JA, Schatzkin A, Schouten LJ, Smit E, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Zhang SM, Smith-Warner SA (2006) A pooled analysis of 12 cohort studies of dietary fat, cholesterol and egg intake and ovarian cancer. Cancer Causes Control 17: 273–285
Gotto Jr AM (1998) Triglyceride: the forgotten risk factor. Circulation 97: 1027–1028
Hinds MW, Kolonel LN, Lee J, Hankin JH (1983) Dietary cholesterol and lung cancer risk among men in Hawaii. Am J Clin Nutr 37: 192–193
Kahn HS, Valdez R (2003) Metabolic risks identified by the combination of enlarged waist and elevated triacylglycerol concentration. Am J Clin Nutr 78: 928–934
Khovidhunkit W, Kim MS, Memon RA, Shigenaga JK, Moser AH, Feingold KR, Grunfeld C (2004) Effects of infection and inflammation on lipid and lipoprotein metabolism: mechanisms and consequences to the host. J Lipid Res 45: 1169–1196
Kono S, Ikeda N, Yanai F, Yamamoto M, Shigematsu T (1990) Serum lipids and colorectal adenoma among male self-defence officials in northern Kyushu, Japan. Int J Epidemiol 19: 274–278
Kundu JK, Surh YJ (2008) Inflammation: gearing the journey to cancer. Mutat Res 659: 15–30
Kushi L, Giovannucci E (2002) Dietary fat and cancer. Am J Med 113 (Suppl 9B): 63S–70S
Langsted A, Freiberg JJ, Nordestgaard BG (2008) Fasting and nonfasting lipid levels. Influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation 118 (20): 2047–2056
Lim U, Gayles T, Katki HA, Stolzenberg-Solomon R, Weinstein SJ, Pietinen P, Taylor PR, Virtamo J, Albanes D (2007) Serum high-density lipoprotein cholesterol and risk of non-Hodgkin's lymphoma. Cancer Res 67: 5569–5574
Lund HL, Wisloff TF, Holme I, Nafstad P (2006) Metabolic syndrome predicts prostate cancer in a cohort of middle-aged Norwegian men followed for 27 years. Am J Epidemiol 164: 769–774
McKeown-Eyssen G (1994) Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol Biomarkers Prev 3: 687–695
Oberaigner W, Vittadello F (2006) Cancer mapping in Alpine Regions 1996–2000. Pro literature Verlag: Mammendarf
Otani T, Iwasaki M, Ikeda S, Kozu T, Saito H, Mutoh M, Wakabayashi K, Tsugane S (2006) Serum triglycerides and colorectal adenoma in a case-control study among cancer screening examinees (Japan). Cancer Causes Control 17: 1245–1252
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB, all at the International Agency for Research on Cancer (2003) Cancer Incidence in Five Continents. IARC: Lyon, France
Rapp K, Schroeder J, Klenk J, Stoehr S, Ulmer H, Concin H, Diem G, Oberaigner W, Weiland SK (2005) Obesity and incidence of cancer: a large cohort study of over 145 000 adults in Austria. Br J Cancer 93: 1062–1067
Rapp K, Schroeder J, Klenk J, Ulmer H, Concin H, Diem G, Oberaigner W, Weiland SK (2006) Fasting blood glucose and cancer risk in a cohort of more than 140 000 adults in Austria. Diabetologia 49: 945–952
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371: 569–578
Rose G, Shipley MJ (1980) Plasma lipids and mortality: a source of error. Lancet 1: 523–526
Rossouw JE, Cushman M, Greenland P, Lloyd-Jones DM, Bray P, Kooperberg C, Pettinger M, Robinson J, Hendrix S, Hsia J (2008) Inflammatory, lipid, thrombotic, and genetic markers of coronary heart disease risk in the women's health initiative trials of hormone therapy. Arch Intern Med 168: 2245–2253
Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, Boekholdt SM, Khaw KT, Gudnason V (2007) Triglycerides and the risk of coronary heart disease: 10 158 incident cases among 262 525 participants in 29 Western prospective studies. Circulation 115: 450–458
Sattler AM, Soufi M, Maisch B, Schaefer JR (2005) Lipids and lipoproteins in women. Herz 30: 368–374
Saydah SH, Platz EA, Rifai N, Pollak MN, Brancati FL, Helzlsouer KJ (2003) Association of markers of insulin and glucose control with subsequent colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 12: 412–418
Sowers MR, Randolph Jr J, Jannausch M, Lasley B, Jackson E, McConnell D (2008) Levels of sex steroid and cardiovascular disease measures in premenopausal and hormone-treated women at midlife: implications for the ‘timing hypothesis’. Arch Intern Med 168: 2146–2153
Strasak AM, Pfeiffer RM, Brant LJ, Rapp K, Hilbe W, Oberaigner W, Lang S, Borena W, Concin H, Diem G, Ruttmann E, Glodny B, Pfeiffer KP, Ulmer H (2009) Time-dependent association of total serum cholesterol and cancer incidence in a cohort of 172 210 men and women: a prospective 19-year follow-up study. Ann Oncol 20 (6): 1113–1120
Strasak AM, Pfeiffer RM, Klenk J, Hilbe W, Oberaigner W, Gregory M, Concin H, Diem G, Pfeiffer KP, Ruttmann E, Ulmer H (2008a) Prospective study of the association of gamma-glutamyltransferase with cancer incidence in women. Int J Cancer 123: 1902–1906
Strasak AM, Rapp K, Brant LJ, Hilbe W, Gregory M, Oberaigner W, Ruttmann E, Concin H, Diem G, Pfeiffer KP, Ulmer H (2008b) Association of gamma-glutamyltransferase and risk of cancer incidence in men: a prospective study. Cancer Res 68: 3970–3977
Tabuchi M, Kitayama J, Nagawa H (2006) Hypertriglyceridemia is positively correlated with the development of colorectal tubular adenoma in Japanese men. World J Gastroenterol 12: 1261–1264
Tabuchi M, Kitayama J, Nagawa H (2008) Hyperglycemia and hypertriglyceridemia may associate with the adenoma-carcinoma transition in colorectal epithelial cells. J Gastroenterol Hepatol 23: 985–987
Tande AJ, Platz EA, Folsom AR (2006) The metabolic syndrome is associated with reduced risk of prostate cancer. Am J Epidemiol 164: 1094–1102
Tsushima M, Nomura AM, Lee J, Stemmermann GN (2005) Prospective study of the association of serum triglyceride and glucose with colorectal cancer. Dig Dis Sci 50: 499–505
Tulinius H, Sigfusson N, Sigvaldason H, Bjarnadottir K, Tryggvadottir L (1997) Risk factors for malignant diseases: a cohort study on a population of 22 946 Icelanders. Cancer Epidemiol Biomarkers Prev 6: 863–873
Ulmer H, Kelleher C, Diem G, Concin H (2004) Why Eve is not Adam: prospective follow-up in 149 650 women and men of cholesterol and other risk factors related to cardiovascular and all-cause mortality. J Womens Health (Larchmt) 13: 41–53
Vatten LJ, Foss OP (1990) Total serum cholesterol and triglycerides and risk of breast cancer: a prospective study of 24 329 Norwegian women. Cancer Res 50: 2341–2346
Whitehead TP, Clarke CA, Whitfield AG (1978) Biochemical and haematological markers of alcohol intake. Lancet 1: 978–981
World Health Organisation (1998) Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation on Obesity. WHO: Geneva
World Health Organization (2008) International Classification of Diseases (ICD). WHO: Geneva. Available at http://www.who.int/classifications/icd/en
Wuermli L, Joerger M, Henz S, Schmid HP, Riesen WF, Thomas G, Krek W, Cerny T, Gillessen S (2005) Hypertriglyceridemia as a possible risk factor for prostate cancer. Prostate Cancer Prostatic Dis 8: 316–320
Yamada K, Araki S, Tamura M, Sakai I, Takahashi Y, Kashihara H, Kono S (1998) Relation of serum total cholesterol, serum triglycerides and fasting plasma glucose to colorectal carcinoma in situ. Int J Epidemiol 27: 794–798
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ulmer, H., Borena, W., Rapp, K. et al. Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br J Cancer 101, 1202–1206 (2009). https://doi.org/10.1038/sj.bjc.6605264
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605264
Keywords
This article is cited by
-
Establishment and validation of serum lipid-based nomogram for predicting the risk of prostate cancer
BMC Urology (2023)
-
Association of serum lipids and abnormal lipid score with cancer risk: a population-based prospective study
Journal of Endocrinological Investigation (2023)
-
Metabolic syndrome and thyroid Cancer: risk, prognosis, and mechanism
Discover Oncology (2023)
-
Association between the TyG index and TG/HDL-C ratio as insulin resistance markers and the risk of colorectal cancer
BMC Cancer (2022)
-
High-density lipoprotein, low-density lipoprotein and triglyceride levels and upper gastrointestinal cancers risk: a trans-ancestry Mendelian randomization study
European Journal of Clinical Nutrition (2022)