Abstract
Administration of BAS 100, a novel mechanism-based CYP3A4 inhibitor isolated from grapefruit juice, resulted in a 2.1-fold increase in erlotinib exposure following oral administration to wild-type and humanised CYP3A4 transgenic mice. This study illustrates the potential of BAS 100 to increase the low and variable oral bioavailability of erlotinib in cancer patients.
Similar content being viewed by others
Main
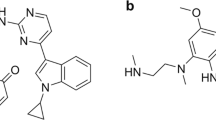
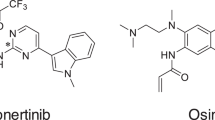
Erlotinib (also known as Tarceva or OSI-774) is a quinazolinamine, small molecule inhibitor of epidermal growth factor receptor (EGFR) tyrosine kinase. It is approved for the treatment of advanced nonsmall cell lung cancer as a single agent and advanced pancreatic cancer in combination with gemcitabine. Erlotinib has an average oral bioavailability in humans of 59% (Frohna et al, 2006), but exhibits substantial (up to eight-fold) interindividual pharmacokinetic variability (Hidalgo et al, 2001; Tan et al, 2004), which may result in variable treatment outcomes. Erlotinib is extensively metabolised into multiple products (Ling et al, 2006), including an active O-desmethyl metabolite, OSI-420. Cytochrome P450 3A4 (CYP3A4) plays a prominent role in the metabolism of this agent (Li et al, 2007b). As erlotinib is subject to extensive first-pass metabolism following oral administration, inhibition of intestinal and/or hepatic CYP3A4 activity may be a promising strategy to decrease interindividual pharmacokinetic variability. The objective of this study was to evaluate the effect of CYP3A4 inhibition by BAS 100, a novel spiro-ortho-ester mechanism-based inhibitor of CYP3A4 present in grapefruit juice (Li et al, 2006a, 2007a), on the pharmacokinetics of erlotinib in mice. Since the grapefruit effect was first reported in the early 1990s (Bailey et al, 1991), the ingestion of grapefruit juice has been shown to enhance the systemic exposure of a number of orally administered drugs (Bailey et al, 2004).
Materials and methods
BAS 100 was obtained from Bioavailabilty Systems (Cocoa Beach, FL, USA), and erlotinib and OSI-420 were obtained from Toronto Research Chemicals (North York, ON, Canada). All other chemicals and reagents were purchased from Sigma-Aldrich (St Louis, MO, USA). Female BALB/c mice (6–8 weeks old) were kept in a controlled environment, with food and water available ad libitum. All procedures were carried out with NCI Animal Care and Use Committee approval. In the first study, BAS 100 and erlotinib were formulated in 10% DMSO and 5% polysorbate 80 in saline. Mice were randomised to receive erlotinib (10 mg kg−1, p.o.) alone or 30 min after BAS 100 (10 mg kg−1, p.o.). Blood was collected by cardiac puncture from three mice per time point at 0.083, 0.25, 0.5, 1, 2, 4, 6 and 24 h following erlotinib administration, and centrifuged to obtain plasma. In the second study, erlotinib was formulated in 0.3% carboxymethylcellulose and 0.1% polysorbate 80 in saline. Female CYP3A4 transgenic mice (Granvil et al, 2003) and wild-type FVB/NCr mice (14 weeks old) received erlotinib (10 mg kg−1, p.o.) alone or 30 min after BAS 100 (25 mg kg−1, p.o.). Blood was collected 2 h after erlotinib administration. All samples were stored at −80°C until analysis. Plasma concentrations of erlotinib and OSI-420 were measured as described previously (Zhao et al, 2003). Plasma concentrations of BAS 100 were measured by a novel liquid chromatography-tandem mass spectrometry method. Briefly, plasma samples were prepared by protein precipitation with acetonitrile. BAS 100 and the internal standard (temazepam) were resolved isocratically on a Waters XTerra MS C18 column (50 × 2.1 mm internal diameter; 3.5 μm particle size). The mass spectrometer was equipped with an electrospray ionisation source and operated in positive mode. Detection was performed by multiple reaction monitoring. The lower limit of quantitation was 10 ng ml−1. Pharmacokinetic parameters were determined by noncompartmental analysis using WinNonlin Professional Version 5.2 (Pharsight Corporation, Mountain View, CA, USA). Bailer's method (Bailer, 1988) was used to estimate the variance of the area under the curve (AUC). A Z-test was used for the pairwise comparison of AUCs (Yuan, 1993).
Results
Administration of BAS 100 prior to erlotinib resulted in a 2.1-fold increase in the AUC of erlotinib (37 953 vs 17 957 h ng ml−1, P<0.05, Figure 1). The AUC of the metabolite, OSI-420, was increased to a similar extent by BAS 100 (Table 1). The relative extent of metabolism of erlotinib into OSI-420 (0.21 and 0.17, respectively), and the half-life of OSI-420 (2.4 and 2.5 h, respectively) were similar whether erlotinib was administered alone or following BAS 100 (Table 1). Interestingly, a 2.5-fold increase in the dose of BAS 100 (to 25 mg kg−1) did not result in a further increase in erlotinib exposure (data not shown). The 2-h plasma concentration of erlotinib was increased by BAS 100 to a similar extent in CYP3A4 transgenic (2.0-fold; 1857±300 vs 929±80 ng ml−1) and wild-type mice (1.9-fold; 1409±237 vs 744±135 ng ml−1). BAS 100 itself was orally bioavailable, reaching peak concentrations at 1 h following administration (Figure 2). These concentrations are in the range required for the inhibition of human CYP3A4 in vitro (Li et al, 2006a).
Discussion
The present study indicates that BAS 100 significantly increased the systemic exposure of erlotinib following oral administration, although it did not change the relative extent of metabolism of erlotinib into OSI-420. Furthermore, the half-lives of the parent drug and the metabolite were not affected by BAS 100. This suggests that the modulation of erlotinib pharmacokinetics by BAS 100 takes place at the level of intestinal absorption rather than elimination. The fact that BAS 100 increased circulating concentrations of erlotinib to a similar extent in mice expressing human CYP3A4 in the intestine and wild-type mice further substantiates this supposition. However, it is also possible that, as a result of Cyp3a inhibition by BAS 100, biotransformation of erlotinib into OSI-420 is shunted to another metabolic pathway that is unaffected by BAS 100. In addition, it cannot be excluded that BAS 100 affects the formation of one or more of the other known erlotinib metabolites (Ling et al, 2006) that were not measured in this study, or that BAS 100 inhibits ABC transporter-mediated efflux of erlotinib in the intestine (Li et al, 2006a). Of note, the relative extent of metabolism of erlotinib into OSI-420 observed in this study is similar to that reported in cancer patients (0.12; Hidalgo et al, 2001). The bioavailability of erlotinib in mice has not been published. However, assuming it is similar to that observed in humans (59%; Frohna et al, 2006), one would not expect a modulator of its metabolism and/or transport to increase its exposure more than two-fold. Indeed, a 2.5-fold increase in the dose of BAS 100 (to 25 mg kg−1) did not result in a further increase in erlotinib exposure in the current study. In patients treated with erlotinib, the pharmacodynamic end point of rash, which has been associated with improved survival (Wacker et al, 2007), is significantly correlated to erlotinib exposure (Lu et al, 2006; Strother et al, 2006). Furthermore, previously obtained data on the related drug, gefitinib, indicate that patients with high CYP3A4 activity are likely to benefit from a modified regimen (increased dose), to achieve the drug concentrations required to interact with EGFR (Li et al, 2006b). A strategy by which enzyme activity is intentionally inhibited could achieve similar results. In view of the significant inverse correlation between decreasing absolute bioavailability and interindividual pharmacokinetic variability (Hellriegel et al, 1996), the current data provide a rationale for the development of exploratory clinical studies aimed at decreasing the variability in erlotinib exposure by concomitant administration of BAS 100.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bailer AJ (1988) Testing for the equality of area under the curves when using destructive measurement techniques. J Pharmacokinet Biopharm 16: 303–309
Bailey DG, Malcolm J, Arnold O, Spence JD (2004) Grapefruit juice–drug interactions. 1998. Br J Clin Pharmacol 58: S831–S840; discussion S841–S843
Bailey DG, Spence JD, Munoz C, Arnold JM (1991) Interaction of citrus juices with felodipine and nifedipine. Lancet 337: 268–269
Frohna P, Lu J, Eppler S, Hamilton M, Wolf J, Rakhit A, Ling J, Kenkare-Mitra SR, Lum BL (2006) Evaluation of the absolute oral bioavailability and bioequivalence of erlotinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in a randomized, crossover study in healthy subjects. J Clin Pharmacol 46: 282–290
Granvil CP, Yu AM, Elizondo G, Akiyama TE, Cheung C, Feigenbaum L, Krausz KW, Gonzalez FJ (2003) Expression of the human CYP3A4 gene in the small intestine of transgenic mice: in vitro metabolism and pharmacokinetics of midazolam. Drug Metab Dispos 31: 548–558
Hellriegel ET, Bjornsson TD, Hauck WW (1996) Interpatient variability in bioavailability is related to the extent of absorption: implications for bioavailability and bioequivalence studies. Clin Pharmacol Ther 60: 601–607
Hidalgo M, Siu LL, Nemunaitis J, Rizzo J, Hammond LA, Takimoto C, Eckhardt SG, Tolcher A, Britten CD, Denis L, Ferrante K, von Hoff DD, Silberman S, Rowinsky EK (2001) Phase I and pharmacologic study of OSI-774, an epidermal growth factor receptor tyrosine kinase inhibitor, in patients with advanced solid malignancies. J Clin Oncol 19: 3267–3279
Li F, Desai PB, Harris JW (2006a) Modulation of hepatic and intestinal CYP3A4 and P-gp expression and activity by BAS 100, a naturally occurring bioavailability-boosting agent from grapefruit juice. Drug Metab Rev 38 (Suppl 2): 116
Li F, Kulkarni A, Pauletti G, Desai P (2007a) Influence of BAS 100, a spiro-ortho-ester, isolated from grapefruit juice on the activity and expression of drug metabolizing enzymes and transporters. AAPS J 9 (Suppl 2): Abstract T3402
Li J, Karlsson MO, Brahmer J, Spitz A, Zhao M, Hidalgo M, Baker SD (2006b) CYP3A phenotyping approach to predict systemic exposure to EGFR tyrosine kinase inhibitors. J Natl Cancer Inst 98: 1714–1723
Li J, Zhao M, He P, Hidalgo M, Baker SD (2007b) Differential metabolism of gefitinib and erlotinib by human cytochrome P450 enzymes. Clin Cancer Res 13: 3731–3737
Ling J, Johnson KA, Miao Z, Rakhit A, Pantze MP, Hamilton M, Lum BL, Prakash C (2006) Metabolism and excretion of erlotinib, a small molecule inhibitor of epidermal growth factor receptor tyrosine kinase, in healthy male volunteers. Drug Metab Dispos 34: 420–426
Lu JF, Eppler SM, Wolf J, Hamilton M, Rakhit A, Bruno R, Lum BL (2006) Clinical pharmacokinetics of erlotinib in patients with solid tumors and exposure–safety relationship in patients with non-small cell lung cancer. Clin Pharmacol Ther 80: 136–145
Strother RM, Jones DR, Skaar T, Huh WS, Porter J, Foster A, Sweeney C (2006) Erlotinib-associated rash correlates with plasma levels at steady state. J Clin Oncol ASCO Annual Meeting Proceedings Part I. 24 (18S): 13008
Tan AR, Yang X, Hewitt SM, Berman A, Lepper ER, Sparreboom A, Parr AL, Figg WD, Chow C, Steinberg SM, Bacharach SL, Whatley M, Carrasquillo JA, Brahim JS, Ettenberg SA, Lipkowitz S, Swain SM (2004) Evaluation of biologic end points and pharmacokinetics in patients with metastatic breast cancer after treatment with erlotinib, an epidermal growth factor receptor tyrosine kinase inhibitor. J Clin Oncol 22: 3080–3090
Wacker B, Nagrani T, Weinberg J, Witt K, Clark G, Cagnoni PJ (2007) Correlation between development of rash and efficacy in patients treated with the epidermal growth factor receptor tyrosine kinase inhibitor erlotinib in two large phase III studies. Clin Cancer Res 13: 3913–3921
Yuan J (1993) Estimation of variance for AUC in animal studies. J Pharm Sci 82: 761–763
Zhao M, He P, Rudek MA, Hidalgo M, Baker SD (2003) Specific method for determination of OSI-774 and its metabolite OSI-420 in human plasma by using liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 793: 413–420
Acknowledgements
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research (Bethesda, MD, USA). We thank Dr Linda G Byrd (Laboratory of Metabolism, Centre for Cancer Research, National Cancer Institute, Bethesda, MD, USA) for assistance with the CYP3A4 transgenic mouse study and Dr Ming Zhao (Johns Hopkins University, Baltimore, MD, USA) for assistance with sample analyses.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products or organisations implies endorsement by the US Government.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Smith, N., Baker, S., Gonzalez, F. et al. Modulation of erlotinib pharmacokinetics in mice by a novel cytochrome P450 3A4 inhibitor, BAS 100. Br J Cancer 98, 1630–1632 (2008). https://doi.org/10.1038/sj.bjc.6604353
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604353
Keywords
This article is cited by
-
The matricellular protein CCN1 suppresses hepatocarcinogenesis by inhibiting compensatory proliferation
Oncogene (2016)
-
Preclinical assessment of the interactions between the antiretroviral drugs, ritonavir and efavirenz, and the tyrosine kinase inhibitor erlotinib
Cancer Chemotherapy and Pharmacology (2015)
-
Preclinical Pharmacokinetic/Pharmacodynamic Models to Predict Schedule-Dependent Interaction Between Erlotinib and Gemcitabine
Pharmaceutical Research (2013)
-
Tumor penetration and epidermal growth factor receptor saturation by panitumumab correlate with antitumor activity in a preclinical model of human cancer
Molecular Cancer (2012)