Abstract
Capillary malformation (CM; ‘port-wine stain’), is a common vascular malformation affecting cutaneous capillary vessels in 0.3% of newborns. Increased incidence of lesions in first-degree relatives of these patients and several reported familial cases suggest that genetic factors may play a role in the pathogenesis of CM. We report the first genome-wide linkage analysis of familial CM. In the non-parametric linkage analysis, strong evidence of linkage (peak Z-score 6.72, P-value 0.000136) was obtained in an interval of 69 cM between markers D5S407 and D5S2098, corresponding to 5q11–5q23. Parametric linkage analysis gave a maximum combined HLOD score of 4.84 (α-value 0.67) at marker D5S2044 on 5q15, and analysis using only the linked families, defined a smaller, statistically significant locus CMC1 of 23 cM (peak LOD score 7.22) between markers D5S1962 and D5S652 corresponding to 5q13–5q15. Interesting candidate genes implicated in vascular and neural development, such as MEF2C, RASA1, and THBS4, are in this locus.
Similar content being viewed by others
Introduction
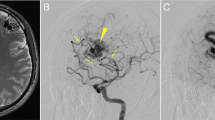
Vascular anomalies are a heterogenous group of disorders manifesting abnormal development of blood vessels. They are divided into tumours and malformations, and the latter are sub-categorised according to the defective type of vessel.1 Capillary malformation (CM, ‘port-wine stain’), (OMIM 163000) is a common vascular malformation, occurring in 0.3% of neonates.2 CMs are flat cutaneous lesions (Figure 1) that are typically located in the head and neck region, and change in colour from pink-to-purple with age.3 These lesions are usually obvious at birth and grow proportionally with the child. Similar macular stains of the face and neck, called ‘salmon patch’, ‘angel's kiss’, or ‘nevus flammeus neonatorum’ occur in up to 40% of newborns,2,4 however, they predictably fade during infancy. In contrast, CMs do not disappear; they darken, and often thicken with age, and cause psychological distress.5
Clinical and histological characteristics of capillary malformation (CM). (A and B) CM on face, subject I-2 (family M) and subject III-11 (family C), respectively. Subject III-11 (family C) had also an intramaxillar arteriovenous malformation. (C) CM on hand, subject III-1 (family A). (D) CM on thorax, subject III-4 (family C). (E), retroauricular CM, subject III-1 (family F). (F) hematoxylin eosin staining of CM. Asterisks (*) indicate dilated capillary-like channels within papillary dermis.
Although CM is usually sporadic, families in which these lesions segregate in a dominant manner, with incomplete penetrance, have been reported.6,7,8,9 Further evidence of genetic predisposition has been obtained in demographic studies showing that 7–22% of CM patients have relatives with a cutaneous vascular stain.8,10,11 Thus, susceptibility to CM can be familial, but low penetrance and high frequency of sporadic cases complicate determination of an inheritance pattern.
CM also occurs in the combined vascular syndromes. A patch of CM is frequently found in the skin overlying a pure (classic) lymphatic malformation.3 In Klippel–Trenaunay syndrome (OMIM 149000), capillary malformation is associated with vascular anomalies of lymphatics and veins, and accompanied by hypertrophy of bone and soft tissues.3 Interestingly, the prevalence of CM in the first-degree relatives of patients with Klippel–Trenaunay syndrome is 1.8%, significantly higher than in the general population.12 This suggests that descendants of patients with CM have an increased risk for Klippel–Trenaunay syndrome. Parkes–Weber syndrome is another combined vascular disorder composed of CM, multiple arteriovenous fistulas, and tissue hypertrophy.3 Sturge–Weber syndrome (OMIM 185300) is defined as a cutaneous CM located in V1, or V1–V2 trigeminal neurotomal distribution associated with choroidal and leptomeningeal anomalies and causing facial hypertrophy, glaucoma, and epilepsy.13
Etiopathogenesis of CM is poorly understood. Histologically, these lesions have an increased number of ectatic capillary-like channels within the papillary dermis, suggesting defective angiogenesis (Figure 1F).14 Walls of the dilated vessels have normal morphology, based on immunohistochemical analysis of major structural components, such as type IV collagen and fibronectin.15 Similarly, endothelial-specific antigens such as factor VIII, PAL-E (pathologische anatomie Leiden-endothelium), ICAM-1 (intercellular adhesion molecule-1) and ELAM-1 (endothelial leukocyte adhesion molecule-1) exhibit normal staining patterns in the ectatic capillaries.16 In contrast, studies using antibodies against neuronal cytoplasmic protein (PGP 9.5), neuron-specific enolase (NSE), and S100 protein have demonstrated that the density of cutaneous nerves is significantly decreased in CM.17,18 These findings support the hypothesis that the gradual dilatation of the dermal vessels is the result of abnormal neural regulation of blood flow.17 However, the decreased density of cutaneous nerves can be a secondary effect due to reduced blood flow and chronic ischemia in the lesions.19
In an effort to understand the genetic mechanisms that underlie CM, and are likely to control cutaneous vascular morphogenesis, we performed genome-wide linkage analysis on six families with inherited CM (families A–F, Figure 2). Using non-parametric and parametric linkage analysis, we identified cosegregation of CM with a large locus on chromosome 5q. This region of susceptibility was reinforced by analysis of seven additional families with inherited CM, and a minimal locus of 23 cM could be identified with a subset of the families.
Materials and methods
Informed consent was obtained from all subjects participating in the study, in accordance with the ethics committees of the Faculty of Medecine of Université catholique de Louvain, Saitama Children's Medical Center and Boston Children's Hospital. Blood or buccal brush samples were collected from 60 affected and 51 unaffected individuals (Figure 2). Patients were clinically examined by a plastic surgeon (LM Boon, JB Mulliken and S Watanabe), or general practitioner (H Grynberg). In the 13 families involved in this study, most CMs were pink-to-purple macular lesions, measuring a few centimeters in diameter (Figure 1). All subjects with a CM of at least 1 cm in diameter were considered affected. Individuals with only one lesion, smaller than 1 cm, or with faint nuchal stain, reminiscent of a fading birthmark, were considered to be unaffected. Out of 60 affected subjects, 19 had a lesion on the face, 15 in the nuchal region and 26 in other parts of the body. Fifteen subjects had multiple lesions (Figure 2). In subject III-12, in family C, and subject III-1 in family E, an arteriovenous malformation underlay the cutaneous vascular stain (Figure 2). Subject III-5, in family D, had an arteriovenous fistula between the left carotid artery and jugular vein, a cutaneous vascular stain and soft tissue hypertrophy of the homolateral face. Subject III-11, in family C, had a hemi-facial CM associated with left intramaxillar arteriovenous malformation (Figure 1B).
Genomic DNA was extracted from blood samples using the Qiagen DNA purification kit (Westburg, the Netherlands) or from buccal cells using a lysis method, as described.20 The six most informative families (A–F) were selected for a genome scan. Due to space constraints on acrylamide gels, some unaffected individuals were left out and the screening was performed on 34 affected and 26 unaffected subjects (Figure 2). Since none of the six families showed evidence of sex-linked inheritance, the genome scan was restricted to the autosomes. Fluorescently labelled polymorphic markers from Human MapPairs genomewide screening set (n=356, 10 cM average resolution) were amplified by PCR using the conditions recommended by the supplier (LI-COR, Westburg, the Netherlands). Amplified markers were electrophoresed on 6.5% acrylamide gels on Gene Readir 4200 DNA analyser, and genotyped with SAGA GT 2.0 software (LI-COR, Westburg, the Netherlands). Altogether, 168 additional markers, synthesized by Gibco Lifetechnologies (UK) or Isogen (the Netherlands), were used to cover genomic regions where Human MapPairs markers were uninformative. These markers were radioactively end-labelled with γ-[32P] using polynucleotide kinase (TAKARA/BioWhittaker, Belgium) before amplification by PCR, and electrophoresed on 5% acrylamide gels, and scored manually after autoradiography overnight. Multipoint linkage analyses were performed with Genehunter 2.0.21 The unaffected grandparents in family D (I-1 and I-2) and unaffected subject II-2 in family F were considered unknown for CM phenotype in all linkage calculations (Figure 2).
Results
CM segregated as a dominant trait in the 13 studied families. Evidence for incomplete penetrance was noted in families D, F, L and M (Figure 2). In addition, phenotypic variation from single small CM in extremities to large facial lesion with arteriovenous involvement, was observed (Figures 1 and 2).
A non-parametric multipoint linkage analysis was performed first. This identified strong evidence of linkage between CMs and chromosome 5q. A maximum Z-score of 4.50 with a P-value of 0.0025 was found between markers D5S401 and D5S2044, and a 28 cM region with a P-value<0.01 was observed between markers D5S357 and D5S652. Suggestive evidence of linkage (P-value<0.05) was also found on chromosomes 2p (P=0.031), 4q (P=0.049), 6q (P=0.015), 7q (P=0.045), 8p (P=0.045), 10q (P=0.045) and 12p (P=0.028).
Genomewide multipoint linkage analysis was then performed under the assumption of autosomal dominant mode of inheritance with an allelic frequency of 0.0001 for the disease. The analysis was carried out with 90 and 80% penetrances, and the phenocopy rate was set at 0.3%, corresponding to the incidence of CM in the general population. With 90% penetrance, a statistically significant multipoint HLOD of 4.58 (α-value 0.92) was obtained on 5q between markers D5S357 and D5S2003, confirming the results of non-parametric analysis. There was also suggestive evidence of linkage (HLOD>1.0) on 6q, with a multipoint HLOD score of 1.06 (α-value 0.25). No other chromosomes exhibited evidence of linkage. 5q and 6q also gave the highest multipoint HLOD scores under 80% penetrance: 4.41 and 0.98, respectively.
In order to further define the linked region on chromosome 5q, 27 additional markers were genotyped for the six families, including the family members, mostly unaffected, who were excluded in the initial screening (Figure 2). Furthermore, seven additional small CM families (Figure 2) were genotyped with eight markers on chromosome 5q. Non-parametric linkage analysis using these 13 families yielded a maximum Z-score of 6.72 (P-value=0.000136) at marker AFM205WG7 on 5q15 (Figure 3). The Z-score remained significant (P<0.01) over a 69 cM region between D5S407 and D5S2098, with the exemption of an interval of 1 cM (proximal to marker D5S2084) (P=0.011).
Multipoint linkage analysis of chromosome 5q on 13 families. Thick line, multipoint Z-score; thin line, multipoint HLOD score with 90% penetrance and 0.3% phenocopy rate. Maximum multipoint Z-score of 6.72 obtained at marker AFM205WG7, and maximum multipoint HLOD score of 4.84 1 cM centromeric of AFM205WG7. Genetic distance, in cM, from 5pter shown below.
Parametric multipoint linkage analyses of chromosome 5q, under various penetrances (50–90%) with all the 13 families, gave the highest multipoint HLOD scores with 90% penetrance. A maximum HLOD of 4.84 (α-value 0.67) was obtained at marker D5S2044, which is 1 cM centromeric of marker AFM205WG7 that yielded the peak in the NPL analysis (Figure 3). Another peak of HLOD>3.0 was 4.09 (α-value 0.51), between markers D5S2084 and D5S1453. In the studied 5q region, the estimated fraction of families linked (α-values) varied between 0.51 and 0.67, suggesting genetic heterogeneity. When the families B, E, G and M, which yielded negative multipoint LOD scores at marker D5S2044, were excluded from linkage analysis, a maximum multipoint LOD score of 7.22 (α-value 1.00) was obtained at marker D5S2044 using 90% penetrance (Figure 4). The most likely linked region, defined by borders of multipoint LOD score<−2.00, was between markers D5S1962 and D5S652, covering 23 cM (Figure 4).
Multipoint linkage analysis on nine families (A, C, D, F, H, I, J, K and L) linked to CMC1-locus. Analysis performed under 90% penetrance and 0.3% phenocopy rate. Maximum LOD score of 7.22 obtained at marker D5S2044 (1 cM centromeric of marker AFM205WG7). Most likely linked region located between markers D5S1962 and D5S652. Genetic distance, in cM, from 5pter shown below.
Discussion
The results of the non-parametric and parametric linkage analyses showed that the CMC1-locus for susceptibility for capillary malformations is located on 5q. However, the high rate of phenocopies (0.3%), the incomplete penetrance, and the obvious genetic heterogeneity complicate determination of the exact boundaries for the locus. In the non-parametric linkage analysis, strong evidence of linkage (peak Z-score 6.72, P-value 0.000136) was obtained in an interval of 69 cM between markers D5S407 and D5S2098, corresponding to 5q11–5q23. Parametric linkage analysis, using only the linked families, defined a smaller, statistically significant locus of 23 cM (LOD score 7.22) between markers D5S1962 and D5S652 corresponding to 5q13–5q15.
Genes expressed in embryonal angiogenesis should be prime positional candidates for mutations that cause CM. However, it is difficult to pinpoint the best positional candidate genes, as studies on other vascular malformations have shown that the defective proteins have very different functions.22,23 For example, mutations in cell surface receptors are known, such as TIE2 (endothelial cell-specific tyrosine kinase) in familial mucocutaneous venous malformation;24 VEGFR3 (vascular endothelial growth factor receptor-3) in inheritable lymphedema;25,26 and endoglin and activin in hereditary haemorrhagic telangiectasia.27,28 Transcription factor FOXC2 (forkhead family transcription factor) is responsible for multiple lymphedema syndromes,29 and mutations in a gene coding for intracellular putative signalling molecule, KRIT1 (Krev1 interaction trapped-1), cause cerebral capillary malformations, sometimes associated with hyperkeratotic cutaneous capillary–venous malformation.30,31,32 Moreover, positional cloning has led to identification of a factor with unknown function as the cause for glomuvenous malformation (‘glomangioma’).33
The 23 cM CMC1-locus reported here contains a number of potential genes, such as MEF2C (myocyte enhancer factor-2C) and RASA1 (RAS p21 protein activator-1). Mice deficient in MEF2C manifested lumen size abnormalities of the large vessels close to the heart, as well as diminished peripheral capillary vasculature.34 This was suggested to be due to defects in remodelling of the primary vascular network to mature vasculature. In the RASA1 null mice, the primary capillary plexus of the yolk sac failed to mature and remained in a honeycomb structure at E10.5.35 Mosaic mice composed of wild-type and RASA1 null cells survived longer, and at E15, embryos exhibited localized vascular defects resembling CM. The large 69 cM region contains also FER (FPS/FES related tyrosine kinase) gene, an activating mutation of which resulted in hypervascularity and multifocal vascular anomalies in transgenic mice.36 In addition, molecules connected to neurogenesis should be considered. THBS4 (thrombospondin-4) gene, involved in neuronal growth and sprouting,37 is located in the 23 cM interval. Furthermore, SIAT8D (Sialyl-transferase-8) and EFNA5 (ephrin-A5) genes, which have been implicated in the development of the central nervous system, are located in the larger linked region.38,,39
Interestingly, there is some evidence for chromosome 5q being involved in the genesis of other vascular anomalies, specifically familial hemangiomas and Klippel–Trenaunay syndrome. Hemangiomas, which are histologically characterized by overgrowth of capillaries, are benign vascular tumours occurring in up to 10% of infants. Recent studies on clonality have suggested that hemangiomas arise from an intrinsic defect, ie a somatic mutation, in vascular endothelial cells.40 Interestingly, six hemangioma tissues showed evidence of LOH in chromosome 5q in a large region overlapping with the CMC1-locus.41 There is also suggestive linkage for familial hemangiomas to 5q31-33, an interval distal to CMC1.42 In addition, a patient with a balanced translocation between chromosomes 5q13.3 and 11p15.1 was found in Klippel–Trenaunay syndrome.43 Thus, it is possible that inherited CMs, familial hemangiomas and Klippel–Trenaunay syndrome, three conditions with capillary involvement, share some common pathogenic mechanisms.
In summary, we identified a susceptibility locus, CMC1, for familial capillary malformation on chromosome 5q. Identification of the causative gene(s) should give insight into ethiopathogenic mechanisms that cause inherited and sporadic CM, and CM in combination with other vascular defects. It should also shed light into embryonal capillary morphogenesis and thus to angiogenesis in general.
References
Mulliken JB, Glowacki J . Hemangiomas and vascular malformation in infants and children: A classification based on endothelial characteristics Plast Reconstr Surg 1982 69: 412–420
Jacobs AH, Walton RG . The incidence of birthmarks in the neonate Pediatrics 1976 58: 218–222
Mulliken JB, Young AE (eds). Vascular birthmarks: Hemangiomas and malformations Philadelphia: WB Saunders 1988
Pratt AG . Birthmarks in infants AMA Arch Derm Syph 1967 67: 302
Lanigan SW, Cotterill JA . Psychological disabilities amongst patients with port wine stains Br J Dermatol 1989 121: 209–215
Pasyk KA . Familial multiple lateral telangiectatic nevi (port-wine stain) Clin Genet 1992 41: 197–201
Redondo P, Vazquez-Doval F . Familial multiple nevi flammei J Am Acad Dermatol 1996 35: 769–770
van der Horst CMAM, van Eijk TGJ, de Borgie CAJM, Koster PHL, Struycken PM, Strackee SD . Hereditary port-wine stains, do they exist? Lasers Med Sci 1999 14: 238–243
Berg JN, Quaba AA, Georgantopoulou A, Porteous ME . A family with hereditary port wine stain J Med Genet 2000 37: 12
Mills CM, Lanigan SW, Hughes J, Anstey AV . Demographic study of port wine stain patients attending a laser clinic: family history, prevalence of naevus anaemicus and results of prior treatment Clin Exp Dermatol 1997 22: 166–168
Troilius A . Characterisation and treatment of patients with port wine stains with special reference to the emotional impact PhD thesis, Lund University, Lund, Sweden 1999
Aelvoet GE, Jorens PG, Roelen LM . Genetic aspects of the Klippel-Trenaunay syndrome Br J Dermatol 1992 126: 603–607
Enjolras O, Riché MC, Merland JJ . Facial port-wine stains and Sturge-Weber syndrome Pediatrics 1985 76: 48–51
Barsky SH, Rosen S, Geer DE, Noe JM . The nature and evolution of port wine stains: A computer-assisted study J Invest Dermatol 1980 74: 154–157
Finley JL, Clark RA, Colvin RB, Blackman R, Noe J, Rosen S . Immunofluorescent staining with antibodies to factor VIII, fibronectin, and collagenous basement membrane protein in normal human skin and port wine stains Arch Dermatol 1982 118: 971–975
Neumann R, Leonhartsberger H, Knobler R, Honigsmann H . Immunohistochemistry of port-wine stains and normal skin with endothelium-specific antibodies PAL-E, anti-ICAM-1, anti-ELAM-1, and anti-factor VIIIrAg Arch Dermatol 1994 130: 879–883
Smoller BR, Rosen S . Port-wine stains. A disease of altered neural modulation of blood vessels? Arch Dermatol 1986 122: 177–179
Rydh M, Malm M, Jernbeck J, Dalsgaard CJ . Ectatic blood vessels in port-wine stains lack innervation: Possible role in pathogenesis Plast Reconstr Surg 1991 87: 419–422
Oosthuyse B, Moons L, Storkebaum E et al. Deletion of the hypoxia-response element in the vascular endothelial growth factor promoter causes motor neuron degeneration Nat Genet 2001 28: 131–138
Richards B, Skoletsky J, Shuber AP et al. Multiplex PCR amplification from the CFTR gene using DNA prepared from buccal brushes/swabs Hum Mol Genet 1993 2: 159–163
Kruglyak L, Daly MJ, Reeve-Daly MP, Lander ES . Parametric and nonparametric linkage analysis: a unified multipoint approach Am J Hum Genet 1996 58: 1347–1363
Vikkula M, Boon LM, Mulliken JB, Olsen BR . Molecular basis of vascular anomalies Trends Cardiovasc Med 1998 8: 281–292
Vikkula M, Boon LM, Mulliken JB . Molecular genetics of vascular malformation Matrix Biol 2001 20: 327–335
Vikkula M, Boon LM, Carraway KL et al. Vascular dysmorphogenesis caused by an activating mutation in the receptor tyrosine kinase TIE2 Cell 1996 87: 1181–1190
Kärkkäinen MJ, Ferrell RE, Lawrence EC et al. Missense mutations interfere with VEGFR-3 signalling in primary lymphoedema Nat Genet 2000 25: 153–159
Irrthum A, Karkkainen MJ, Devriendt K, Alitalo K, Vikkula M . Congenital hereditary lymphedema caused by a mutation that inactivates VEGFR3 tyrosine kinase Am J Hum Genet 2000 67: 295–301
Johnson DW, Berg JN, Baldwin MA et al. Mutations in the activin receptor-like kinase 1 gene in hereditary haemorrhagic telangiectasia type 2 Nat Genet 1996 13: 189–195
McAllister KA, Grogg KM, Johnson DW et al. Endoglin, a TGF-beta binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1 Nat Genet 1994 8: 345–351
Finegold DN, Kimak MA, Lawrence EC et al. Truncating mutations in FOXC2 cause multiple lymphedema syndromes Hum Mol Genet 2001 10: 1185–1189
Laberge-le Couteulx S, Jung HH, Labauge P et al. Truncating mutations in CCM1, encoding KRIT1, cause hereditary cavernous angiomas Nat Genet 1999 23: 189–193
Sahoo T, Johnson EW, Thomas JW et al. Mutations in the gene encoding KRIT1, a Krev-1/rap1a binding protein, cause cerebral cavernous malformations (CCM1) Hum Mol Genet 1999 8: 2325–2333
Eerola I, Plate KH, Spiegel R, Boon L, Mulliken JB, Vikkula M . KRIT1 is mutated in hyperkeratotic cutaneous capillary-venous malformation associated with cerebral capillary malformation Hum Mol Genet 2000 9: 1351–1355
Brouillard P, Boon LM, Mulliken JB et al. Mutations in a novel factor glomulin are responsible for glomuvenous malformations (‘glomangiomas’) Am J Hum Genet 2002 70: 866–874
Bi W, Drake CJ, Schwarz JJ . The transcription factor MEF2C-null mouse exhibits complex vascular malformations and reduced cardiac expression of angiopoietin 1 and VEGF Dev Biol 1999 15: 255–267
Henkemeyer M, Rossi DJ, Holmyard DP et al. Vascular system defects and neuronal apoptosis in mice lacking ras GTPase-activating protein Nature 1995 377: 695–701
Greer P, Haigh J, Mbamalu G, Khoo W, Bernstein A, Pawson T . The Fps/Fes protein-tyrosine kinase promotes angiogenesis in transgenic mice Mol Cell Biol 1994 14: 6755–6763
Arber S, Caroni P . Thrombospondin-4, an extracellular matrix protein expressed in the developing and adult nervous system promotes neurite outgrowth J Cell Biol 1995 131: 1083–1094
Nakayama J, Fukuda MN, Fredette B, Ranscht B, Fukuda M . Expression cloning of a human polysialyltransferase that forms the polysialylated neural cell adhesion molecule present in embryonic brain Proc Natl Acad Sci USA 1995 92: 7031–7035
Drescher U, Kremoser C, Handwerker C, Loschinger J, Noda M, Bonhoeffer F . In vitro guidance of retinal ganglion cell axons by RAGS, a 25 kDa tectal protein related to ligands for Eph receptor tyrosine kinases Cell 1995 82: 359–370
Boye E, Yu Y, Paranya G, Mulliken JB, Olsen BR, Bischoff J . Clonality and altered behavior of endothelial cells from hemangiomas J Clin Invest 2001 107: 745–752
Berg JN, Walter JW, Thisanagayam U et al. Evidence for loss of heterozygosity of 5q in sporadic haemangiomas: Are somatic mutations involved in haemangioma formation? J Clin Pathol 2001 54: 249–252
Walter JW, Blei F, Anderson JL, Orlow SJ, Speer MC, Marchuk DA . Genetic mapping of a novel familial form of infantile hemangioma Am J Med Genet 1999 82: 77–83
Whelan AJ, Watson MS, Porter FD, Steiner RD . Klippel-Trenaunay-Weber syndrome associated with a 5:11 balanced translocation Am J Med Genet 1995 59: 492–494
Acknowledgements
The authors are grateful to all the families involved in this study. The work was supported by the Fonds Speciaux de Recherche – Université catholique de Louvain, the Belgian Federal Service for Scientific, Technical and Cultural Affairs, and the F.N.R.S (Fonds national de la recherche scientifique) (all to M Vikkula, a ‘chercheur qualifié du F.N.R.S’). I Eerola was supported by a Marie Curie Fellowship of the European Community Program Quality of Life, under contract number QLRI-CT-1999-51491. The authors thank Ms Ana Gutierrez for technical assistance and Mrs Liliana Niculescu for secretarial help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eerola, I., Boon, L., Watanabe, S. et al. Locus for susceptibility for familial capillary malformation (‘port-wine stain’) maps to 5q. Eur J Hum Genet 10, 375–380 (2002). https://doi.org/10.1038/sj.ejhg.5200817
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5200817
Keywords
This article is cited by
-
Theoretical and in vivo experimental investigation of laser hyperthermia for vascular dermatology mediated by liposome@Au core–shell nanoparticles
Lasers in Medical Science (2022)
-
A novel RASA1 mutation causing capillary malformation-arteriovenous malformation (CM-AVM): the first genetic clinical report in East Asia
Hereditas (2018)
-
Genome-wide analyses identify common variants associated with macular telangiectasia type 2
Nature Genetics (2017)
-
A spectrum of intracranial vascular high-flow arteriovenous shunts in RASA1 mutations
Child's Nervous System (2016)
-
Fluch des Diplomaten
Rechtsmedizin (2014)