Key Points
-
Presents the case of a pregnant woman with erosions and desquamation with erythematose areas only on the gingiva due to Pemphigus vulgaris.
-
Gingival lesions comprise severe desquamative or erosive gingivitis.
-
Often the disease initially manifests on the gingiva so dentists should be the first to recognise it.
-
An early diagnosis reduces the need to use a high dose of corticoids.
Abstract
The erosive gingival lesions associated with vesiculobullous diseases can be an important early clinical manifestation of serious diseases such as pemphigus vulgaris (PV). PV is a vesiculobullous disease of the skin and mucosa which tends to be chronic and which normally affects people of 40-60 years of age.1,2,34,5 Its incidence varies from 0.5 to 3.2 cases per 100,000 per year.6,7 Mucosal lesions are located mainly in the oral and pharyngeal mucosa, although conjunctiva, larynx, nasal mucosa, vulva, vagina, cervix, and ano-rectal mucosa may also be involved. It is a serious mucocutaneous disease of an autoimmune nature, whose appearance during pregnancy is extremely rare.8,9,10
Similar content being viewed by others
Main
It initially manifests itself in the oral cavity in 50% of cases11,12,13 in the form of irregular erosions or ulcers, lesions that are secondary to the breaking of the blisters due to the thinness and friability of their covering.14,15 Mucosal lesions may be the sole sign for an average of five months before skin lesions develop, or they may be the sole manifestation of the disease. Early diagnosis improves the prognosis and prevents the lesions from spreading.16,17,1819,20 When the disease has its initial manifestation on the gingiva dentists are often the first to recognise it. Gingival lesions comprise severe desquamative or erosive gingivitis where bullae have ruptured to leave flaps of healing tissue with red erosions or deep ulcerative craters, mainly in the attached gingiva. We describe a PV case of exclusively gingival location that began during pregnancy.
Case report
The patient, a 32-year-old Caucasian living in the north-west of the province of Murcia (SE Spain) came to the consultation because of a generalised pain she had been suffering in her gums for eight weeks. She had previously been treated for pregnancy gingivitis by means of oral hygiene and antiseptics (chlorhexidine), but there had been no improvement in her condition. Medical records showed that the patient had had hepatitis B at the age of ten. She had no drug habit and did not smoke. She was in the twentieth week of pregnancy and had delivered a normal healthy son six years ago after an uneventful pregnancy.
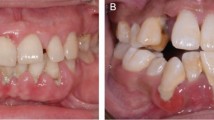
Intra-oral examination showed erosions and desquamation with erythematose areas on the gingiva which were not healing. The discomfort felt by the patient was limited to difficulties in eating. The Nikolsky sign was negative. Examination showed an amalgam restoration in tooth 24, the absence of tooth 36 and no prosthesis (Figs 1 and 2). Extra-orally, there were no signs of skin lesions or lesions to the mucosa. A blood test showed slight hyperglycaemia 120mg/dL (80-110mg/dL), other parameters being normal. A gingival biopsy was made using an 8 mm punch and the histopathological examination showed intense acantholysis in the lower stratum spinosum, with the basal cells of the epithelium remaining attached to the basement membrane, suggesting a diagnosis of pemphigus vulgaris (Fig. 3). Direct immunofluorescence on fresh tissue was positive and revealed the presence of IgG in the intercellular spaces throughout the epithelium, a pattern immunofluorescence consistent with diagnosis of PV.
A further inspection was made to discount any other lesion to the skin or mucosa. It was decided to prescribe anaesthetic mouthwashes and corticosteroids (0.05% clobetasol propionate) (Colgate-Palmolive España SA, Madrid, Spain) applied topically three times a day in association with nystatin 100,000IU/cc. The oral symptoms improved with this treatment, permitting the patient to eat and thus avoid any ill effects associated with malnutrition of the foetus. Three months after the first oral examination, the patient was no longer suffering symptoms and could eat and drink normally. The patient's condition was followed by the dermatology and neonatology services throughout the pregnancy since antibodies can pass the placental barrier, producing neonatal pemphigus. No alteration was observed (prematurity or foetal death).
Discussion
This study concerns a pregnant woman with erosions and desquamation with erythematose areas only on the gingiva due to PV. The oral manifestation of PV tends to be early, as in our case, affecting the mouth only on the gingiva, with no cutaneous lesions or other mucous membrames.3,7 Clinically, PV manifests itself as blisters, which break easily during eating. Any pressure or trauma may increase the size of the blisters, which is why exploration usually shows secondary ulcers or erosions covered by a pseudo-membrane. Nikolsky's sign is sometimes positive but never as strongly as in the skin.1,2
In cases of PV, the form of the erosive gingival lesions differential diagnosis must be made with other entities, especially lichen planus and cicatricial pemphigoid, as well as lupus erythematosus, epidermolysis bullosa acquisita and linear IgA disease. Similar appearances may be seen in reaction to dental materials, mouthwashes, medications and chewing-gum.11 In our experience, early gingival lesions due to PV only rarely appear as extensive erythema and erosions. It can be diagnosed clinically, by exfoliative cytology, histopathology and direct and indirect immunofluorescence.4,18
Histologically, epithelial acantholysis with little inflammatory reaction can be seen. The acantholytic cells are found in the vesicles, in the roof of which villi, corresponding to papillae with remaining basal stratum showing signs of incipient regeneration are very prominent. By exfoliative cytology it is possible to see the Tzanck cells — due to the acantholysis. Direct immunofluorescence is the gold standard for diagnosis5,11 which shows a reticular pattern at the level of the stratum spinosum due to the deposit of immunoglobins (IgG) and complement C3. Indirect immunofluorescence is 80-90% positive, pointing to the presence of antibodies circulating in the serum. The antibody titre is correlated with the activity of the disease.
Pemphigus in pregnancy is rare. When present, maternal autoantibodies may cross the placenta, resulting in neonatal pemphigus. Neonatal pemphigus is transient and improves with clearance of maternal autoantibodies. PV during pregnancy creates the problem of the need to treat the disease and the similar need not to alter the physiology of the pregnancy.
Treatment is based on systemic corticoids. PV is the most serious cause; prior to the introduction of systemic corticosteroid treatment, the clinical course of PV was unfavourable. Therapy must be tailored for each patient, taking into account pre-existing and coexisting conditions.6 There is no consensus regarding the initial steroid dosage needed to induce remission nor its effect on the subsequent course of the disease, but it is generally agreed that low doses (60 mg/d) usually do not suffice to induce initial control.17 In pregnant patients, there is a slight risk of teratogenesis (cleft palate) and delayed intra-uterine growth when administered in high doses early in pregnancy. It is recommended to begin treatment with systemic corticoids after the twelfth week of gestation to avoid the risk of teratogenesis. The use of azathioprine, cyclophosphamide and methotrexate to treat PV should be avoided because they provoke immunosuppression and teratogenesis. In our case, the lesions were exclusively located in the mouth on gingiva and we instructed the patient in what oral hygiene measures she should take and anaesthetic solutions that should be used before eating so that she could eat adequately. Corticoids were also applied topically and in this way the lesions could be controlled.
Early diagnosis is the most important arm in fighting the disease since this means that treatment can be begun during its early stages, thus reducing the need to use corticoids. The number of cases of PV during pregnancy is small and the recurrence of symptoms cannot be predicted, meaning that each case should be treated individually.
References
Chossegros C . Advanced oral lesions. Pemphigus vulgaris. Rev Stomatol Chir Maxillofac 2003; 104: 302–303.
Barnett M L . Pemphigus vulgaris presenting as a gingival lesion. A case report. J Periodontol 1988; 59: 611–614.
Castellano Suarez J L . Gingival disorders of immune origin. Med Oral 2002; 7: 271–283.
Fantasia J E, Damm D D . Oral diagnosis. Mucosal and skin lesions. Pemphigus vulgaris. Gen Dent 2002; 50: 82–84.
Scully C, Challacombe S J . Pemphigus vulgaris: update on etiopathogenesis, oral manifestations, and management. Crit Rev Oral Biol Med 2002; 13: 397–404.
Muhammad J K, Lewis M A, Crean S J . Oral pemphigus vulgaris occurring during pregnancy. J Oral Pathol Med 2002; 31: 121–124.
Stoopler E T, DeRossi S S, Sollecito T P . Pemphigus: update for the general practitioner. N Y State Dent J 2003; 69: 30–32.
Chowdhury M M, Natarajan S . Neonatal pemphigus vulgaris associated with mild oral pemphigus vulgaris in the mother during pregnancy. Br J Dermatol 1998; 139: 500–503.
Daniel Y, Shenhav M, Botcham A, Peyser M R, Lessin JB . Pregnancy associated with pemphigus. Br J Obstet Gynaecol 1995; 102: 67–69.
Virgili A, Corazza M, Vesce F, Garutti P, Mollica G, Califano A . Pemphigus in pregnancy. Acta Derm Venereal 1995; 75: 172–190.
Stoopler E T, Sollecito T P, DeRossi S S . Desquamative gingivitis: early presenting symptom of mucocutaneous disease. Quint Int 2003; 34: 582–586.
Campo-Voegeli A, Muniz F, Mascaro J M, Garcia F, Casals M, Arimany J L et al. Neonatal pemphigus vulgaris with extensive mucocutaneous lesions from a mother with oral pemphigus vulgaris. Br J Dermatol 2002; 147: 801–805.
Scully C, Paes De AlmeidaO, Porter S R, Gilkes J J . Pemphigus vulgaris: the manifestations and long-term management of 55 patients with oral lesions. Br J Dermatol 1999; 40: 84–86.
Pires F R, Ferraz C C, Alves Fde A, Lopes M A, Paes De Almeida O . Pemphigus vulgaris in adolescence: case report. Pediatr Dent 2000; 22: 159–162.
Davenport S, Chen S Y, Miller A S . Pemphigus vulgaris: clinicopathogenic review of 33 cases in the oral cavity. Int J Perio Rest Dent 2001; 21: 85–90.
Navarro C M, Sposto M R, Onofre M A, Scully C . Gingival lesions diagnosed as pemphigus vulgaris in an adolescent. Case report. J Periodontol 1999; 70: 808–812.
Mignogna M D, Lo MuzioL, Bucci E . Clinical features of gingival pemphigus vulgaris. J Clin Periodontol 2001; 28: 489–493.
Fainaru O, Mashiach R, Kupferminc M, Shenhav M, Pauzner D, Lessing J B . Pemphigus vulgaris in pregnancy: a case report and review of literature. Hum Reprod 2000; 15: 11–15.
Robinson J C, Lozada-Nur F, Frieden I . Oral pemphigus vulgaris: a review of the literature and a report on the management of 12 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 84: 349–355.
Kalayciyan A, Engin B, Serdaroglu S, Mat C, Aydemir E H, Kotogyan A . A retrospective analysis of patients with pemphigus vulgaris associated with pregnancy. Br J Dermatol 2002; 147: 396–397.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
López-Jornet, P., Bermejo-Fenoll, A. Gingival lesions as a first symptom of pemphigus vulgaris in pregnancy. Br Dent J 199, 91–92 (2005). https://doi.org/10.1038/sj.bdj.4812523
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812523