Key Points
-
The main aim of this work was to determine if Enhance-L.C. adhesion promoter is material-specific as stated by the manufacturer.
-
Enhance-L.C. neither significantly increases the bond strength of Light-Bond (the manufacturer's recommended adhesive) nor Transbond-XT.
-
Light-Bond/ Enhance-L.C. provided a bond strength significantly greater than Transbond-XT/Enhance-L.C.
-
Light-Bond left less remaining adhesive on the enamel than Transbond-XT, whether or not either of the systems were used with Enhance-L.C.
Abstract
Objective Enhance-L.C. is an orthodontic adhesion promoter. Our aim was to find out if this product is material-specific as stated by its manufacturers or whether its effects are similar when the promoter is used with other adhesive systems.
Design In vitro study.
Setting Dental Clinic. University of Murcia, Spain, 2002.
Materials and methods Enhance-L.C. was used with one of the manufacturer's recommended adhesives, Light-Bond, and with a second from another manufacturer, Transbond-XT. One hundred premolars were divided into four groups of 25 premolars: 1)Transbond-XT, 2) Transbond-XT/Enhance-L.C., 3) Light-Bond, 4) Light-Bond/Enhance-L.C.
Main outcome measures Shear bond strength was evaluated with a universal test machine and the adhesive remaining after debonding was determined using image analysis equipment.
Results Enhance-L.C. did not significantly increase the bond strength of either of the two systems (P > 0.008). However, Light-Bond/Enhance-L.C. provided a bond strength significantly greater (P < 0.008) than Transbond-XT and Transbond-XT/Enhance-L.C. Light-Bond also left significantly (P < 0.05) less adhesive remaining on the enamel than Transbond-XT, whether or not either of the systems were used with Enhance-L.C.
Conclusions The use of Enhance-L.C with Light-Bond is to be recommended whenever extra bond strength is needed.
Similar content being viewed by others
Main
Bracket bond failure is one of the most frustrating ocurrences in orthodontic practice. The consequences include an increase in treatment time, additional costs in both materials and personnel, and additional patient visits.
The three most important factors affecting bond strength between a bracket and the enamel surface are: the retention mechanisms at the base of the bracket, the adhesive material, and the preparation of the tooth surface.1
The percentage of bracket failure is currently estimated to be between 5 and 7% of brackets bonded using light-cured or self-cured composite resins.2,3
Enhance-L.C. (Reliance, Itasca, Ill.) is an adhesion promoter used in orthodontics. The expression 'adhesion promoter' was first used in connection with certain molecules which could achieve chemical bonding in dental structures.4 One of the first molecules to be used was NPG-GMA [N-(2hydroxy-3-methacryloxy-propyl)-N-phenylglycine], introduced by Bowen in 1965.5
Enhance-L.C. is composed of HEMA (Hydroxyethyl methacrylate), tetrahydrofurfuryl cyclohexane dimethacrylate and ethanol. The HEMA molecule contains two functional groups, one hydrophobic, the other hydrophilic.6 Hydrophilic priming resins have been used mainly on dentine in conservative dentistry, but it would appear that the incorporation of hydrophilic monomers in adhesive systems helps resin infiltrate enamel etched at the level of the prisms. This characteristic should reduce interfacial porosity and therefore increase adhesion, achieving a greater bond strength through polymerization.7 On the basis of these concepts, such resins are being introduced into various orthodontic adhesives in order to improve bond strength and interfacial integrity.8
According to the manufacturer, Enhance-L.C. can increase bond strength amongst its own range of bonding products (Phase II, Rely-a-Bond, Light-Bond or Excel) with any enamel (including fluorosed, hypocalcified or temporary), metal or composite surfaces.
The main aim of this work was to determine if Enhance-L.C. is material-specific as stated by the manufacturer, or if it produces the same effects with other adhesives systems which do not belong to this manufacturer's range of products. To do this, it was used in combination with one of the recommended systems, Light-Bond, and another light-cured composite resin adhesive from another manufacturer as standard reference, Transbond-XT (3M Unitek Dental Products, Monrovia, Calif.).
Materials and Methods
Teeth
A hundred human upper premolars, free from caries and fillings were used. These had been extracted for reasons unrelated to the objectives of this study and with the informed consent of the patients. The project has been approved by the Murcia University Bio-ethical Commission.
The teeth were washed in water to remove any traces of blood and then placed in a 0.1% Timol solution. Afterwards they were stored in distilled water which was changed periodically to avoid deterioration. In no case was a tooth stored for more than a month after extraction.
The premolars were set in a 4 cm long copper cylinder with an internal diameter of 3 cm, their roots set in type IV plaster.
Brackets
One hundred metal upper premolar brackets were used (Victory Series, 3M Unitek Dental Products, Monrovia, Calif.).
The base area of each bracket was calculated (mean = 9.79 mm2) using image analysis equipment and MIP 4 software (Microm Image Processing Software. Digital Image Systems, Barcelona, Spain).
Bonding procedure
The teeth were divided into four groups of 25 upper premolars and brackets were bonded on the buccal surface.
For all groups the buccal surfaces were polished with a rubber cup and polishing paste (Détartrine, Septodont. Saint-Maur, France), afterwards the area to which the bracket was to be located was etched with a 37% o-phosphoric acid gel (Total Etch, Ivoclar, Vivadent, Schaan, Liechtenstein) for thirty seconds, and then washed with water. After washing, for groups I and III the enamel surface was completely dried with compressed air; for groups II and IV, the enamel surface was air-dried leaving the surface slightly moist.
Group I: Transbond-XT (3M Unitek Dental Products, Monrovia, Calif.). A layer of Transbond-XT primer was applied and was light-cured for ten seconds with an Ortholux XT lamp (3M Unitek Dental Products, Monrovia, Calif.). Transbond-XT paste was applied to the base of the bracket which was then placed onto the tooth pressing firmly. Excess adhesive was removed from around the base of the bracket, the adhesive was light-cured positioning the light guide on each interproximal side for ten seconds. We followed the instructions supplied by the manufacturer of this product.
Group II: Transbond-XT/Enhance-L.C. Two layers of Enhance-L.C. (Reliance, Itasca, Ill) were applied; after the second layer the surface was completely dried with compressed air. The surface should be left with a shiny appearance. Immediately afterwards the bracket was bonded in place with Transbond-XT adhesive system (primer and paste). We followed the instructions supplied by the manufacturer of each product.
Group III: Light-Bond (Reliance, Itasca, Ill.). A layer of Light-Bond liquid resin was applied and light-cured for ten seconds. Light-Bond paste was applied to the base of the bracket which was positioned on the tooth pressing firmly. Excess adhesive was removed from around the base of the bracket and it was light-cured positioning the light guide on the incisal side of the bracket for twenty seconds and for ten seconds on the mesial side. We followed the instructions supplied by the manufacturer of this product.
Group IV: Light-Bond/Enhance-L.C. After applying Enhance-L.C. as in Group II, the brackets were bonded in position with Light-Bond (primer and paste). We followed the instructions supplied by the manufacturer of each product.
Storage of test specimens
The specimens were immersed in distilled water at a temperature of 37°C for 24 hours.9
Bond strength test
Shear bond strength was measured with a universal test machine (Autograph AGS-1KND, Shimadzu. Japan) with a 1 KN load cell connected to a metal rod with one end angled at 30°. The cross-head speed was 1mm min−1.9
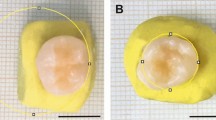
The teeth were set at the base of the machine so that the sharp end of the rod incised in the area between the base and the wings of the bracket, exerting a force parallel to the tooth surface in an occluso-apical direction (Fig. 1).
The force required to debond each bracket was registered in Newtons (N), and converted into Mega-Pascals as a ratio of Newtons to surface area of the bracket (MPa = N mm−2). We think that to properly compare different studies about bond tests in orthodontics, it is necessary to determine bond strength, because using force of debond we can not compare brackets with different geometries.
Adhesive remnant index
The percentage of the surface of the bracket base covered by adhesive was determined using an image analysis equipment (Sony dxc 151-ap video camera, connected to an Olympus SZ11 microscope) and MIP software.
The percentage of the area still occupied by adhesive remaining on the tooth after debonding was obtained by subtracting the area of adhesive covering the bracket base from 100%. Afterwards each tooth was assigned an adhesive remnant index (ARI) value according to the following criteria:10
0 = No adhesive left on the tooth
1 = Less than half of the adhesive left on the tooth
2 = More than half of the adhesive left on the tooth
3 = All the adhesive left on the tooth
Possible enamel fractures were also registered macroscopically.
Statistical analysis
The Kolmogorov-Smirnov normality test and the Levene variance homogeneity test were applied to the bond strength data. As the data did not show a normal distribution, significant difference was evaluated (P < 0.05) using the Kruskal-Wallis test, finding those groups which were significantly different with the Mann-Whitney test for two independent samples. In order to avoid an accumulation of errors due to mutiple comparisons, the significance level was modified dividing this (P < 0.05) between the number of comparisons made (Bonferroni Correction) and P < 0.008 was considered significant.
Bond strength data were also analyzed with Kaplan-Meier survival analysis using log Rank statistic (P < 0.05), finding those groups which were significantly different, comparing by pairs with the same test, taking the Bonferroni correction into account (P < 0.008).
ARI values were analyzed using the Pearson Chi-squared test and an analysis of corrected residuals. Both statistical tests were repeated grouping the cases in categories with 0 and 1 index points or 2 and 3 points, with the aim of avoiding categories showing an expected frequency lower than 5.
Enamel fractures were evaluated with the Pearson Chi-squared test and an analysis of corrected residuals.
A significance level P < 0.05 was set for both Pearson's Chi-squared test and the analysis of corrected residuals (residual > 2 implies P < 0.05).
The Kolmogorov-Smirnov test and the Levene homogeneity test of variances were applied to the data for percentage of area of bond remaining on tooth. As there was no homogeneity of variances in the groups, they were also analyzed using the Kruskal Wallis test and the Mann-Whitney test for two independent samples, taking the Bonferroni correction into account.
Results
Mann-Whitney test showed significant differences in shear bond strength between: 1) Light-Bond/Enhance-L.C. and Transbond-XT (P = 0.001) and 2) Light-Bond/Enhance-L.C. and Transbond-XT/Enhance-L.C (P = 0.001) (Table 1).
Kaplan-Meier survival analysis showed significant differences (P = 0.00) in shear bond strength. Significant differences were found between the same groups as those as when the Mann-Whitney test was applied (Fig. 2).
By means of the corrected residuals analysis it was observed that Transbond-XT and Transbond-XT/Enhance-L.C. were associated significantly for value 2 of ARI (residual = 3.3 and 5.4 respectively); Light-Bond and Light-Bond/Enhance-L.C. were significantly associated for value 1 (residual = 3.9 and 4.7 respectively) (Table 2).
In the same way, when cases were grouped into two categories, those showing 0 and 1 values and those showing 2 and 3 on the ARI, a significant association was observed between Transbond-XT and Transbond-XT/Enhance-L.C. for the '2&3' category (residuals = 3.3 and 5.4 respectively) and between Light-Bond and Light-Bond/Enhance-L.C. for the '0&1' category (residuals = 3.9 and 4.6 respectively) (Table 3).
The analysis of enamel fractures did not show significant differences (P = 0.22) between the groups; however, the analysis of corrected residuals indicated a significant association (residual = 2) between Transbond-XT and an absence of fractures (Table 2).
Values for the percentage of area of the tooth occupied by remaining adhesive are shown in Table 4. Significant differences were found between: 1) Light-Bond and Transbond-XT (P = 0.00); 2) Light-Bond and Transbond-XT/Enhance-L.C. (P = 0.00); 3) Light-Bond/Enhance-L.C. and Transbond-XT (p= 0.00); and 4) Light-Bond/Enhance-L.C. and Transbond-XT/Enhance-L.C. (P = 0.00) (Table 4).
Discussion
It has been suggested that a bond strength of between 5.8 and 7.8 MPa is more than sufficient for successful bonding for orthodontic purposes.11 All the groups evaluated showed values greater than this point of reference.
Our results showed that Enhance-L.C. produced a greater increase in bond strength for Light-Bond than for Transbond-XT, although the increase was not significant for either of the adhesives. Recent research has observed that there is no significant increase to bond strength when Enhance-L.C. was used with Light-Bond on new brackets, but when used on rebonded brackets there was a reduction (although not significant) in bond strength.12 Enhance-L.C. was already evaluated when applied to the base of rebonded brackets; its use did not achieve improved bonding.13
The 'adhesive remnant index' results and the analysis of the percentage of area of tooth occupied by adhesive indicated that Enhance-L.C. did not produce significant increases in the quantity of adhesive remaining on the enamel. These results agree with previous studies.12 It was observed that Light-Bond system left less adhesive on the enamel than Transbond-XT, whether or not either of the systems were used in combination with Enhance-L.C. This is an advantage as the cleaning procedures for adhesive left on the tooth after debonding is always accompanied by a certain loss of enamel.14 However it has been suggested that to avoid enamel fracture, the adhesive failure should occur between the bracket base and the adhesive rather than between the adhesive and the enamel.1 In our opinion the ideal adhesive should leave the least remanent on the tooth after debonding without producing enamel fractures.
As the highest values for bond strength were achieved with Light-Bond/Enhance-L.C., these being significantly higher than those obtained for Transbond-XT and Transbond-XT/Enhance-L.C., it may be said that Enhance-L.C. together with Light-Bond could be useful in cases where increased bond strength is required, for example when the patient is uncooperative, in areas were the control of humidity might be difficult, etc. Another advantage is that after the debonding procedure, there will not be much adhesive left on the tooth.
Enamel fracture was produced in all groups except when Transbond-XT was used exclusively. This might indicate a tendency for fractures to occur when bond strength exceeds a certain threshold, this being found in our study by Transbond-XT. Because of the irreversible nature of such lesions, we believe that this is not an unimportant issue in clinical orthodontics, although further research with a larger sample would be necessary in order to collate conclusive results.
For this reason a greater caution is advisable during debonding procedures whenever systems that provide a bond strength greater than the level mentioned are used, or perhaps it would be even better to avoid their use. Some authors have already indicated that adhesion promoters are not to be recommended for patients with enamel defects.15
Lastly, although the universal test machine is considered a standard when evaluating bond strength, we should remember that the results were obtained under laboratory conditions. In real practice bonding systems are exposed to numerous intra-oral factors.16 Nevertheless, laboratory testing remains a necessity for the initial evaluation of bonding systems.17
References
Urabe H, Rossouw PE, Titley KC, Ymin C . Combinations of etchants, composite resins, and bracket systems: An important choice in orthodontic bonding procedures. Angle Orthod 1999; 69: 267–274.
O'Brien KD, Read MJ, Sandinson RJ, Roberts CT . A visible light-activated direct-bonding material: an in vivo comparative study. Am J Orthod Dentofac Orthop 1989; 95: 348–355.
Underwood ML, Rawls HR, Zimmerman BF . Clinical evaluation of a fluoride- exchanging resin as an orthodontic adhesive. Am J Orthod Dentofac Orthop 1989; 96: 93–99.
Ray NJ . Aspects of adhesion in dentistry-Part III: Adhesion promoters. J Irish Dent Assoc 1983; 29: 56–61.
Bowen RL, Marjenhoff WA . Development of an adhesive bonding system. Oper Dent 1992 (Suppl 5): 75–80.
Nakabayashi N, Kojima K, Masuhara E . The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res 1982; 16: 265–273.
Hotta K, Miura F, Nakabayashi N . Effect of 4-MET on bond stregth and penetration of monomers into enamel. Dent Mater 1992; 8: 173–175.
Eliades T, Eliades G . Orthodontic adhesives resins. In: Brantley W A, Eliades T (ed) Orthodontic materials. Scientific and clinical aspects. NewYork: Thieme, 2001. pp 201–220.
International Organization for Standarization. Dental materials-guidance on testing of adhesion to tooth structure. Geneva, Switzerland, 1994. ISO TR 11405.
Artun J, Bergland S . Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod 1984; 85: 333–340.
Reynolds IR . A review of direct orthodontic bonding. Br J Orthod 1975; 2: 171–178.
Chung CH, Fadem BW, Levitt HL, Mante FK . Effects of two adhesion boosters on the shear bond strength of new and rebonded orthodontic brackets. Am J Orthod Dentofac Orthop 2000; 18: 295–299.
Egan FR, Alexander SA, Cartwright GE . Bond strength of rebonded orthodontic brackets. Am J Orthod Dentofac Orthop 1996; 109: 64–70.
Bishara SE, VonWald L, Laffon JF, Jacobsen JR . Effect of altering the type of enamel conditioner on the shear bond strength of a resin-reinforced glass ionomer adhesive. Am J Orthod Dentofac Orthop 2000; 118: 288–294.
Newman GV, Newman RA, Sun BI, Ha J-LJ, Ozsoylu SA . Adhesion promoters, their effect on the bond strength of metal brackets. Am J Orthod Dentofac Orthop 1995; 108: 237–241.
Pickett KL, Sadowsky PL, Jacobson A, Lacafield W . Orthodontic in vivo bond strength: comparison with in vitro results. Angle Orthod 2001; 71: 141–148.
Büyükyilmaz T, Zachrison YO, Zachrison BU . Improving orthodontic bonding to gold alloy. Am J Orthod Dentofac Orthop 1995; 108: 510–518.
Acknowledgements
The authors thanks 3M Unitek Dental Products for supplying brackets free of charge.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Vicente, A., Bravo, L., Romero, M. et al. Bond strength of brackets bonded with an adhesion promoter. Br Dent J 196, 482–485 (2004). https://doi.org/10.1038/sj.bdj.4811178
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811178
This article is cited by
-
Physical and chemical mechanisms involved in adhesion of orthodontic bonding composites: in vitro evaluations
BMC Oral Health (2021)
-
An in vitro investigation of an adhesion promoter
British Dental Journal (2004)