Key Points
-
Previous studies have indicated that dental surgery is not a risk factor for sporadic CJD, but in variant CJD the tissue distribution of infectivity is much wider, raising concerns over transmission via dental surgical instruments.
-
A range of dental tissues were studied for the presence of the abnormal form of the prion protein, using a combination of immunohistochemistry and a sensitive Western blot assay.
-
Abnormal prion protein was detected in the trigeminal ganglia, tonsil and lymph nodes in variant CJD but not in sporadic CJDcases. Alveolar nerves, gingiva, dental pulp, tongue and salivary gland tissue were negative in all cases. Lymphoid tissues (including tonsil) were negative in sporadic CJD.
-
Since the presence of the abnormal form of the prion protein is associated with infectivity, these findings indicate that the highest levels of infectivity in dental tissues are likely to be found in the tonsil and associated lymphoid tissues. This does not exclude the presence of lower levels of infectivity in the negative tissues in our study.
-
These new findings will be of use to inform the risk assessment on dental tissues and variant CJD.
Abstract
Objective To study the distribution of disease-associated prion protein (PrP) in oral and dental tissues in variant CJD.
Design Prospective single centre autopsy based study.
Setting Within the National CJD Surveillance Unit, UK, 2000-2002.
Materials and methods Patients with suspected variant CJD undergoing autopsy where permission to remove tissues for research purposes had been obtained from the relatives. Fixed and frozen autopsy tissues from the brain, trigeminal ganglion, alveolar nerve, dental pulp, gingiva, salivary gland, tongue and tonsils were studied by Western blot, PET blot and immunocytochemistry to detect disease-associated PrP.
Results Disease-associated PrP was only detected in the brain, trigeminal ganglia and tonsils.
Conclusions The failure to detect disease-associated PrP in most dental and oral tissues will help inform ongoing risk assessments for dental surgery in relation to the possible iatrogenic transmission of variant CJD via dental instruments.
Similar content being viewed by others
Introduction
The transmissible spongiform encephalopathies or prion diseases are a group of rare fatal neurodegenerative disorders which occur as sporadic, familial and acquired diseases.1 The commonest of these disorders is the sporadic form of Creutzfeldt-Jakob disease (CJD), which is a worldwide disorder with a relatively uniform incidence of around one patient per million population per annum.2 These disorders, and the related animal diseases scrapie and bovine spongiform encephalopathy (BSE), are transmissible under both natural and experimental conditions, but the precise nature of the infective agent is uncertain. There is increasing evidence to support the prion hypothesis, which predicts that the agent is composed of a modified host-encoded protein, prion protein.1
The normal form of the prion protein, PrPC, is expressed at highest levels in neurones of the central nervous system, but has been detected in a wide range of other tissues.1 The disease-associated isoform, PrPSc, accumulates in the brain in all forms of prion disease and its presence is pathognomonic of these disorders.1 PrPSc has the same amino acid sequence as PrPC, but differs in its conformation, possessing a higher ß-sheet content, and existing in an aggregated state, which confers resistance to proteolytic cleavage.3 This property is exploited diagnostically; since none of the currently available antibodies to prion protein reliably distinguish PrPSc from PrPC, limited proteolytic digestion is employed to generate a protease-resistant cleavage product from PrPSc, named PrPres, under conditions in which PrPC is totally degraded.1,4 The detection of PrPres by Western blot analysis, PET blot or immunohistochemistry is a convenient marker of prion disease infectivity in tissues that can be used to inform risk assessment.4,5
Interest in prion diseases has been stimulated in recent decades by the emergence of BSE as an epidemic in UK cattle, and the occurrence of BSE-related disorders in other species.1,6,7 In 1996, the National Creutzfeldt-Jakob Disease Surveillance Unit in the UK identified a new form of human prion disease, now termed variant CJD.8 Since then, substantial experimental evidence has indicated that variant CJD is caused by exposure to the BSE agent, most likely by the oral route through the consumption of BSE-contaminated meat products.9,10,11,12
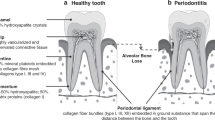
In most forms of human prion disease, the accumulation of PrPres is confined to the central nervous system and retina.13,14 However, the accumulation of PrPres in variant CJD tissues is more widespread than in sporadic CJD,4,5,13,15 suggesting a greater potential risk of secondary disease transmission by contaminated surgical instruments since prion infectivity is notoriously resistant to standard forms of decontamination.16,17,18 Although there is little evidence to suggest that dental surgery is a risk factor for sporadic or iatrogenic forms of CJD,2,19 the potential risk of secondary transmission of variant CJD posed by dentistry is currently unknown.17,18 Infectivity in dental tissues has been described in a rodent model of scrapie,20 and experimental inoculation of infected brain homogenate into the tongue and into dental pulp appears to be an efficient route of neuroinvasion.21 However, PrPres was undetectable in dental pulp samples from patients with sporadic CJD.22 Here we use Western blot, PET blot and immunohistochemical analysis of a range of oral and dental tissues taken at autopsy from patients with variant CJD for the presence of PrPres in order to determine whether this disease might pose a greater risk of secondary transmission by dental procedures than other forms of CJD.
Materials and Methods
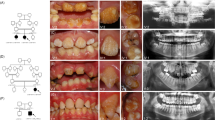
Tissues were obtained at autopsy from five cases of variant CJD (three males, two females, age range at death 26–53 years, duration of illness 7–18 months), one case of sporadic CJD (female, age at death 72 years and duration of illness two months, subtype VV2) and a single case of Lewy body dementia (used as a negative control for prion disease), where permission for research and retention of tissues had been obtained. LREC approval had been obtained for research on autopsy tissues on patients with CJD. The diagnosis was confirmed by neuropathological examination of the brain, and by Western blotting for PrPres in the brain. All cases of variant CJD showed PrPres accumulation in lymphoid tissues throughout the body (including cervical and submandibular nodes). The tissues sampled included brain, tonsil, tongue (full thickness, anterior and posterior regions), submandibular and parotid salivary glands (without lymph nodes), trigeminal ganglia, alveolar nerve (maxillary division) and inferior alveolar nerve, dental pulp and gingiva; not all tissues were available from each case. Dental pulp was obtained from non-restored molars from the lower mandible. Gingival tissue samples included both free and attached gingiva from the lower mandible. Tissues for Western blot analysis were snap frozen in liquid nitrogen at the time of autopsy. Tissues for histology were fixed in 10% buffered formalin for up to ten days following autopsy; these were immersed in 96% formic acid for one hour (to reduce infectivity in the tissue block) prior to washing and routine processing into paraffin wax.
Immunohistochemistry and PET blot
PrPres detection was performed on sections of formalin fixed, formic acid treated tissue by immunohistochemistry and the PET blot method. Paraffin sections of 5 μm were mounted on Superfrost plus slides (BDH) for immunohistochemistry and on nitrocellulose membrane (Bio-Rad) for PET blotting. Sections mounted on nitrocellulose were de-waxed and washed in TBST (10 mM Tris HCl pH 7.8, 100 mM NaCl, 0.05% Tween 20). After an overnight digestion in proteinase K (25 μg ml−1) at 55°C, digestion was terminated and protein denatured by immersing in 3M guanidine isothiocyanate for 10 mins. After washing in TBST, membranes were blocked with caesin before incubating in the primary antibody 3F4 (Dako) diluted 1/500 in blocking solution for two hours. Labelling was completed using a Vectastain ABC-Amplification detection system (Vector Laboratories). Labelling was visualised using NBT/BCIP (5-bromo-4-chloro-3 indolyl phosphate/ nitroblue tetrazolium) and observed using a stereomicroscope.
PrPres immunolabelling was carried out using the mouse monoclonal antibody, KG9 (Institute for Animal Health, Compton) in combination with a catalysed signal amplification kit (CSA) (Dako), in a protocol that distinguishes PrPres from PrPc. Briefly, after taking down to water, sections were pre-treated with a combination of hydrated autoclaving at 121°C for 10 mins, immersion in 96% formic acid for 5 mins and digestion with proteinase K at 100g ml−1 for 5 mins. After blocking with normal rabbit serum, non-specific binding of avidin and biotin was blocked using an avidin/biotin blocking kit (Vector Laboratories), before incubating in the primary antibody KG9 at 1/20,000 for 1 hour. Immunolabelling was completed using the CSA amplification kit, which is superior in terms of sensitivity to most other immunohistochemistry detection systems.23 Labelling was visualised using diaminobenzidene.
Western blot
Western blot analysis was carried out according to our previously published methods.4 Briefly, the low speed supernatant of a 10% (w/v) non-ionic detergent extract of frozen tissues was treated with proteinase K at 50 μg ml−1 for 1 hour at 37°C. Brain tissue (frontal cortex) was analysed without further treatment. The PrPres in dental tissues was first concentrated by centrifugation at 21,000 G for 1 hour at 4°C using the method of Lee et al.24 Pellets were dissolved in SDS-PAGE sample buffer and electrophoresed through 12% T SDS-PAGE minigels (Bio-Rad). Separated proteins were transferred using a semi-dry blotter (Bio-Rad) to Hybond-P membranes (Amersham Pharmacia Biotechnology). Detection employed the monoclonal antibody 3F4 (Dako) at 100 ng ml−1 IgG, horseradish peroxidase-conjugated anti-mouse antibody (generously provided by Diagnostics Scotland), ECL Plus and ECL Hyperfilm (both from Amersham Pharmacia Biotechnology).
Results
The results are summarised in Table 1. Western blotting resolves the protease-resistant core of PrPSc into three bands corresponding to di-, mono, and non-glycosylated PrPres.4 PrPres is abundant in variant CJD brain samples but undetectable in concentrated gingiva (0/3), dental pulp (0/2) and alveolar nerve (0/2) samples from the three cases of variant CJD examined. The detection of PrPres in a 1/5th dilution of a brain extract and the absence of signal from 20 fold concentrates of dental tissues suggests that PrPres, if present in these dental tissues, must be at a level less than 100 times that found in corresponding grey matter enriched brain samples (Fig. 1a). A second experiment using a larger amount (100 mg) of the most abundant dental tissue sample (gingiva) suggests that for this tissue the possible upper limit of PrPres accumulation is less than 1,000 times that found in the brain (Figs 1b and 1c). PrPres was not detectable in the only available dental tissue (gingiva) from another case of variant CJD; however, PrPres was detectable in samples of trigeminal ganglion and tonsil from this case when concentrated by an equivalent amount (Figs 2a and 2b). A third case of variant CJD had available samples of gingiva, dental pulp and alveolar nerve and these too proved to be negative for PrPres by Western blot (Fig. 3). Submandibular salivary gland tissue from two of these cases of variant CJD were also examined along with similar tissue from two further cases of variant CJD, a case of sporadic CJD and a case of Lewy body dementia. Each salivary gland sample was concentrated by a factor of 40 but in none of these was PrPres detectable (data not shown). Where possible, larger volumes of salivary gland extract were also concentrated, but these too proved negative.
Samples are from variant CJD case 1. The brain sample was loaded as a standard amount (0.5 mg tissue) and as a one fifth of the standard amount (0.1 mg tissue). The dental samples were analysed after centrifugal concentration of a twenty-fold greater amount of tissue (10 mg). A separate gingival sample from the same case of variant CJD was analysed after concentration of a greater amount of tissue (100 mg) (b and c) and given an optimal (b) or maximal (c) autoradiographic exposure.
In (b) the tonsil sample is flanked by standard positive control brain samples from sporadic CJD (left) and variant CJD (right). The brain samples in (a) and (b) were loaded as a standard amount (0.5 mg tissue) whereas the trigeminal ganglion, gingiva and tonsil samples were analysed after centrifugal concentration of a forty-fold greater amount of tissue (20 mg). Maximal exposure of (a) failed to reveal any signal in the gingival sample.
Standard positive control frontal cortex samples (brain) from variant CJD and sporadic CJD were alternated across the gel and loaded as a standard amount (0.5 mg tissue). The dental samples were analysed after centrifugal concentration of a forty-fold greater amount of tissue (20 mg). Maximal exposure failed to reveal any signal in the any of the dental samples.
Heavy deposits of PrPres were detected within brain tissue from sporadic and variant CJD cases, included as positive control material, using both immunohistochemistry and the PET blot method. In the dental tissue from three variant CJD patients, PrPres was not detected using either the highly sensitive immunohistochemistry method or the PET blot technique (Table 1 and Fig. 4). Salivary glands from these three cases were also examined using both immunodetection methods along with salivary glands from one further variant CJD case and a case of sporadic CJD. PrPres was not detected within the submandibular or parotid salivary gland in any of these cases in either serous or mucinous acini, or in ducts. Parotid lymph nodes were not examined, but submandibular and cervical lymph nodes from the variant CJD cases contained PrPres on immunocytochemistry. In each of the four variant CJD cases and the one sporadic CJD case, intense labelling for PrPres was observed within the ganglion cells of the trigeminal ganglia using immunohistochemistry (Fig. 4). The intensity of the labelling varied from cell to cell, but was present throughout all areas of the ganglion. The PET blot method was not carried out on these tissues. As expected, a trigeminal ganglion from a case of Lewy body disease showed no PrPres within the ganglion cells.
Discussion
Our studies have failed to detect PrPres in a series of dental tissues in patients with variant CJD apart from the tonsils, which were positive in all cases. The routine limits of detection of the assay suggest that if present PrPres must in all cases be at a level less than 1% of that found in brain. In certain samples of gingiva and salivary gland this upper limit can be further reduced to 1/1,000 of the level found in brain. In keeping with these findings, the two PrPres immunodetection methods for PrPres failed to demonstrate any evidence of PrPres accumulation in gingiva, dental pulp and alveolar nerve in two cases of variant CJD, even when the trigeminal ganglia (which innervates gum and dental pulp) were positive. Salivary glands from variant and sporadic CJD cases showed no detectable levels of PrPres. While these findings certainly offer a degree of reassurance with respect to the possible upper limit of any infectivity present in dental tissues in patients with vCJD, two important caveats should be borne in mind. First, no assay for PrPres has yet achieved the sensitivity of animal transmission studies in detection of the agent. Second, the exact relationship between infectivity and PrPres, as detected in assays such as these, remains a matter of some debate. Hence significant infectivity might yet be present in tissues where current techniques fail to detect PrPres.
Infectivity in lymphoid tissues in variant CJD is likely to be present in asymptomatic carriers who have been exposed to BSE for some considerable time before the onset of a neurological illness.15 PrPres was detected by immunocytochemistry in appendicectomy specimens which were removed 8 months and 2 years prior to the onset of neurological illness in patients with variant CJD; another specimen removed nine years before the disease onset was negative.25 Infectivity in tonsils is therefore likely to be present in asymptomatic carriers of variant CJD. Since at present we have no means of identifying these individuals, a precautionary approach to dealing with the prospects of iatrogenic disease transmission by surgical instruments seems appropriate.17
Although the numbers of cases studied is small, the results indicate that involvement of dental tissues in variant CJD may not differ from sporadic CJD.22 This situation is comparable with the failure to detect PrPres in peripheral nerves in variant CJD,5 despite the fact that PrPres can be detected in dorsal root ganglia and spinal cord.4 Further studies are required to confirm these preliminary findings, but the difficulties in obtaining consent for autopsy with permission for retention of tissues for research and the technical difficulties involved in acquiring adequate specimens should not be underestimated.
Animal models of prion diseases have also been used to study the routes of neuroinvasion following peripheral exposure to prion agents.26,27 These studies have shown that several routes of neuroinvasion are possible, depending on the strain of the agent used, the host species used for the model and the route of inoculation. These models have also demonstrated that centrifugal spread of infectivity from the brain can occur after neuroinvasion has been established. This finding may be relevant to the results presented here, since the identification of PrPres in trigeminal ganglia, but not in the peripheral branches of the nerve in the gum and dental pulp, would be consistent with centrifugal spread from the brain. The same may apply to previous findings in the dorsal root ganglia and peripheral nerves in variant CJD.
Both infectivity and PrPres have both been detected in dental tissues (including salivary gland and tongue) in experimental models of prion diseases;20,21,27,28 however, these studies have generally employed models where levels of infectivity both in the nervous system and in other tissues are likely to be higher than those encountered in human prion diseases.29 Accordingly, the relevance of these studies to human diseases can be questioned, but there is a need for more sensitive and specific means of detection of PrPres in human tissues and fluids, which might also allow the development of screening tests for asymptomatic carriers who are incubating variant CJD. Recent studies on animal models have also suggested that the tongue and gingiva might represent site of transmission for prion diseases.20,21 A case control study on variant CJD has not yet identified any significant difference between cases and controls in terms of the history of dental surgery and other surgical procedures (Dr H. Ward, personal communication).
Our findings will help inform the ongoing risk assessment for exposure of surgical instruments to infectivity in variant CJD.30,31 In terms of dental surgery, the most significant infectivity will be encountered in the tonsils (including the pharyngeal, palatine and lingual tonsils). In variant CJD there is also a theoretical risk that blood may also contain PrPres and carry infectivity, but no direct evidence for this is available.5,29 However, both BSE and scrapie have recently been transmitted experimentally by blood transfusion in a sheep model.32 Since the distribution of infectivity in the sheep model of experimental BSE is similar to that in variant CJD, this finding has reinforced concerns about potential infectivity in blood in variant CJD, which have been addressed in various precautionary measures by the national blood authorities in the UK. The significance of prion infectivity in tonsils for dental surgery has been considered in recent reviews;17,18,31 recent measures from the Department of Health to improve standards of cleaning and decontamination of surgical instruments are likely to help reduce these risks, even given the difficulties associated with decontamination in prion disease.31,33 The results of ongoing research into means of improving decontamination and cleaning techniques for surgical instruments is awaited with interest, as these are likely not only to help reduce risks of variant CJD transmission, but also the risks of transmission of other infectious agents via surgical instruments.16,33
References
Prusiner SB . Prions. Proc Natl Acad Sci USA 1998; 10: 13363–13383.
Ward HJT, Everington D, Croes EA, et al. Sporadic Creutzfeldt-Jakob disease and surgery – a case-control study using community controls. Neurology 2002; 59: 543–548.
Harrison PM, Bamborough P, Daggett V, Prusiner SB, Cohen FE . The prion folding problem. Curr Opin Struct Biol 1997; 7: 53–59.
Ironside JW, Head MW, Bell JE, McCardle L, Will RG . Laboratory diagnosis of variant Creutzfeldt-Jakob disease. Histopathology 2000; 37: 1–9.
Wadsworth JDF, Joiner S, Hill AF, et al. Tissue distribution of protease resistant prion protein in variant Creutzfeldt-Jakob disease using a highly sensitive immunoblotting assay. Lancet 2001; 358: 171–180.
Wilesmith JW, Wells GA, Cranwell MP, Ryan JB . Bovine spongiform encephalopathy: epidemiological studies. Vet Rec 1988; 123: 638–644.
Anderson RM, Donnelly CA, Ferguson NM, et al. Transmission dynamics and epidemiology of BSE in British cattle. Nature 1996; 382: 779–788.
Will RG, Ironside JW, Zeidler M, et al. A new variant of Creutzfeldt-Jakob disease in the UK. Lancet 1996; 347: 921–925.
Collinge J, Sidle KC, Meads J, Ironside J, Hill AF . Molecular analysis of prion strain variation and the aetiology of 'new variant' CJD. Nature 1996; 383: 685–690.
Bruce ME, Will RG, Ironside JW, et al. Transmissions to mice indicate that 'new variant' CJD is caused by the BSE agent. Nature 1997; 389: 498–501.
Hill AF, Desbruslais M, Joiner S, et al. The same prion strain causes vCJD and BSE. Nature 1997; 389: 448–450.
Scott MR, Will R, Ironside J et al. Compelling transgenetic evidence for transmission of bovine spongiform encephalopathy prions to humans. Proc Natl Acad Sci USA 1999; 96: 15137–15142.
Hill AF, Butterworth RJ, Joiner S, et al. Investigation of variant Creutzfeldt-Jakob disease and other human prion diseases with tonsil biopsy samples. Lancet 1999; 353: 183–189.
Head MW, Northcott V, Rennison K et al. Prion protein accumulation in eyes of patients with sporadic and variant Creutzfeldt-Jakob disease. Invest Ophthalmol Vis Sci 2003; 44: 342–346.
Hilton DA, Fathers E, Edwards P, Ironside JW, Zajicek J . Prion immunoreactivity in appendix before the clinical onset of variant Creutzfeldt-Jakob disease. Lancet 1998; 325: 703–704.
Bebermeyer RD, Powell JF, Hobdell MH, Durban EM . Dental practice implications of prion diseases. Quinessence Int 2003; 34: 38–44.
Gill DS, Tredwin CJ, Gill SK, Ironside JW . The transmissible spongiform encephalopathies (prion diseases): a review for dental surgeons. Int Dent J 2001; 51: 439–446.
Whitworth CL . Variant Creutzfeldt-Jakob disease – a problem for general dental practitioners. Prim Dent Care 2002; 9: 95–99.
Collins S, Law MG, Fletcher A, et al. Surgical treatment and risk of sporadic Creutzfeldt-Jakob disease: a case-control study. Lancet 1999; 353: 693–697.
Ingrosso L, Pisani F, Pocchiari M . Transmission of 263K scrapie strain by the dental route. J Gen Virol 1999; 80: 3043–3047.
Bartz JC, Kincaid AE, Bessen RA . Rapid prion neuroinvasion following tongue infection. J Virol 2003; 77: 583–591.
Blanquet-Grossard F, Sazdovitch V, Jean A, et al. Prion protein is not detectable in dental pulp from patients with Creutzfeldt-Jakob disease. J Dent Res. 2000; 79: 700.
Sabattini E, Bisgaard K, Asacani S, et al. The En Vision++ system: a new immunohistochemical method for diagnostics and research. Critical comparison with the APAAP, ChemMate, CSA, LABC and SABC techniques. J Clin Pathol 1998; 51: 506–511.
Lee DC, Stenland CJ, Hartwell RC, et al. Monitoring plasma processing steps with a sensitive Western blot method for the detection of prion protein. J Virol Methods 2000; 84: 77–89.
Hilton DA, Ghani AC, Conyers L, et al. Accumulation of prion protein in tonsil and appendix: review of tissue samples. Br Med J 2002; 321: 633–634.
Foster JD, Parnham DW, Hunter N, Bruce M . Distribution of the prion protein in sheep terminally affected with BSE following experimental oral transmission. J Gen Virol 2001; 82: 2319–2326.
Hadlow WJ, Race RE, Kennedy RC . Temporal distribution of transmissible mink encephalopathy virus in mink inoculated subcutaneously. J Virol 1987; 61: 3235–3240.
Skaguchi S, Katamine S, Yamanouchi K, et al. Kinetics of infectivity are dissociated from PrP accumulation in salivary glands of Creutzfeldt-Jakob disease agent-inoculated mice. J Gen Virol 1993; 74: 2117–2123.
Bruce ME, McConnell I, Will RG, Ironside JW . Detection of variant Creutzfeldt Jakob disease infectivity in extraneural tissues. Lancet 2001; 358: 208–209.
Gonzales TS, Rushing EJ . Bad news and good news: what the dentist needs to know about transmissible spongiform encephalopathies. Quinessence Int 1998; 29: 319–321.
Porter S, Scully C, Ridgway GL, Bell J . The human transmissible spongiform encephalopathies (TSEs): implications for dental practitioners. Br Dent J 2000; 188: 432–436.
Hunter N, Foster J, Chong A, et al. Transmission of prion diseases by blood transfusion. J Gen Virol 2002; 83: 2897–2905.
Smith A, Dickson M, Aitken J, et al. Contaminated dental instruments. J Hosp Infection 2002; 51: 233–235.
Acknowledgements
The authors would like to thank all the Neuropathologists and their technical staff in the UK for their support of the National CJD Surveillance Unit. We also thank the laboratory staff in the unit for invaluable technical support. The National CJD Surveillance Unit is funded by the Department of Health and the Scottish Executive. The Unit is a member of the EC funded projects PRIONET (QLK2-CT-2000-00837) and TSELAB (QLK2-CT-2002-81532).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Head, M., Ritchie, D., McLoughlin, V. et al. Investigation of PrPres in dental tissues in variant CJD. Br Dent J 195, 339–343 (2003). https://doi.org/10.1038/sj.bdj.4810536
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4810536
This article is cited by
-
Wide distribution of prion infectivity in the peripheral tissues of vCJD and sCJD patients
Acta Neuropathologica (2021)
-
Risk factors for variant Creutzfeldt-Jakob disease in dental practice: a case-control study
British Dental Journal (2012)
-
Risk management in clinical practice. Part 4. Endodontics
British Dental Journal (2010)
-
Dental treatment and risk of variant CJD – a case control study
British Dental Journal (2007)
-
Cleanability of dental instruments – implications of residual protein and risks from Creutzfeldt-Jakob disease
British Dental Journal (2007)