Abstract
It is appreciated that phagocytosis of apoptotic cells (AC) is an immunological relevant process that shapes the pro- versus anti-inflammatory macrophage phenotype. It was our intention to study the respiratory burst, a prototype marker of macrophage activation, under the impact of AC. Following incubation of RAW264.7 macrophages with AC, we noticed attenuated production of reactive oxygen species (ROS) in response to PMA treatment, and observed a correlation between attenuated ROS formation and suppression of protein kinase Cα (PKCα) activation. EMSA analysis demonstrated an immediate activation of peroxisome proliferator-activated receptor-γ (PPARγ) following supplementation of AC to macrophages. In macrophages carrying a dominant-negative PPARγ mutant, recognition of AC no longer suppressed PKCα activation, and the initial phase of ROS formation was largely restored. Interference with actin polymerization and transwell experiments suggest that recognition of AC by macrophages suffices to attenuate the early phase of ROS formation that is attributed to PPARγ activation.
Similar content being viewed by others
Introduction
Cells entering the route of programmed cell death are recognized by professional phagocytes. The uptake of dying cells before the cell membrane integrity is lost averts an inflammatory response in the surrounding tissue by preventing contact of neighboring cells with cellular constituents of dying cells.1 It became apparent that phagocytosis of apoptotic cells (AC) by macrophages is an immunologically relevant process that shapes the pro- versus anti-inflammatory cellular macrophage phenotype, provoking cell desensitization. This is characterized by the release of anti-inflammatory cytokines such as TGFβ and the suppression of proinflammatory cytokine production.1 The engulfment of AC by macrophages also attenuates NO production, as determined by decreased nitrite levels following LPS/IFNγ stimulation.2 Thus, clearance of AC must be considered as an immune regulatory process that is not species specific because major determinants for recognition are conserved between human and murine cells.3
Professional phagocytes produce reactive oxygen species (ROS) during phagocytosis of pathogens, which is considered a prototype marker of cell activation. The oxidative burst is triggered by a multicomponent NADPH oxidase protein complex.4 Stimulation of macrophages with the phorbol ester PMA provokes phosphorylation of p47phox, one of the cytosolic components of NADPH oxidase.5 Phosphorylation initiates translocation of a preformed p47phox/p67phox complex to the cell membrane where it interacts with flavocytochrome b5586 to assemble the active NADPH oxidase. For human monocytes and RAW264.7 macrophages, it has been shown that the primary event, that is, phosphorylation of p47phox, is facilitated by protein kinase Cα (PKCα).7, 8 Recently, we demonstrated that downregulation of PKCα or expression of a kinase-dead mutant attenuates the PMA-induced oxidative burst.9 However, the impact of AC on the oxidative burst remains unknown.
One candidate recognized for its ability to desensitize macrophages is the peroxisome proliferator-activated receptor-γ (PPARγ),10 belonging to the nuclear hormone receptor superfamily.11 Ligand binding activates PPARγ, causes heterodimer formation with the retinoic X receptor (RXR) and binding to peroxisome proliferator response elements (PPRE) in the promoter region of responsive genes. This is in contrast to the PPARβ/RXR heterodimer that constitutively binds to the DNA.12 Besides transcriptional regulation via direct DNA binding, PPARγ attenuates gene expression by scavenging other transcription factors such as NF-κB13 or by hindering transcriptional cofactors to exert their costimulatory role. These effects are mediated by direct protein–protein interactions.14
It was our intention to characterize the oxidative burst of macrophages following the uptake of AC. ROS formation was attenuated by recognition of AC and correlated with the inability to activate PKCα. Moreover, the initial but not the later phase of ROS suppression was reversed in macrophages carrying a dominant-negative mutant of PPARγ (d/n PPARγ), whereas PKCα-overexpressing cells could not be sensitized. Blocking phagocytosis with cytochalasin D,15 and transwell experiments indicated that binding of AC to macrophages suffices in attenuating early cell activation. We conclude that recognition of apoptotic cell debris by macrophages is an immunologically relevant anti-inflammatory process that controls the macrophage oxidative burst.
Results
AC attenuate nitrite- and ROS formation in macrophages
First, we verified the anti-inflammatory effect of apoptotic Jurkat cells (AC) on RAW264.7 macrophages by following nitrite formation in the cell supernatant. Both AC and TGFβ attenuated LPS/INFγ-stimulated nitrite formation as previously described.2 Throughout the study, attenuated nitrite formation was followed as a marker indicating activation of anti-inflammatory pathways in macrophages. We then tested whether AC might affect ROS formation in RAW264.7 macrophages (Figure 1). With an initial experiment, we ruled out that coincubations of either apoptotic or necrotic Jurkat cells with macrophages produced ROS (Figure 1a and c). In contrast, stimulation of macrophages with PMA produced ROS-formation as detected by the rightward shift of the hydroethidine (HE) signal. Pre-incubating macrophages with AC for 1 h followed by PMA stimulation reduced ROS formation by roughly 50% (Figure 1b), whereas coincubations with necrotic cells did not impair ROS production (Figure 1d). This supports the finding of others that necrotic cells do not affect RAW264.7 cells.16 Exposing macrophages for 1 h to 5 ng/ml TGFβ neither provoked ROS formation on its own (Figure 1e), nor did TGFβ block the response towards PMA (Figure 1f). Statistical evaluation of these findings is shown in Figure 1g. It is interesting that AC as well as TGFβ attenuated nitrite formation but TGFβ differed from AC in the ability to suppress ROS formation at early times.
ROS production in response to apoptotic or necrotic Jurkat cells and TGFβ. ROS production in RAW264.7 macrophages was analyzed by flow cytometry using 3 μM HE as the redox-sensitive dye as described in Materials and Methods. Cells were stimulated with 1 μM PMA (unfilled dark gray traces) or remained as controls (black traces). (a) AC were preincubated for 30 min (filled light gray), (b) AC were preincubated for 1 h with subsequent PMA addition (filled light gray), (c) Necrotic cells were preincubated for 30 min (filled light gray), (d) Necrotic cells were preincubated for 1 h with subsequent PMA addition (filled light gray), (e) 5 ng/ml TGFβ was preincubated for 30 min (filled light gray), (f) TGFβ was preincubated for 1 h with subsequent PMA addition (filled light gray). (g) Statistical evaluation of (a–f). The shift of the peak medians from untreated cells to PMA-treated cells was set as 100% activation and any inhibition was calculated proportionally. Data are the S.E.M. of at least three different experiments (*P≤0.05 versus PMA-stimulated controls). (h–m) Successful removel of AC from RAW264.7 cells was confirmed by fluorescent microscopy. AC were stained with DiI for 30 min before addition to macrophages. After 1 h, AC were removed by washing two times with PBS. Pictures show RAW264.7 cells that remained untreated (h; phase contrast; i; red flourescence), exposed to AC (j; phase contrast; k; red flourescence) and exposed to AC followed by washing two time with PBS (l; phase contrast; m; red fluorescence). Data are representative of at least three individual experiments
To exclude an impact of Jurkat cell protein on responses followed in macrophages we proved that AC are washed off from macrophages before any further analysis in macrophages. We exposed RAW 264.7 cells for 1 h to 1,1′dioctadecyl-3,3,3′,3′-tetramethyl-indocarbocyanine perchlorate (DiI) (red fluorescent dye)-stained AC, washed macrophages twice with PBS and analyzed macrophages by fluorescent microscopy (Figure 1h–m). Except for a few particles, taken up by phagocytosis, apoptotic Jurkat cells were removed by washing. Routinely using the washing procedure in our experiments excludes the variations in the protein amount or ROS originating from contaminating AC.
To obtain supporting documentation that AC attenuate ROS formation we followed PKCα expression. Considering that subsequent to PKCα activation by PMA, PKCα translocates to the membrane, a decrease of cytosolic PKCα is indicative of its prior activation. Figure 2a shows protein expression of PKCα in RAW264.7 macrophages, which is not significantly altered when AC and macrophages are cocultured. As predicted, PMA addition for 1–6 h provoked PKCα activation. A cotreatment of macrophages with AC and PMA for 1 h completely blocked PKCα migration to the membrane. At 3 h, AC attenuated PMA-induced PKCα activation to a minor extent only, and the inhibitory effect was gone at 6 h. Figure 2b shows the statistical evaluation of PKCα levels during the first hour, when inhibition of PKCα activation by AC was most prominent. Neither necrotic nor vital Jurkat cells influenced PKCα activation.
PKCα activation in response to PMA and apoptotic cells. (a) Cytosolic expression of PKCα and actin was determined in control RAW264.7 macrophages, following the addition of apoptotic Jurkat cells (AC), 100 nM PMA, or a combination of PMA and AC. Treatments were for 1, 3 or 6 h. (b) Statistical evaluation of Western blot data for 1 h treatments. (c) PKCα protein levels in the cytosolic versus membrane fractions were determined in control RAW264.7 macrophages, following the addition of 100 nM PMA, or a combination of PMA and AC. Treatments were for 1 h. For details see Materials and Methods. Data are the S.E.M. of at least three different experiments or are representative of at least three individual experiments
To further prove that PKCα activation and subsequent cytosol to membrane translocation is inhibited, we analyzed cytosolic versus the membrane fractions (Figure 2c). As expected, PMA provoked PKCα translocation to the membrane, whereas coincubations with AC attenuated its translocation. To rule out that Jurkat protein may affect PKCα amounts detected by Western analysis we compared the amount of total protein recovered in samples with or without AC, but failed to notice any difference. Thus, we rule out that Jurkat protein affects protein analysis in macrophages. We conclude that AC suppress activation of PKCα and ROS production in macrophages after 1 h, but the effect vanishes after 3–6 h.
PPARγ modulates the oxidative burst in macrophages
In order to obtain more information on potential signaling pathways induced by AC in regulating the oxidative burst, we considered the established anti-inflammatory behavior of PPARγ by focusing on early events of macrophage activation occurring within 1 h. Exposing RAW264.7 macrophages for 15–60 min to AC, we noticed a transient activation of PPARγ, which was most prominent at 15 min (Figure 3a). Thereafter, activation declined during the first hour, reaching nonstatistical values compared to resting macrophages after 45 min. Statistical analysis of EMSA data are shown in Figure 3b.
Activation of PPARγ in RAW264.7 macrophages. (a) EMSA analysis of PPARγ activation in untreated RAW264.7 macrophages (upper panel), in macrophages cocultured with AC (+AC; middle panel) and upon coculture of AC with macrophages carrying a d/n PPARγ mutant (lower panel). Following stimulation for 15–60 min, EMSA analysis was performed as described under Materials and Methods. For controls (upper panel) cell stimulation was omitted. (b) Statistical evaluation of results obtained by EMSA analysis. Untreated controls are set as one. Data represent the S.E.M. of at least three individual experiments (*P≤0.05 versus unstimulated RAW264.7). (c) RAW264.7 macrophages carrying a d/n PPARγ mutant were exposed to AC and/or 100 nM PMA for 1 h or remained as controls as indicated. Expression of PKCα and actin were followed by Western analysis. (d) Statistical analysis of the PKCα Western blots as shown in c. Data represent the S.E.M. of three individual experiments (*P≤0.05 versus untreated controls)
To address the role of PPARγ in the oxidative burst we eliminated PPARγ in RAW264.7 macrophages by retroviral transduction of a d/n PPARγ mutant. Exposing macrophages carrying the d/n PPARγ to AC showed no activation of PPARγ (Figure 3a). In the following experiments, we used d/n PPARγ macrophages to analyze PKCα expression (Figure 3c). Cytosolic expression of PKCα remained unaffected when exposed to AC but was activated when stimulated with PMA. This situation is comparable to the behavior of parent cells, documented in Figure 2b. However, parent and d/n PPARγ macrophages behaved different when exposed to AC and simultaneously stimulated with PMA. While translocation of PKCα was completely prevented in parent cells (Figure 2b), activation of PKCα in d/n PPARγ cells was significantly higher when treated with the combination AC/PMA compared to controls (Figure 3c). The statistical evaluation of these data is shown in Figure 3d.
Considering that PPARγ is necessary to attenuate PKCα activation, we now use d/n PPARγ compared to parent macrophages to examine ROS-formation with AC being pre-exposed (Figure 4). Adding AC to parent RAW264.7 macrophages attenuated PMA-evoked ROS formation. This was evident when AC were preincubated for 1 h, with more pronounced inhibition seen at preincubation periods of 3 or 6 h (Figure 4a, c and e). Exposing d/n PPARγ macrophages for 1 h to AC before PMA addition did not block ROS production at all (Figure 4b). The response was indistinguishable from the PMA effect but was different from the situation seen in parent cells (compare Figure 4b and a). However, prolonging coincubation periods of d/n PPARγ macrophages with AC reduced inhibition of ROS formation at a 3-h preincubation period, which became more pronounced after 6 h (Figure 4d and f). The statistical evaluation of these observations is presented in Figure 4g. Evidently, inhibition of ROS production in response to PMA is instantaneously attenuated in parent macrophages by the exposure to AC, and increases from roughly 40% at 1 h to 60% at 6 h. The situation in d/n PPARγ macrophages is different. During early times of AC addition, that is, at a 1-h preincubation period there is no inhibition while blockage of ROS formation became comparable to parent cells with a prolonged AC exposure of 6 h. This implies a biphasic inhibitory effect with only the early phase being PPARγ dependent. Therefore, PMA-evoked ROS formation in d/n PPARγ macrophages upon recognition of AC correlated at least in part with expression modulation, that is, activation of PKCα as shown in Figure 3d.
ROS production in response to AC in RAW264.7, d/n PPARγ or PKCα-overexpressing macrophages. ROS production in parent and d/n PPARγ transduced RAW264.7 macrophages was analyzed by flow cytometry using 3 μM HE as the redox-sensitive dye. Cells were stimulated with 1 μM PMA (unfilled dark gray traces) or remained as controls (black traces). Apoptotic cells were added for 1, 3 or 6 h before PMA addition. (a–b) AC were preincubated for 1 h prior to PMA addition (filled light gray), (c–d) AC were preincubated for 3 h before PMA addition (filled light gray), (e–f): AC were preincubated for 6 h before PMA addition (filled light gray). (g) Statistical examination of results presented in a–f. The shift of the peak medians from untreated cells to PMA-treated cells was set as 100% activation, and any inhibition was calculated proportionally. (h) ROS production in PKCα-overexpressing RAW264.7 macrophages was analyzed by flow cytometry using 3 μM HE. Cells were stimulated with 1 μM PMA (unfilled dark gray traces) or remained as controls (black traces). AC were preincubated for 1 h before PMA addition (filled light gray). (i) Statistical evaluation of data shown in h. Data represent the S.E.M. of at least four individual experiments (*P≤0.05 versus RAW264.7)
To further prove an involvement of PKCα in attenuating ROS production, we used PKCα-overexpressing cells.9 Coincubations with AC before PMA activation left the oxidative burst unaltered, that is, comparable to PMA addition (Figure 4h) with statistical evaluation as shown in Figure 4i. This supports the idea that inhibition of ROS formation is a consequence of attenuated PKCα activation.
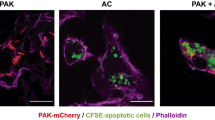
AC recognition is sufficient to attenuate PKCα activation by PMA
To elucidate whether the impact of apoptotic Jurkat cells on macrophages requires cell–cell contacts we performed transwell experiments. In these experiments, AC and macrophages were separated by a permeable membrane that only allowed the passage of diffusible messengers. As shown in Figure 5a, separation of AC and macrophages allowed activation of PKCα following PMA addition, which points to the requirement of direct cell-to-cell interactions, excluding the involvement of paracrine signaling. We then asked whether engulfment of AC would be required to modulate PKCα activation or whether intercellular contacts would suffice. Experimentally, we used cytochalasin D, an inhibitor of actin polymerization, to block phagocytosis of AC (Figure 5b). As expected, cytochalasin D alone did not modulate cytosolic PKCα expression or PMA-induced PKCα activation. When treating macrophages with the combination of cytochalasin D, AC and PMA, translocation of PKCα was suppressed. This indicates that phagocytosis of apoptotic material is not needed for AC to convey their signal.
Roles of phagocytosis and paracrine signaling in modulating PKCα activation. (a) A transwell set up was used to separate apoptotic Jurkat cells from macrophages. Not allowing a direct cell–cell contact, macrophages were exposed to AC and/or 100 nM PMA for 1 h or remained as controls. Cytosolic expression of PKCα and actin were followed by Western analysis. (b) RAW264.7 macrophages were exposed to AC, 2 μM cytochalasin D (cyto D) and/or 100 nM PMA for 1 h or remained as controls as indicated. Cyto D was preincubated for 45 min. Translocation of PKCα was determined as indicated under Materials and Methods. Blots are representative for three individual experiments
Discussion
It is appreciated that macrophages, following recognition/elimination of AC, acquire an altered inflammatory program when challenged with innate stimuli.17 This is reflected among other changes by decreased TNFα or NO formation1, 2 but an increased production of PGE2 or TGFβ1.18 The ability of TGFβ and AC to attenuate nitrite formation in macrophages was corroborated in our study, indicating the suitability of our test system. For most experiments, we used a macrophage-AC coculture period of 1 h. During this period, the population of Jurkat cells exclusively revealed apoptotic markers, implying that alterations seen in macrophages are associated with the impact of apoptotic rather than necrotic or viable cells.
ROS formation is an early marker of macrophage activation, and is important in bactericidal activity. Activation of NADPH oxidase requires PKCα activation in order to facilitate phosphorylation of p47phox and thus assembly of the functional oxidase complex.5 Inherent to PKCα activation one finds protein translocation to the plasma membrane, which is a correlative marker for kinase activation.19 Our data extends existing knowledge on the ability of AC to modulate the macrophage behavior by attenuating PMA-evoked ROS formation in RAW264.7 cells.20 In our experiments, AC attenuated ROS generation and preserved cytosolic PKCα expression, indicating that the kinase was not activated by PMA. This suggests that the primary step in NADPH oxidase activation, that is, PKCα activation, was inhibited. Interestingly, ROS suppression was not shared by TGFβ signaling, implying that different signaling pathways affect inhibition of NO versus ROS formation. Although TGFβ has been proposed as an important mediator of AC in reprogramming macrophages,18 other studies suggested that TGFβ does not affect the initial anti-inflammatory response following AC recognition such as modulating NF-κB activity.15 This is consistent with our observation that early regulation of ROS production is TGFβ independent.
Recent information implies a role for PPARγ in inflammation control.10 Activation of PPARγ can be achieved by fatty acid metabolites, including those of the arachidonic acid cascade.12 Immunosuppressive functions are largely mediated through the ability of PPARγ to transrepress the activities of transcription factors such as NF-κB, STATs or NFAT.10 One may assume that recognition of AC generates lipid-based signals needed for PPARγ activation. This hypothesis is supported by the notion that uptake of oxidized lipoproteins (oxLDL), which is facilitated at least in part by receptors also involved in the uptake of AC, that is, CD36, promotes PPARγ activation.21 There is evidence that oxidation of lipid components, for example, phosphatidylserine, at the outer membrane of AC is required as a recognition signal that allows phagocytosis of AC.22 One can speculate whether oxidized lipid components of AC, in some analogy to oxidized lipid components of oxLDL, account for PPARγ activation and whether signals are transmitted via CD36. Furthermore, AC have been shown to release phospholipids such as lysophosphatidylcholine, which influence the macrophage behavior.23 Recently, it was shown that oxidized eicosanoids24 or lysophosphatidic acid25 may provoke PPARγ activation, and thus represent possible PPARγ activation signals.
Our study shows a rapid and transient activation of PPARγ by AC within 1 h, which is correlated to attenuated ROS production and preserved PKCα expression that otherwise translocates to the membrane because of PMA addition. A direct role of PPARγ was proven in d/n PPARγ-expressing macrophages. These cells, despite AC treatment, generated ROS and revealed decreased cytosolic expression of PKCα in response to PMA. Interestingly, it has been reported that rosiglitazone, known to activate PPARγ, partially inhibits oxLDL-induced PKC activity26 and blocks PKCδ signaling.27 Furthermore, the absence of ROS inhibition in PKCα-overexpressing cells supports the central role of PKCα in regulating the oxidative burst. Although mechanistic insights to explain how PPARγ might block PKCα activation and subsequent NADPH oxidase assembly await clarification, (in)direct protein–protein interactions of PKCα with PPARγ and/or the degree of phosphorylation of PKCα by either attenuating kinases or stimulating phosphatases appear testable approaches. Direct interactions of PPARs with other cytosolic proteins has been shown,28 which supports the assumption that a similar mechanism may apply to the interaction of PKCα and PPARγ. Besides short-term activation as seen in this study, PPARγ is also involved in long-term regulation of ROS formation,29 and thus accounts for an alternative mechanism to regulate ROS production at later time points. Again, this hypothesis will be tested in the future. The controversy about whether RAW264.7 macrophages indeed express PPARγ has been settled by showing that these cells express PPARγ mRNA30 and protein31 as well as its activation in response to LPS/IFNγ.32 Our data on EMSA analysis, reporter activity and elimination of PPARγ effects by transduction of a d/n PPARγ mutant corroborated these findings.
Following suggestions that soluble factors released from AC may influence macrophages,17 we performed transwell experiments which ruled out the involvement of paracine signaling. Moreover, experiments with cytochalasin D suggested that cell–cell contacts rather than phagocytosis of apoptotic material suffices in attenuating ROS formation. This supports findings by others showing that binding of AC to macrophages was sufficient in exerting anti-inflammatory effects.15 The finding that ROS production is not completely inhibited although PKCα is apparently translocated at later time points suggests that PKCα may not be the exclusive factor responsible for the PMA-induced oxidative burst.
In summary, our study shows that binding of AC to murine macrophages attenuates the oxidative burst via an early PPARγ-dependent inhibition of PKCα activation.
Materials and Methods
Materials
PMA, staurosporine, cytochalasin D and LPS were purchased from Sigma (Deisenhofen, Germany). HE and DiI were obtained from Molecular Probes (Leiden, The Netherlands). Murine rIFNγ and the alkaline phosphatase-labeled antidigoxigenin (DIG) antibody were from Roche Diagnostics (Mannheim, Germany). Culture supplements and FCS were ordered from Biochrom (Berlin, Germany). Oligonucleotides were bought from Eurogentec (Seraing, Belgium). Antiactin antibody was purchased from Amersham Bioscience (Freiburg, Germany). Mouse anti-PKCα and TGFβ were obtained from BD Biosciences (Heidelberg, Germany). All chemicals were of the highest grade of purity and were commercially available.
Vector construction
To suppress PPARγ signaling in RAW264.7. macrophages, a PPARγ d/n mutant (PPARγ-AF2), kindly provided by Prof. Chatterjee, Department of Medicine, University of Cambridge, UK, was used. There are two mutations in the AF2 domain (Leu468Ala/Glu471Ala), thus impairing ligand binding and concomitant ligand-dependent PPARγ activation.33 The mutant was subcloned into a retroviral vector system to allow efficient gene transfer and genomic integration of the gene. Therefore, it was transferred into the HpaI site of the multicloning site of the retroviral pLXIN vector (Clontech, BD Biosciences, Heidelberg, Germany). Primers were designed to generate a DNA fragment, containing the PPARγ-AF2 sequence. The sequences of the primers were as follows 5′>3 5′-ATG ACC ATG GTT GAC ACA GAG ATC G-3′, TA=62°C; 3′>5′ 5′-GTA CAA GTC CTT GTA GAT CGC CTG CAG AGC-3′, TA=62°C. By PCR we generated a 1490 bp fragment, which was run on agarose gels, eluted and ligated into the HpaI-opened pLXIN vector. Correct orientation was verified by restriction analyses followed sequencing.
Retroviral transduction
Retroviral infection of RAW264.7 macrophages was performed essentially as described.34 Briefly, transient transfection of packaging plasmids encoding the vesicular stomatitis virus glycoprotein G35 and the MLV-gag-pol genes36 together with the retroviral vector pLXIN-PPARγ-AF2 was carried out in 293T cells. Target cells were then incubated for 24 h with the infectious supernatant containing 8 μg/ml polybrene. Positive clones (d/n PPARγ) were verified by PPARγ mutant-specific PCR of genomic DNA and reporter assay. PKCα-overexpressing RAW 264.7 macrophages were used as described recently.9
Cell culture
The mouse monocyte/macrophage cell line RAW264.7 and the human T-cell line Jurkat were maintained in RPMI 1640 supplemented with 100 U/ml penicillin, 100 μg/ml streptomycin and 10% heat-inactivated FCS. For induction of apoptosis, a medium without FCS was used. For transwell experiments, we used the Falcon™ Cell culture insert System (BD Labware, Heidelberg, Germany) with a 1.0 μm PET insert.
Generation of apoptotic and necrotic cells
To generate AC an appropriate amount of Jurkat cells was seeded in 10 cm dishes in RPMI 1640 without FCS, supplemented with 100 U/ml penicillin and 100 μg/ml streptomycin. Cells were incubated for 3 h with 0.5 μg/ml staurosporine and afterwards washed twice with medium. Necrotic cells were generated by heating an appropriate number of Jurkat cells at 55°C for 25 min.15 In all experiments, the ratio of apoptotic or necrotic cells to macrophages was kept at a ratio of 5 : 1. For all Western blots, EMSA analysis and flow cytometry experiments, apoptotic Jurkat cells were removed by washing two times with PBS. Cell death was confirmed by flow cytometry, using annexin V-FITC/PI labeling (Immunotech, Marseille, France).
Western blot analysis
PKCα Western blot analysis was carried out as described before9 with the modification of using 60 μg protein. Anti-PKCα was used at a ratio of 1 : 1000 and HRP-labeled goat anti-rabbit secondary antibody was used at a dilution of 1 : 2000.
EMSA
An established EMSA method with minor modifications was used.37 Nuclear protein (20 μg) was incubated for 20 min at room temperature with 2 μg poly(dI-dC) from Pharmacia, 2.5 μl buffer D (20 mM HEPES/KOH, 20% glycerol, 100 mM KCl, 0.5 mM EDTA, 0.25% Nonidet P-40, 2 mM DTT, 0.5 mM PMSF, pH 7.9), 5 μl buffer F (20% Ficoll-400, 100 mM HEPES/KOH, 300 mM KCl, 10 mM DTT, 0.5 mM PMSF, pH 7.9) and 200 fmol 5-DIG-labeled oligonucleotides in a final volume of 25 μl. DNA–protein complexes were resolved at 80 V using a taurine-buffered native 6% polyacrylamide gel, blotted onto positively charged nylon membranes (Nytran Supercharge, Schleicher and Schuell, Dassel, Germany) and crosslinked with 4 J/cm2 on a UV transilluminator. DNA was detected using an alkaline phosphatase-labeled anti-DIG antibody and visualized using the substrate CSPD according to the manufacturer's protocol. Oligonucleotides with the consensus PPRE site highlighted (bold letters) were used38: 5′-GGT AAA GGT CAA AGG TCA AT-3′; 3′-A TTT CCA GTT TCC AGT TAG CCG-5′.
Flow cytometry of oxygen radical production (HE assay)
RAW264.7 cells were seeded in 3 cm plates at a density of 1 × 105 cells/plate 24 h before the experiment. After 1, 3 or 6 h of preincubation with apoptotic Jurkat cells, the medium and AC were removed by washing two times with 1 ml PBS. Macrophages were then suspended in 1 ml PBS and incubated for 30 min with 1 μM PMA. Thereafter, 3 μM HE was added and incubations went on for 30 min. Flow cytometry analysis was performed using a FACSCalibur flow cytometer (BD Biosciences, Heidelberg, Germany) by means of the CellQuestPro software. HE was measured at 630 nm emission (FL3). Gates were set on RAW264.7 macrophages due to their FSC/SSC characteristics. Data from 10 000 cells were collected to reach a statistical significance. Statistical analysis was performed using the appropriate peak median. The shift of the median from untreated cells to PMA-treated cells was set to 100% activation and any inhibition was calculated proportionally.
Statistical analysis
Each experiment was performed at least three times, and statistical analysis was performed using the two-tailed Student's t-test. Otherwise, representative data are shown.
Abbreviations
- AC:
-
apoptotic cells
- ROS:
-
reactive oxygen species
- PPARγ:
-
peroxisome proliferator-activated receptor-γ
- d/n:
-
dominant negative
- PKCα:
-
protein kinase Cα
References
Savill J and Fadok V (2000) Corpse clearance defines the meaning of cell death. Nature 407: 784–788
Freire-de-Lima CG, Nascimento DO, Soares MB, Bozza PT, Castro-Faria-Neto HC, de Mello FG, DosReis GA and Lopes MF (2000) Uptake of apoptotic cells drives the growth of a pathogenic trypanosome in macrophages. Nature 403: 199–203
Voll RE, Herrmann M, Roth EA, Stach C, Kalden JR and Girkontaite I (1997) Immunosuppressive effects of apoptotic cells. Nature 390: 350–351
Lambeth JD (2004) NOX enzymes and the biology of reactive oxygen. Nat. Rev. Immunol. 4: 181–189
Inanami O, Johnson JL, McAdara JK, Benna JE, Faust LR, Newburger PE and Babior BM (1998) Activation of the leukocyte NADPH oxidase by phorbol ester requires the phosphorylation of p47PHOX on serine 303 or 304. J. Biol. Chem. 273: 9539–9543
Bokoch GM and Diebold BA (2002) Current molecular models for NADPH oxidase regulation by Rac GTPase. Blood 100: 2692–2696
Larsen EC, DiGennaro JA, Saito N, Mehta S, Loegering DJ, Mazurkiewicz JE and Lennartz MR (2000) Differential requirement for classic and novel PKC isoforms in respiratory burst and phagocytosis in RAW 264.7 cells. J. Immunol. 165: 2809–2817
Li Q, Subbulakshmi V, Fields AP, Murray NR and Cathcart MK (1999) Protein kinase calpha regulates human monocyte O-2 production and low density lipoprotein lipid oxidation. J. Biol. Chem. 274: 3764–3771
von Knethen A, Tautenhahn A, Link H, Lindemann D and Brune B (2005) Activation-induced depletion of protein kinase C{alpha} provokes desensitization of monocytes/macrophages in sepsis. J. Immunol. 174: 4960–4965
von Knethen A and Brune B (2003) PPARgamma – an important regulator of monocyte/macrophage function. Arch. Immunol. Ther. Exp. (Warsz) 51: 219–226
Zhang X and Young HA (2002) PPAR and immune system – what do we know? Int. Immunopharmacol. 2: 1029–1044
Daynes RA and Jones DC (2002) Emerging roles of PPARs in inflammation and immunity. Nat. Rev. Immunol. 2: 748–759
Chung SW, Kang BY, Kim SH, Pak YK, Cho D, Trinchieri G and Kim TS (2000) Oxidized low density lipoprotein inhibits interleukin-12 production in lipopolysaccharide-activated mouse macrophages via direct interactions between peroxisome proliferator-activated receptor-gamma and nuclear factor-kappa B. J. Biol. Chem. 275: 32681–32687
Holloway AF, Rao S and Shannon MF (2002) Regulation of cytokine gene transcription in the immune system. Mol. Immunol. 38: 567–580
Cvetanovic M and Ucker DS (2004) Innate immune discrimination of apoptotic cells: repression of proinflammatory macrophage transcription is coupled directly to specific recognition. J. Immunol. 172: 880–889
Cocco RE and Ucker DS (2001) Distinct modes of macrophage recognition for apoptotic and necrotic cells are not specified exclusively by phosphatidylserine exposure. Mol. Biol. Cell 12: 919–930
Savill J, Dransfield I, Gregory C and Haslett C (2002) A blast from the past: clearance of apoptotic cells regulates immune responses. Nat. Rev. Immunol. 2: 965–975
Fadok VA, Bratton DL, Konowal A, Freed PW, Westcott JY and Henson PM (1998) Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-beta, PGE2, and PAF. J. Clin. Invest. 101: 890–898
Maasch C, Wagner S, Lindschau C, Alexander G, Buchner K, Gollasch M, Luft FC and Haller H (2000) Protein kinase calpha targeting is regulated by temporal and spatial changes in intracellular free calcium concentration [Ca(2+)](i). FASEB J. 14: 1653–1663
Serinkan BF, Gambelli F, Potapovich AI, Babu H, Giuseppe MD, Ortiz LA, Fabisiak JP and Kagan VE (2005) Apoptotic cells quench reactive oxygen and nitrogen species and modulate TNF-alpha/TGF-beta1 balance in activated macrophages: involvement of phosphatidylserine-dependent and -independent pathways. Cell Death Differ. 8: 1141–1144
Feng J, Han J, Pearce SFA, Silverstein RL, Gotto Jr AM, Hajjar DP and Nicholson AC (2000) Induction of CD36 expression by oxidized LDL and IL-4 by a common signaling pathway dependent on protein kinase C and PPAR-{gamma}. J. Lipid Res. 41: 688–696
Kagan VE, Gleiss B, Tyurina YY, Tyurin VA, Elenstrom-Magnusson C, Liu SX, Serinkan FB, Arroyo A, Chandra J, Orrenius S and Fadeel B (2002) A role for oxidative stress in apoptosis: oxidation and externalization of phosphatidylserine is required for macrophage clearance of cells undergoing Fas-mediated apoptosis. J. Immunol. 169: 487–499
Lauber K, Bohn E, Krober SM, Xiao YJ, Blumenthal SG, Lindemann RK, Marini P, Wiedig C, Zobywalski A, Baksh S, Xu Y, Autenrieth IB, Schulze-Osthoff K, Belka C, Stuhler G and Wesselborg S (2003) Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal. Cell 113: 717–730
Shiraki T, Kamiya N, Shiki S, Kodama TS, Kakizuka A and Jingami H (2005) Alpha,beta-unsaturated ketone is a core moiety of natural ligands for covalent binding to peroxisome proliferator-activated receptor gamma. J. Biol. Chem. 280: 14145–14153
McIntyre TM, Pontsler AV, Silva AR, St Hilaire A, Xu Y, Hinshaw JC, Zimmerman GA, Hama K, Aoki J, Arai H and Prestwich GD (2003) Identification of an intracellular receptor for lysophosphatidic acid (LPA): LPA is a transcellular PPARgamma agonist. Proc. Natl. Acad. Sci. USA 100: 131–136
Martin-Nizard F, Furman C, Delerive P, Kandoussi A, Fruchart JC, Staels B and Duriez P (2002) Peroxisome proliferator-activated receptor activators inhibit oxidized low-density lipoprotein-induced endothelin-1 secretion in endothelial cells. J. Cardiovasc. Pharmacol. 40: 822–831
Wakino S, Kintscher U, Liu Z, Kim S, Yin F, Ohba M, Kuroki T, Schonthal AH, Hsueh WA and Law RE (2001) Peroxisome proliferator-activated receptor gamma ligands inhibit mitogenic induction of p21Cip1 by modulating the protein kinase cdelta pathway in vascular smooth muscle cells. J. Biol. Chem. 276: 47650–47657
Patel H, Truant R, Rachubinski RA and Capone JP (2005) Activity and subcellular compartmentalization of peroxisome proliferator-activated receptor alpha are altered by the centrosome-associated protein CAP350. J. Cell Sci. 118: 175–186
Von Knethen A and Brune B (2002) Activation of peroxisome proliferator-activated receptor gamma by nitric oxide in monocytes/macrophages down-regulates p47phox and attenuates the respiratory burst. J. Immunol. 169: 2619–2626
Ricote M, Li AC, Willson TM, Kelly CJ and Glass CK (1998) The peroxisome proliferator-activated receptor-gamma is a negative regulator of macrophage activation. Nature 391: 79–82
Cernuda-Morollon E, Rodriguez-Pascual F, Klatt P, Lamas S and Perez-Sala D (2002) PPAR agonists amplify iNOS expression while inhibiting NF-{kappa}B: implications for mesangial cell. J. Am. Soc. Nephrol. 13: 2223–2231
Von Knethen A and Brune B (2001) Delayed activation of PPARgamma by LPS and IFN-gamma attenuates the oxidative burst in macrophages. FASEB J. 15: 535–544
Gurnell M, Wentworth JM, Agostini M, Adams M, Collingwood TN, Provenzano C, Browne PO, Rajanayagam O, Burris TP, Schwabe JW, Lazar MA and Chatterjee VK (2000) A dominant-negative peroxisome proliferator-activated receptor gamma (PPARgamma) mutant is a constitutive repressor and inhibits PPARgamma-mediated adipogenesis. J. Biol. Chem. 275: 5754–5759
Lindemann D, Bock M, Schweizer M and Rethwilm A (1997) Efficient pseudotyping of murine leukemia virus particles with chimeric human foamy virus envelope proteins. J. Virol. 71: 4815–4820
Pietschmann T, Heinkelein M, Heldmann M, Zentgraf H, Rethwilm A and Lindemann D (1999) Foamy virus capsids require the cognate envelope protein for particle export. J. Virol. 73: 2613–2621
Soneoka Y, Cannon PM, Ramsdale EE, Griffiths JC, Romano G, Kingsman SM and Kingsman AJ (1995) A transient three-plasmid expression system for the production of high titer retroviral vectors. Nucl. Acids Res. 23: 628–633
Tautenhahn A, Brune B and von Knethen A (2003) Activation-induced PPARgamma expression sensitizes primary human T cells toward apoptosis. J. Leukoc. Biol. 73: 665–672
Schulman IG, Shao G and Heyman RA (1998) Transactivation by retinoid X receptor-peroxisome proliferator-activated receptor gamma (PPARgamma) heterodimers: intermolecular synergy requires only the PPARgamma hormone-dependent activation function. Mol. Cell. Biol. 18: 3483–3494
Acknowledgements
The work was supported by grants from Deutsche Forschungsgemeinschaft (BR999). We thank Sandra Christmann and Nadja Wallner for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by B Zhivotovsky
Rights and permissions
About this article
Cite this article
Johann, A., von Knethen, A., Lindemann, D. et al. Recognition of apoptotic cells by macrophages activates the peroxisome proliferator-activated receptor-γ and attenuates the oxidative burst. Cell Death Differ 13, 1533–1540 (2006). https://doi.org/10.1038/sj.cdd.4401832
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401832
Keywords
This article is cited by
-
SILAC-based quantitative proteomics to investigate the eicosanoid associated inflammatory response in activated macrophages
Journal of Inflammation (2022)
-
Rab17 mediates differential antigen sorting following efferocytosis and phagocytosis
Cell Death & Disease (2016)
-
Innate apoptotic immunity: the calming touch of death
Cell Death & Differentiation (2008)
-
The signaling mechanism of ROS in tumor progression
Cancer and Metastasis Reviews (2007)