Abstract
Caspases are considered to be the key effector proteases of apoptosis. Initiator caspases cleave and activate downstream executioner caspases, which are responsible for the degradation of numerous cellular substrates. We studied the role of caspases in apoptotic cell death of a human melanoma cell line. Surprisingly, the pancaspase inhibitor zVAD-fmk was unable to block cleavage of poly(ADP-ribose) polymerase (PARP) after treatment with etoposide, while it did prevent DEVDase activity. It is highly unlikely that caspase-2, which is a relatively zVAD-fmk-resistant caspase, is mediating etoposide-induced PARP cleavage, as a preferred inhibitor of this caspase could not prevent cleavage. In contrast, caspase activation and PARP degradation were blocked by pretreatment of the cells with the serine protease inhibitor 4-(2-aminoethyl)benzenesulfonyl fluoride (AEBSF). We therefore conclude that a serine protease regulates an alternative initiation mechanism that leads to caspase activation and PARP cleavage. More importantly, while zVAD-fmk could not rescue melanoma cells from etoposide-induced death, the combination with AEBSF resulted in substantial protection. This indicates that this novel pathway fulfills a critical role in the execution of etoposide-induced programmed cell death.
Similar content being viewed by others
Introduction
Apoptosis is crucial for homeostasis and development in various organisms, whereas its inhibition via the accumulation of mutations is considered a prerequisite for the generation of malignant tumors. Apoptosis is executed by specialized proteases, called caspases, which cleave downstream caspases and numerous other cellular substrates.1 Two major pathways of apoptosis initiation have been described: the extrinsic and intrinsic pathways. The extrinsic pathway is used by death receptor ligands, for instance CD95 ligand or tumor necrosis factor α (TNFα), which induce the activity of the initiator caspase-8.2 The intrinsic pathway is crucial for the induction of apoptosis by other types of stress, for example irradiation or chemotherapeutic drugs. These triggers lead to the release of apoptogenic factors, such as mitochondrial cytochrome c, into the cytosol. Released cytochrome c complexes to Apaf-1 and caspase-9, inducing its oligomerization and activation in a so-called ‘apoptosome’.3 Active caspase-9 is capable of activating the executioner caspase-3, which in turn leads to the activation of other downstream caspases and the cleavage of cellular substrates.
However, caspase-9 and Apaf-1 are not essential for downstream caspase activity under all circumstances, because irradiated Apaf-1 or caspase-9 null thymocytes still display residual DEVD and PARP cleavage activity.4 Moreover, cell death itself is only marginally affected in these ‘apoptosome-deficient’ cells, suggesting that an apoptosome-independent caspase activation program exists. Apoptosis in the absence of the apoptosome appears to depend on caspase activity. Caspase-1 and -7 are candidates for directly activated caspases that are upstream of or bypass mitochondria and employ the apoptosome merely to amplify the caspase cascade.4 In addition, caspase-2 is recruited to a large protein complex in which it becomes active, and this process occurs in the absence of Apaf-1 oligomerization as well.5 The role of caspase-2 in cell death upstream or downstream of the mitochondria is, however, greatly disputed.6 This is largely due to the fact that neither the actual activation nor the substrates have been identified.
Melanomas are characterized by early metastasis and extremely poor response to chemo- and radiotherapy. It is remarkable that p53 is rarely mutated in melanoma,7 while p53 mutations occur often in other aggressive and chemoresistant tumors. It has been proposed that the mechanism underlying melanoma resistance is the loss of Apaf-1 expression, as this mutation is commonly found in metastatic melanoma and correlates with resistance to the induction of an apoptotic program.8 Another explanation for melanoma resistance is the deregulation of the protein Survivin, a member of the inhibitor of apoptosis protein (IAP) family. This protein is strongly expressed in malignant melanoma9 and reported to bind to and inhibit effector caspase-3 and -7,10 although the direct effect on caspases has been questioned by other groups.11,12 Two other members of the IAP family, ML-IAP/Livin,13,14 and XIAP (LP, unpublished observations) are expressed at higher levels in melanoma cell lines than in normal melanocytes. Together, these observations suggest that the therapy resistance of melanomas is due to defects in the pathways downstream of or parallel to mitochondrial release.
Previously, we have shown that melanoma cell line IGR39D, which does not express functional p53, can be sensitized to diverse cell death triggers by expression of the c-Myc oncoprotein (LP et al., submitted for publication). Activation of caspase-3, cleavage of PARP, DNA laddering and membrane blebbing indicate that this death occurs through an apoptotic process. In this report, we studied whether the pancaspase inhibitor zVAD-fmk could reverse the apoptotic program in these melanoma cells after triggering with DNA damage inducers or with the death receptor ligand TNFα. Although zVAD-fmk effectively blocked the DEVDase activity after apoptotic treatment of these cells, no effect was observed on the classical caspase substrate PARP. This result suggests that a zVAD-insensitive protease was able to induce the cleavage of PARP. Here, we describe a novel pathway that is induced upon several stress signals. This pathway is initiated by a serine protease that mediates the activation of downstream caspases and PARP cleavage.
Materials and Methods
Cell lines
The melanoma cell lines, neuroblastoma cell line IMR3215 and the rat fibroblast cell line16 Rat-1/c-MycERTM were cultured in DMEM supplemented with glutamine, penicillin/streptomycin and 8% heat-inactivated fetal calf serum at 37°C. Human melanoma cell line IGR39D, its stable c-myc transfectant IGRmyc clone 3 (IGRmyc-3) and 603 are described elsewhere.17 Rat-1/c-MycERTM cells were used in the absence of 4-hydroxytamoxifen.
Irradiation and other treatments
Where indicated, exponentially growing cells were treated with 10 μg/ml etoposide (VP16, Bristol-Myers Squibb, New York, NY, USA) or 50 ng/ml TNFα (Boehringer Ingelheim, Germany) or ionizing radiation for the indicated time periods. Irradiation was performed in 9-cm dishes or six-well plates at room temperature using a 6-MV linear accelerator at a dose rate of 4 Gy/min. Doses were given in a single fraction of 8 Gy. After irradiation, dishes were immediately returned to the incubator. Pretreatment with zVAD-fmk (Bachem, Bubendorf, Switzerland), zVDVAD-fmk (Enzyme Systems Products, Livermore, CA, USA) or AEBSF (Sigma) was performed for 60 min before application of the apoptotic triggers.
Western blotting
Adherent and nonadherent cells were collected together and washed twice with PBS. Whole-cell lysates were prepared by lysis of the cell pellets in cold lysis buffer consisting of 0.2 M triethanolamine, 0.14 M NaCl, 0.5% NP-40, 0.2% sodiumdeoxycholate or in CHAPS lysis buffer,18 with freshly added 1 mM PMSF and 1 mM leupeptin. After clearing the lysate by high-speed centrifugation, protein concentrations were determined by a modified Bradford method.19 Equal amounts of total protein were resolved on SDS-PAGE gels and blotted on Hybond-P (Amersham, Uppsala, Sweden). Ponceau S stainings were performed to verify protein quantities. Membranes were blocked with 5% nonfat dry milk in 20 mM Tris-HCl pH 7.6, 137 mM NaCl and 0.2% Tween-20 (TBS-T) for 1 h. Primary antibody incubations were carried out in 1% milk/TBS-T for 2 h and followed by three washes with TBS-T. Membranes were incubated with appropriate anti-mouse or anti-rabbit IgG horseradish peroxidase conjugates (Amersham) for 1 h, washed three times and developed using ECLplus reagents (Amersham). The antibodies used were rabbit polyclonal antibodies recognizing human PARP (9542, New England Biolabs, Beverly, MA, USA) at 1 : 3000 and cleaved human caspase-3 (9661, New England Biolabs) at 1 : 1000.
Survival analyses
Cell death was determined using propidium iodide (PI) uptake. For these experiments, floating and adherent cells were collected as described above. Cells were incubated for 5 min at room temperature with 1 mg/ml PI in PBS containing 0.5% BSA and 0.1% sodium azide. After this incubation, cells were analyzed for PI positivity on a FACScaliburR (BD-Biosciences, Erembodegem, Belgium). Cell survival was determined with clonogenic survival assays. Cells were treated with etoposide for 3 h in the absence or presence of the inhibitors 10 μM zVAD-fmk and 200 μM AEBSF. Culture medium was refreshed and the cells were incubated for 1 week with or without inhibitors. Cells were washed, fixed and stained with 5% Giemsa stain.
Substrate cleavage assays
For the DEVD and VDVAD cleavage assays, lysates were prepared from pooled adherent and nonadherent cells in CHAPS lysis buffer.18 Caspase activity in these samples was assayed by measuring the release of 7-amino-4-trifluoromethyl-coumarin (AFC) from DEVD- or VDVAD-containing peptides.18,20
The in vitro PARP cleavage assays were performed by incubating 20-ng aliquots of recombinant human PARP (Alexis, Montreal, Canada) in caspase cleavage buffer18 for 1.5 h at 30°C with increasing concentrations of recombinant human caspase-3 or caspase-2 (R&D Systems, Minneapolis, MN, USA) in the presence or absence of 1 μl 10 mM DEVD-AFC or VDVAD-AFC peptide, respectively. The release of AFC in the AFC-containing reactions was measured in a multilabel counter18 and the cleavage of the added PARP in the matching reactions was determined by Western blotting.
Results
Etoposide-induced PARP cleavage in melanoma cells occurs independently of zVAD-fmk-sensitive caspases
We have previously shown that treatment of melanoma cell line IGRmyc-3 with various DNA-damaging triggers, ER stress inducers, heat shock or TNFα leads to the onset of an apoptotic program characterized by activation of caspase-3 and cleavage of its substrate PARP (LP et al., submitted for publication). To establish whether a pancaspase inhibitor could rescue these cells from DNA damage-induced apoptosis, we pretreated the cells with zVAD-fmk and measured PARP cleavage and DEVDase activity. Although all caspases are able to cleave DEVD-afc to some extent, it is the preferred substrate of caspase-3 and -7, which can both cleave PARP.21,22,23 Surprisingly, we observed that etoposide-induced PARP cleavage could not be inhibited with 10 μM zVAD-fmk, as analyzed by Western blotting (Figure 1a). In the untreated cell cultures, there are always some dying cells because of general culture stress, resulting in some cleavage of PARP in the control samples. Cell detachment and membrane blebbing, as visualized by microscopy, confirmed that the cells demonstrated characteristics of an apoptotic process in the presence of zVAD-fmk (Figure 1b). To confirm that the inhibitor was indeed functional under these conditions, we measured DEVDase activity and observed a complete inhibition when the cells were pretreated with 10 μM zVAD-fmk (Figure 1c). Similar data were obtained when these cells were treated with irradiation (data not shown), suggesting that this human melanoma cell line dies by an apoptotic program that is independent of DEVDase activity. Moreover, PARP cleavage occurs at least to a large extent by a zVAD-fmk-insensitive protease under these conditions.
The pancaspase inhibitor zVAD-fmk blocks DEVDase activity, but cannot block DNA damage-induced apoptosis. (a) IGRmyc-3 cells were treated with etoposide in the absence or presence of 10 μM zVAD-fmk. Whole-cell lysates were prepared at the indicated time points and PARP cleavage was determined on Western blot using a rabbit polyclonal antibody. (b) IGRmyc-3 cells were photographed under a phase-contrast microscope at × 200 magnification after treatment for 24 h with etoposide and/or 10 μM zVAD-fmk or left untreated as indicated. (c) DEVDase activity was measured in DEVD-AFC cleavage assays using 10 μg of protein from lysates of IGRmyc-3 at the indicated time points after treatment with etoposide in the absence or presence of 10 μM zVAD-fmk. The figure is representative of three independent experiments
Caspase-2 is not responsible for the cleavage of PARP
Caspase-2 has been reported to be fairly insensitive to zVAD-fmk.24 Since caspase-2 is suggested to cleave PARP25 and can act as an initiator caspase,26 we analyzed whether caspase-2 is responsible for PARP cleavage in this melanoma cell line using several strategies. First, we determined the ability of recombinant active caspase-2 to cleave recombinant PARP by in vitro incubation. As expected, control incubations of PARP with active recombinant caspase-3 resulted in effective processing of PARP even at low concentrations of the enzyme. However, to our surprise, caspase-2 was unable to cleave PARP in vitro under the same conditions, while at the same time processing of the VDVAD substrate under the same conditions was clearly observed (Figure 2a). This experiment indicates that recombinant caspase-2 is not a PARPase in vitro, yet does not exclude a role for caspase-2 in etoposide-induced PARP cleavage in vivo. To analyze the involvement of caspase-2 further, we blocked caspase-2 activity in vivo by using the inhibitor zVDVAD-fmk which is able to inhibit caspase-2, -3 and -7 with similar efficiencies.23 Consistent with the data in Figure 2a, pretreatment of the cells with increasing concentrations, up to 50 μM, of zVDVAD-fmk did not reduce etoposide-induced PARP cleavage (Figure 2b, upper panel). The VDVADase activity, which might represent activation of caspase-2 as well as caspase-3 and -7, in these cells was significantly inhibited, even at the lowest concentration of zVDVAD-fmk (Figure 2b, lower panel). Moreover, pretreatment of the cells with 10 μM zVAD-fmk, the pancaspase inhibitor that was unable to prevent PARP cleavage, resulted in a complete block of the VDVADase activity (Figure 2c). This suggests that either caspase-2 is sensitive to this concentration of zVAD-fmk or that the VDVADase activity measured in these cells reflects the activity of other caspases. These experiments thus make it very unlikely that caspase-2 plays a role in PARP cleavage in this cell line.
Caspase-2 is not responsible for the PARP cleavage observed during etoposide-induced apoptosis. (a) 20-ng aliquots of recombinant human PARP were incubated in caspase cleavage buffer with increasing concentrations of active recombinant human caspase-3 or -2 as indicated. Cleavage of PARP was determined on Western blot. In matching reactions, the caspase-3 and -2 activity was measured using DEVD-AFC or VDVAD-AFC, respectively. (b) IGRmyc-3 cells were left untreated (−) or treated (+) with etoposide for 24 h in the absence or presence of 10 μM zVAD-fmk or of the indicated concentrations of zVDVAD-fmk (μM). CHAPS cell lysates were prepared and PARP cleavage was determined by Western blotting. VDVDADase activity in the same lysates was determined using the AFC-labelled substrate. (c) VDVADase activity was measured in VDVAD cleavage assays of lysates prepared from IGRmyc-3 cells after treatment with etoposide for the indicated time periods in the absence or presence of 10 μM zVAD-fmk. The figure is representative for three independent experiments
A serine protease inhibitor abolishes DNA damage-induced apoptosis
As etoposide-induced PARP cleavage in the human melanoma cell line IGRmyc-3 appears caspase-independent, we hypothesized that a distinct protease is responsible for the cleavage of cellular substrates. Therefore, these cells were pretreated with the potent serine protease inhibitor 4-(2-aminoethyl)benzenesulfonyl fluoride (AEBSF), which acts by sulfonylation of the serine residue at the active site.27 We monitored the appearance of the cleaved PARP fragment on Western blots. In contrast to zVAD-fmk, pretreatment with AEBSF prevented etoposide-induced cleavage of PARP (Figure 3a, upper panel), suggesting that a serine protease is involved in the cascade that leads to PARP processing. Importantly, the observed etoposide-induced PARP cleavage is not due to postlysis effects, but occurs in intact cells as cell lysates prepared by immediate boiling in SDS buffer display identical levels of PARP cleavage (data not shown).
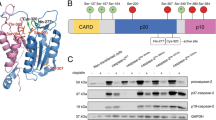
Serine protease inhibitor AEBSF blocks DNA damage-induced apoptosis, but not TNFα-triggered apoptosis. (a) Western blot of whole-cell lysates of IGRmyc-3 cells, harvested at the indicated time points after addition of etoposide. Cells were treated in the absence or presence of 10 μM zVAD-fmk or 400 μM AEBSF. The upper part was incubated with an antibody recognizing full-length and cleaved PARP and the lower part with an antibody specific for cleaved caspase-3. The p20 and p17 subunits are marked. (b) IGRmyc-3 cells were irradiated with 8 Gy or treated with TNFα as indicated. Full-length PARP (◂) and cleaved PARP (◃) were determined by Western blotting. (c) DEVDase activity was determined using the substrate DEVD-AFC. The left part is representative for three independent experiments of treatment of IGRmyc-3 cells with etoposide for the indicated time periods with or without pretreatment of 400 μM AEBSF. The right part represents IGRmyc-3 cells treated with TNFα for 16 h either without pretreatment, or pretreated with 10 μM zVAD–fmk or 400 μM AEBSF. The graph is representative for at least two independent experiments. (d) IGRmyc-3 cells were left untreated or treated with etoposide in the presence or absence of increasing concentrations of AEBSF (μM) and/or 10 μM zVAD-fmk for 24 or 32 h, as indicated. The percentage of cells that failed to exclude PI was determined by FACS analysis. The percentages of PI-positive untreated cells were 17 and 14% at 24 and 32 h, respectively. The background percentages of PI-positive cells cultured in the absence of etoposide were subtracted from the corresponding etoposide-treated samples. (e) IGRmyc cells were treated with etoposide in the absence or presence of the indicated inhibitors. After 3 h, the medium and inhibitors were refreshed and cells were incubated for 1 week. Cells were visualized by staining with Giemsa solution. The left panel shows photographs of the cells, cultured in six-well plates. The right panel shows microscopic pictures of the same cell cultures at × 50 magnification
Activation of caspase-3 is achieved through a two-step process. The first cleavage results in p12 and p20 subunits, while the second step is a further processing of this p20 subunit to the p17 subunit.28 The latter cleavage, known to be mediated by caspase-3 itself, is blocked when the melanoma cells are pretreated with zVAD-fmk (Figure 3a, lower panel). This result underscores the observation that zVAD-fmk prevented caspase activity, because it blocked autoprocessing to the p17 subunit in our system (Figure 1c). Nevertheless, we did observe the appearance of the p20 subunit indicating that the initial cleavage of caspase-3 occurred in the presence of a pancaspase inhibitor in these cells (Figure 3a). Interestingly, the serine protease inhibitor AEBSF also blocked this initial caspase-3 processing (Figure 3a) and DEVDase activity (Figure 3c, left), and thus seems to act upstream of caspase-3 activation.
To determine whether the protective effect of AEBSF was restricted to etoposide-induced apoptosis, we treated these cells with irradiation. Irradiation-induced PARP cleavage in these melanoma cells could be prevented by AEBSF (Figure 3b, upper panel). Cleavage of PARP triggered by the ER stress inducer Brefeldin A could also be partially blocked (data not shown), suggesting that the involvement of a serine protease in the apoptotic process is not limited to DNA damage-induced apoptosis. On the other hand, cleavage of PARP and caspase-3 caused by the death receptor ligand TNFα could not be inhibited by AEBSF (Figure 3b, lower panel). In agreement with this finding, DEVDase activity induced by TNFα was insensitive to AEBSF (Figure 3c, right). This result confirmed the observation that AEBSF is not a general inhibitor of caspases.29,30 In agreement, when added directly to the lysates or to recombinant caspase-3, AEBSF was not able to inhibit the DEVDase activity in vitro, in contrast to zVAD-fmk (data not shown). These results indicate that the DEVDase activity in these cells is inhibited indirectly by AEBSF and suggests that AEBSF acts upstream of caspase-3.
Inhibition of serine protease and caspase activity rescues etoposide-treated cells
Activation of caspases and cleavage of several caspase substrates are intrinsic to the execution of apoptosis. However, inhibition of these events using caspase inhibitors does not always lead to the protection from death.31,32,33,34 Also here we find that etoposide-induced blebbing of the melanoma cell was hardly affected by addition of zVAD-fmk. The observation that a serine protease acts upstream of caspase activation may explain this phenotype as this protease activity may circumvent the need for caspase activity and still effectively induce cell death. To analyze the effects on cell death in more detail, we therefore set out to determine the membrane integrity of the melanoma cells upon treatment with etoposide. We measured the capacity of the treated cells to exclude PI. Etoposide induced clear loss of membrane integrity already after 16 h (data not shown) and this loss increased over time. At 24 h, PI uptake amounted to 33% over background and to 46% at 32 h. Importantly, zVAD-fmk pretreatment had the capacity to initially prevent this cell death to some extent, but this effect was lost at later time points, suggesting that the inhibition of caspase activity by zVAD-fmk is not sufficient to prevent cell death. We also analyzed the effect of AEBSF pretreatment on cell survival. Unfortunately, this analysis was hampered by the fact that AEBSF itself showed some toxicity, especially at higher concentrations (10–20% cell death). We therefore decided to use declining concentrations of AEBSF to circumvent this side effect. Treatment of cell with 100 μM AEBSF resulted only in marginal toxic effects (5–10% cell death). Nevertheless, this concentration of AEBSF already significantly protected the cells from etoposide-induced death (Figure 3D). This effect increased steadily with increasing concentrations of AEBSF. More importantly, zVAD-fmk together with AEBSF clearly displayed an additive effect. The combination of zVAD-fmk with 100 μM AEBSF almost completely blocked PI uptake, which was back to background levels when zVAD-fmk was used together with 200 μM AEBSF, even at 32 h (Figure 3d).
These data thus suggest that AEBSF in concert with zVAD-fmk can induce survival. In order to determine whether etoposide-treated cells would indeed survive for longer periods of time, we performed clonogenic survival assays. Cells were treated with etoposide in the absence or presence of the inhibitors. After 1 week of incubation, hardly any cells were observed in the etoposide-treated sample, indicating that almost all had succumbed to the toxic effects of etoposide (Figure 3e). The addition of 10 μM zVAD-fmk could not permanently rescue the cells. Even though after shorter periods 200 μM AEBSF could protect the cells against etoposide (Figure 3d), at later time points this protection was no longer observed. This suggests that the toxic effect of AEBSF prohibits the long-term survival. However, incubation of the cells in the presence of both inhibitors resulted in the appearance of many small colonies, suggesting that these cells do not only survive but also regain their proliferative capacity. Of course, the amount of cells seen in the wells is far less as in the untreated samples as the latter ones have not experienced the DNA-damaging effects of etoposide and thus did not need to repair the damage before cycling (Figure 3e, left panel). Moreover, an effect of AEBSF on the cell cycle has been reported as well (Stefanis et al.40 and data not shown). Nevertheless, as small colonies are observed, the long-term effect of the combined inhibitors clearly permits continuing proliferation of the cells (Figure 3e).
(continued) Serine protease inhibitor AEBSF blocks DNA damage-induced apoptosis, but not TNFα-triggered apoptosis. (a) Western blot of whole-cell lysates of IGRmyc-3 cells, harvested at the indicated time points after addition of etoposide. Cells were treated in the absence or presence of 10 μM zVAD-fmk or 400 μM AEBSF. The upper part was incubated with an antibody recognizing full-length and cleaved PARP and the lower part with an antibody specific for cleaved caspase-3. The p20 and p17 subunits are marked. (b) IGRmyc-3 cells were irradiated with 8 Gy or treated with TNFα as indicated. Full-length PARP (◂) and cleaved PARP (◃) were determined by Western blotting. (c) DEVDase activity was determined using the substrate DEVD-AFC. The left part is representative for three independent experiments of treatment of IGRmyc-3 cells with etoposide for the indicated time periods with or without pretreatment of 400 μM AEBSF. The right part represents IGRmyc-3 cells treated with TNFα for 16 h either without pretreatment, or pretreated with 10 μM zVAD–fmk or 400 μM AEBSF. The graph is representative for at least two independent experiments. (d) IGRmyc-3 cells were left untreated or treated with etoposide in the presence or absence of increasing concentrations of AEBSF (μM) and/or 10 μM zVAD-fmk for 24 or 32 h, as indicated. The percentage of cells that failed to exclude PI was determined by FACS analysis. The percentages of PI-positive untreated cells were 17 and 14% at 24 and 32 h, respectively. The background percentages of PI-positive cells cultured in the absence of etoposide were subtracted from the corresponding etoposide-treated samples. (e) IGRmyc cells were treated with etoposide in the absence or presence of the indicated inhibitors. After 3 h, the medium and inhibitors were refreshed and cells were incubated for 1 week. Cells were visualized by staining with Giemsa solution. The left panel shows photographs of the cells, cultured in six-well plates. The right panel shows microscopic pictures of the same cell cultures at × 50 magnification
These results indicate that inhibition of the serine protease activity in combination with inhibition of caspases is sufficient to extend survival of these melanoma cells for longer time periods after treatment with the potent cytotoxic drug etoposide.
AEBSF prevents apoptosis in several cell types
To establish whether etoposide-induced PARP cleavage in other melanoma cell lines can be abolished by pretreatment with AEBSF, we analyzed the cleavage of PARP in IGR39D, the parental cell line of IGRmyc-3, and in melanoma cell line 603, which also shows some sensitivity to etoposide (Figure 4a). The protective effect of AEBSF was not restricted to IGRmyc-3, as this inhibitor could prevent PARP cleavage in the parental cell line IGR39D as well. However, it is clear that the effect of AEBSF was not found in all cell lines, as AEBSF failed to inhibit PARP cleavage in the less susceptible melanoma cell line 603. Importantly, we also found that etoposide-induced PARP cleavage in the human neuroblastoma cell line IMR32 could be blocked by AEBSF (Figure 4a), indicating that the protective effect of AEBSF is not limited to melanoma cells.
AEBSF inhibits apoptosis in several cell types. (a) The human melanoma cell lines IGR39D and 603 and the neuroblastoma cell line IMR32 were left untreated or treated with etoposide for 16 h in the absence or presence of 400 μM AEBSF. Whole-cell lysates were analyzed on Western blot. Full-length PARP (◂) and cleaved PARP (◃) are marked. (b) Rat fibroblast-derived cells were treated with etoposide with or without pretreatment with 400 μM AEBSF and lysed in CHAPS buffer at the indicated time points. Cleavage of PARP was determined by Western blotting. DEVDase activity in the same rat fibroblast lysates was determined using the substrate DEVD-AFC
In addition, we determined whether substrate cleavage and caspase activation in a rat fibroblast-derived cell line could be blocked by pretreatment with AEBSF. Analysis of etoposide-treated rat fibroblasts demonstrated that PARP cleavage as well as DEVDase activity were completely blocked by this serine protease inhibitor (Figure 4b). Together, these data indicate that a serine protease plays an important role in DNA damage-induced apoptosis in various cell types.
Discussion
Caspase-independent initiation of apoptosis
In this study, we characterized certain proteolytic events that are responsible for apoptotic cell death induced by DNA damage in human melanoma cells. In IGRmyc-3 cells, caspase-3 is processed and activated during apoptosis. As expected, DEVDase activity was abolished by pretreatment with the pancaspase inhibitor zVAD-fmk. Nevertheless, these zVAD-fmk-treated cells still demonstrated membrane blebbing, which has been reported previously.31 Intriguingly, we found that in the absence of DEVDase activity, PARP was still cleaved into a fragment of approximately 85 kDa, a phenomenon that to our knowledge has never been reported before. Only in the case of necrosis in Jurkat cells, PARP is processed in the presence of zVAD-fmk, but this processing results in other fragments than we observed in this study.35 Therefore, the question is raised as to which protease was responsible for the observed PARP cleavage.
It has been reported that in COS cells overexpression of caspase-2, which is proposed to be relatively zVAD fmk-insensitive,24 leads to cleavage of PARP.25 Recent studies demonstrate caspase-2 as an initiator caspase upstream of the mitochondria.26,36,37 However, we provide evidence that indicates that caspase-2 is not responsible for initiating the apoptotic program in IGRmyc-3 cells. Whereas VDVADase activity, reflecting the activity of caspase-2, -3 and -7, was blocked by pretreatment with zVDVAD-fmk,23 this inhibitor did not affect the etoposide-induced cleavage of PARP. Furthermore, we demonstrated that zVAD-fmk was able to block the zVDVADase activity, suggesting that caspase-2 is either sensitive to the concentration of zVAD-fmk we used or that the zVDVADase activity in these cells does not reflect the activity of caspase-2, but the activity of caspase-3 or -7. Therefore, we exclude a role for caspase-2 in PARP cleavage in etoposide-treated IGRmyc-3 cells. Our observations are in agreement with O'Reilly et al.,38 who concluded that caspase-2 is not essential for apoptosis in all cell types, because thymocytes and neuronal cells derived from caspase-2-deficient mice die normally in response to a broad range of apoptotic stimuli. Despite these data, a definite exclusive answer on the role of caspase-2 cannot be given as both the mode of activation and the identity of physiological active caspase-2 are unknown. Like other initiator caspases, caspase-2 may be activated by induced proximity. Whether such a caspase-2 apoptosome displays different substrate specificity compared to cleaved caspase-2 product will need to be determined and an effect of AEBSF on this activity is at this point pure speculation but cannot be formally excluded.
Another initiator caspase, caspase-9, is also very unlikely to be the PARPase in our system, as the etoposide-induced LEHDase activity is completely blocked by zVAD-fmk pretreatment (data not shown). We therefore suggest that the apoptotic pathway in IGRmyc-3 can be initiated independently of caspase activity.
Involvement of a serine protease in apoptotic cell death
There are several indications that the mitochondrial pathway is not functional in IGRmyc-3 cells. It has been proposed that melanoma cells often exhibit downregulated Apaf-1 expression, leading to a defect in the apoptotic pathway downstream of the mitochondria and resistance of the cells to apoptosis-inducing triggers.8 Although the Apaf-1 expression in IGRmyc-3 is not downregulated as compared to melanocytes, the expression of caspase-9 is relatively low and there is abundant expression of XIAP (unpublished observations). In line with these observations, we were unable to substantiate a role for cytochrome c release and the activity of the apoptosome during DNA damage-induced apoptosis in IGRmyc-3 melanoma cells (unpublished observations), suggesting that the mitochondrial pathway is not involved in these cells. Interestingly, Marsden et al.4 recently demonstrated that apoptosis is only slightly delayed in Apaf-1- and caspase-9-deficient cells and conclude that in these cells, the apoptosome is not essential for apoptosis. The lack of involvement of the apoptosome pathway in the initiation of DNA damage-induced apoptosis in IGRmyc-3 cells leads us to hypothesize that, in these cells, apoptosis is mediated by an alternative pathway. This study supports this hypothesis, demonstrating that pretreatment with the serine protease inhibitor AEBSF affected the first cleavage step of caspase-3 activation and the cleavage of PARP induced by DNA-damaging agents. Moreover, in combination with zVAD-fmk, AEBSF rescued these cells from etoposide-induced death and even allowed clonogenicity.
Based on the observation that AEBSF could not rescue IGRmyc-3 from TNFα-induced apoptosis, we conclude that the serine protease is not essential for at least this, and possibly other forms of, death receptor-triggered apoptosis. AEBSF is therefore not a general inhibitor of caspases or of apoptotic manifestations. This result is in agreement with previous observations that AEBSF can inhibit Bin-1-mediated apoptosis, but fails to block apoptosis induced by Fas activation, granzyme B,29 or staurosporin.30 In contrast, TNFα-induced apoptosis of human gastric adenocarcinoma cells is inhibited by AEBSF,39 suggesting that the effect of AEBSF is cell line dependent.
Importantly, the activation of apoptosis by an AEBSF-sensitive serine protease is not restricted to IGRmyc-3, a melanoma line that is sensitized by c-Myc. Similar observations were made in the parental, nontransfected cell line IGR39D. Moreover, the neuroblastoma cell line IMR32 and a rat fibroblast line were also shown to be protected from etoposide-induced PARP cleavage and DEVDase activity by AEBSF. Nevertheless, AEBSF-induced protection is cell line dependent, as another melanoma line failed to show inhibition of their apoptotic program. Clarification of the cell type specificity of this inhibition could yield crucial insight into the mechanism of serine protease-induced apoptosis.
The suppression of cell death by AEBSF has been described in earlier publications, in which the AEBSF-sensitive serine protease is placed upstream of caspase activity.29,39,40,41,42 The inhibition of apoptotic features29,39 and the cleavage of PARP by PC12 lysates40 is suggested to be the result of blocking caspases by AEBSF or via inhibition of the function of p53.42 We, however, demonstrated that PARP is cleaved in the absence of DEVDase activity and functional p53. AEBSF is able to block both the DEVDase activity and the cleavage of PARP. We therefore suggest that AEBSF blocks a serine protease that functions upstream of caspases and can also bypass the zVAD-sensitive caspases in the cleavage of PARP. More importantly, we show that this pathway is highly relevant for melanoma cell death induced by several treatments as its incidence kills cells effectively independently of caspases, while its absence allows the cells to survive. As such, a better understanding of this protease may provide new effective ways to treat tumors.
Alternative death pathways
Several protease activities, other than caspases, have been implicated during apoptosis in different systems. For example, cathepsins and calpains, which are cysteine proteases (reviewed by Leist and Jaattela43), and the serine proteases Granzyme B and HtrA2/Omi have been shown to modulate or even initiate an apoptotic cascade. In some cell types, release of cathepsin B from the lysosomal compartment is critically important for TNFα-induced apoptosis.44,45 Once released, cathepsin B activates the caspase machinery, followed by the induction of cell death. Importantly, this pathway can be inhibited effectively using CA-074Me,46 a highly specific cathepsin B inhibitor. This observation prompted us to determine whether cathepsin B was the protease involved in our melanoma system. However, CA-074Me failed to reduce etoposide-induced PARP cleavage in our cells (unpublished observations), suggesting that another protease mediates this cleavage.
Granzyme B, which can induce cell death via cleavage of Bid and caspase-3, -7 and -8,47,48,49,50 is not expressed by these cells. Waterhouse et al.51 previously described a role for calpain in irradiation-induced apoptosis and suggested that activation of this protease leads to cleavage of fodrin as well as caspases. We attempted to analyze the effect of the conventional calpain inhibitor I52 in our system, but the inhibitor had severe toxic side effects on the melanoma cells (data not shown). This result clearly indicates an important role for calpains in survival, but on the other hand does not exclude a role for calpain activity in apoptosis.
The serine protease HtrA2 is released from the mitochondria during apoptosis and sequesters XIAP, thereby allowing caspase activation to occur. Besides its XIAP-binding activity, HtrA2 contains a serine protease activity that by itself can induce cell death.53,54,55,56 Although these findings would propose HtrA2 as a candidate apoptogenic molecule, transfection experiments with full-length as well as processed HtrA2 in IGRmyc-3 indicated that overexpression of this protease did not induce nor accelerate cell death in these melanoma cells (unpublished observations). Taken together, these data point to the presence of yet another serine protease activity, inhibition of which rescues from apoptotic cell death, but formal proof for this idea will be provided by the identification of the protease involved. We are currently pursuing this question.
In conclusion, our data demonstrate that an AEBSF-sensitive protease is central to the initiation of apoptosis in several cell types. This protease might be placed on top of the caspase activation cascade and regulates the cleavage of PARP independently of caspases. Although the exact mechanism by which this protease mediates cell death remains to be determined, our data provide convincing evidence for an alternative pathway by which cells can undergo apoptosis.
Abbreviations
- AEBSF:
-
4-(2-aminoethyl)benzenesulfonyl fluoride
- AFC:
-
7-amino-4-trifluoromethyl-coumarin
- CHAPS:
-
3-[(3-cholamidopropyl)dimethylammonio]-1-propanesulfonate
- etop:
-
etoposide, VP16
- PARP:
-
poly(ADP-ribose) polymerase-1
- PBS:
-
phosphate-buffered saline
- PI:
-
propidium iodide
- PMSF:
-
phenylmethylsulfonyl fluoride
- SDS:
-
sodium dodecylsulfate
- TNFα:
-
tumor necrosis factor α
- zVAD-fmk:
-
benzyloxy-carbonyl-Val-Ala-Asp-fluoromethyl ketone
- zVDVAD-fmk:
-
benzyloxycarbonyl-Val-Asp-Val-Ala-Asp-fluoromethyl ketone
References
Thornberry NA and Lazebnik Y (1998) Caspases: enemies within. Science 281: 1312–1316
Ashkenazi A and Dixit VM (1998) Death receptors: signaling and modulation. Science 281: 1305–1308
Cain K, Bratton SB, Langlais C, Walker G, Brown DG, Sun XM and Cohen GM (2000) Apaf-1 oligomerizes into biologically active approximately 700-kDa and inactive approximately 1.4-MDa apoptosome complexes. J. Biol. Chem. 275: 6067–6070
Marsden VS, O'Connor L, O'Reilly LA, Silke J, Metcalf D, Ekert PG, Huang DC, Cecconi F, Kuida K, Tomaselli KJ, Roy S, Nicholson DW, Vaux DL, Bouillet P, Adams JM and Strasser A (2002) Apoptosis initiated by Bcl-2-regulated caspase activation independently of the cytochrome c/Apaf-1/caspase-9 apoptosome. Nature 419: 634–637
Read SH, Baliga BC, Ekert PG, Vaux DL and Kumar S (2002) A novel Apaf-1-independent putative caspase-2 activation complex. J. Cell. Biol. 159: 739–745
Troy CM and Shelanski ML (2003) Caspase-2 redux. Cell Death. Differ. 10: 101–107
Zerp SF, Van Elsas A, Peltenburg LTC and Schrier PI (1999) p53 mutations in human cutaneous melanoma correlate with sun exposure but are not always involved in melanomagenesis. Br. J. Cancer 79: 921–926
Soengas MS, Capodieci P, Polsky D, Mora J, Esteller M, Opitz-Araya X, McCombie R, Herman JG, Gerald WL, Lazebnik YA, Cordon-Cardo C and Lowe SW (2001) Inactivation of the apoptosis effector Apaf-1 in malignant melanoma. Nature 409: 207–211
Grossman D, McNiff JM, Li F and Altieri DC (1999) Expression and targeting of the apoptosis inhibitor, survivin, in human melanoma. J. Invest. Dermatol. 113: 1076–1081
Tamm I, Wang Y, Sausville E, Scudiero DA, Vigna N, Oltersdorf T and Reed JC (1998) IAP-family protein survivin inhibits caspase activity and apoptosis induced by Fas (CD95), Bax, caspases, and anticancer drugs. Cancer Res. 58: 5315–5320
Banks DP, Plescia J, Altieri DC, Chen J, Rosenberg SH, Zhang H and Ng SC (2000) Survivin does not inhibit caspase-3 activity. Blood 96: 4002–4003
Verdecia MA, Huang H, Dutil E, Kaiser DA, Hunter T and Noel JP (2000) Structure of the human anti-apoptotic protein survivin reveals a dimeric arrangement. Nat. Struct. Biol. 7: 602–608
Vucic D, Stennicke HR, Pisabarro MT, Salvesen GS and Dixit VM (2000) ML-IAP, a novel inhibitor of apoptosis that is preferentially expressed in human melanomas. Curr. Biol. 10: 1359–1366
Kasof GM and Gomes BC (2001) Livin, a novel inhibitor of apoptosis protein family member. J. Biol. Chem. 276: 3238–3246
Tumilowicz JJ, Nichols WW, Cholon JJ and Greene AE (1970) Definition of a continuous human cell line derived from neuroblastoma. Cancer Res. 30: 2110–2118
Littlewood TD, Hancock DC, Danielian PS, Parker MG and Evan GI (1995) A modified oestrogen receptor ligand-binding domain as an improved switch for the regulation of heterologous proteins. Nucleic Acids Res. 23: 1686–1690
Versteeg R, Noordermeer IA, Krüse-Wolters KM, Ruiter DJ and Schrier PI (1988) c-Myc downregulates class I HLA expression in human melanomas. EMBO J. 7: 1023–1029
Kashkar H, Krönke M and Jürgensmeier JM (2002) Defective Bax activation in Hodgkin B-cell lines confers resistance to staurosporine-induced apoptosis. Cell Death Differ. 9: 750–757
Sedmak JJ and Grossberg SE (1977) A rapid, sensitive, and versatile assay for protein using Coomassie brilliant blue G250. Anal. Biochem. 79: 544–552
Stennicke HR and Salvesen GS (1997) Biochemical characteristics of caspases-3, -6, -7, and -8. J. Biol. Chem. 272: 25719–25723
Rotonda J, Nicholson DW, Fazil KM, Gallant M, Gareau Y, Labelle M, Peterson EP, Rasper DM, Ruel R, Vaillancourt JP, Thornberry NA and Becker JW (1996) The three-dimensional structure of apopain/CPP32, a key mediator of apoptosis. Nat. Struct. Biol. 3: 619–625
Nicholson DW, Ali A, Thornberry NA, Vaillancourt JP, Ding CK, Gallant M, Gareau Y, Griffin PR, Labelle M and Lazebnik YA (1995) Identification and inhibition of the ICE/CED-3 protease necessary for mammalian apoptosis. Nature 376: 37–43
Talanian RV, Quinlan C, Trautz S, Hackett MC, Mankovich JA, Banach D, Ghayur T, Brady KD and Wong WW (1997) Substrate specificities of caspase family proteases. J. Biol. Chem. 272: 9677–9682
Garcia-Calvo M, Peterson EP, Leiting B, Ruel R, Nicholson DW and Thornberry NA (1998) Inhibition of human caspases by peptide-based and macromolecular inhibitors. J. Biol. Chem. 273: 32608–32613
Gu Y, Sarnecki C, Aldape RA, Livingston DJ and Su MS (1995) Cleavage of poly(ADP-ribose) polymerase by interleukin-1 beta converting enzyme and its homologs TX and Nedd-2. J. Biol. Chem. 270: 18715–18718
Lassus P, Opitz-Araya X and Lazebnik Y (2002) Requirement for caspase-2 in stress-induced apoptosis before mitochondrial permeabilization. Science 297: 1352–1354
Markwardt F, Drawert J and Walsmann P (1974) Synthetic low molecular weight inhibitors of serum kallikrein. Biochem. Pharmacol. 23: 2247–2256
Han Z, Hendrickson EA, Bremner TA and Wyche JH (1997) A sequential two-step mechanism for the production of the mature p17:p12 form of caspase-3 in vitro. J. Biol. Chem. 272: 13432–13436
Kagaya S, Kitanaka C, Noguchi K, Mochizuki T, Sugiyama A, Asai A, Yasuhara N, Eguchi Y, Tsujimoto Y and Kuchino Y (1997) A functional role for death proteases in s-Myc- and c-Myc-mediated apoptosis. Mol. Cell. Biol. 17: 6736–6745
Elliott K, Ge K, Du W and Prendergast GC (2000) The c-Myc-interacting adaptor protein Bin1 activates a caspase-independent cell death program. Oncogene 19: 4669–4684
McCarthy NJ, Whyte MK, Gilbert CS and Evan GI (1997) Inhibition of Ced-3/ICE-related proteases does not prevent cell death induced by oncogenes, DNA damage, or the Bcl-2 homologue Bak. J. Cell. Biol. 136: 215–227
Brunet CL, Gunby RH, Benson RS, Hickman JA, Watson AJ and Brady G (1998) Commitment to cell death measured by loss of clonogenicity is separable from the appearance of apoptotic markers. Cell Death Differ. 5: 107–115
Davidson FF and Steller H (1998) Blocking apoptosis prevents blindness in Drosophila retinal degeneration mutants. Nature 391: 587–591
Johnson MD, Xiang H, London S, Kinoshita Y, Knudson M, Mayberg M, Korsmeyer SJ and Morrison RS (1998) Evidence for involvement of Bax and p53, but not caspases, in radiation-induced cell death of cultured postnatal hippocampal neurons. J. Neurosci. Res. 54: 721–733
Gobeil S, Boucher CC, Nadeau D and Poirier GG (2001) Characterization of the necrotic cleavage of poly(ADP-ribose) polymerase (PARP-1): implication of lysosomal proteases. Cell Death Differ. 8: 588–594
Robertson JD, Enoksson M, Suomela M, Zhivotovsky B and Orrenius S (2002) Caspase-2 acts upstream of mitochondria to promote cytochrome c release during etoposide-induced apoptosis. J. Biol. Chem. 277: 29803–29809
Guo Y, Srinivasula SM, Druilhe A, Fernandes-Alnemri T and Alnemri ES (2002) Caspase-2 induces apoptosis by releasing proapoptotic proteins from mitochondria. J. Biol. Chem. 277: 13430–13437
O'Reilly LA, Ekert P, Harvey N, Marsden V, Cullen L, Vaux DL, Hacker G, Magnusson C, Pakusch M, Cecconi F, Kuida K, Strasser A, Huang DC and Kumar S (2002) Caspase-2 is not required for thymocyte or neuronal apoptosis even though cleavage of caspase-2 is dependent on both Apaf-1 and caspase-9. Cell Death Differ. 9: 832–841
Park IC, Park MJ, Choe TB, Jang JJ, Hong SI and Lee SH (2000) TNF-alpha induces apoptosis mediated by AEBSF-sensitive serine protease(s) that may involve upstream caspase-3/CPP32 protease activation in a human gastric cancer cell line. Int. J. Oncol. 16: 1243–1248
Stefanis L, Troy CM, Qi H and Greene LA (1997) Inhibitors of trypsin-like serine proteases inhibit processing of the caspase Nedd-2 and protect PC12 cells and sympathetic neurons from death evoked by withdrawal of trophic support. J. Neurochem. 69: 1425–1437
Dong Z, Saikumar P, Patel Y, Weinberg JM and Venkatachalam MA (2000) Serine protease inhibitors suppress cytochrome c-mediated caspase-9 activation and apoptosis during hypoxia-reoxygenation. Biochem. J. 347 (Part 3): 669–677
Rideout HJ, Zang E, Yeasmin M, Gordon R, Jabado O, Park DS and Stefanis L (2001) Inhibitors of trypsin-like serine proteases prevent DNA damage-induced neuronal death by acting upstream of the mitochondrial checkpoint and of p53 induction. Neuroscience 107: 339–352
Leist M and Jaattela M (2001) Four deaths and a funeral: from caspases to alternative mechanisms. Nat. Rev. Mol. Cell Biol. 2: 589–598
Foghsgaard L, Wissing D, Mauch D, Lademann U, Bastholm L, Boes M, Elling F, Leist M and Jaattela M (2001) Cathepsin B acts as a dominant execution protease in tumor cell apoptosis induced by tumor necrosis factor. J. Cell. Biol. 153: 999–1010
Guicciardi ME, Miyoshi H, Bronk SF and Gores GJ (2001) Cathepsin B knockout mice are resistant to tumor necrosis factor-alpha-mediated hepatocyte apoptosis and liver injury: implications for therapeutic applications. Am. J. Pathol. 159: 2045–2054
Navab R, Chevet E, Authier F, Di Guglielmo GM, Bergeron JJ and Brodt P (2001) Inhibition of endosomal insulin-like growth factor-I processing by cysteine proteinase inhibitors blocks receptor-mediated functions. J. Biol. Chem. 276: 13644–13649
Darmon AJ, Nicholson DW and Bleackley RC (1995) Activation of the apoptotic protease CPP32 by cytotoxic T-cell-derived granzyme B. Nature 377: 446–448
Trapani JA, Davis J, Sutton VR and Smyth MJ (2000) Proapoptotic functions of cytotoxic lymphocyte granule constituents in vitro and in vivo. Curr. Opin. Immunol. 12: 323–329
Sutton VR, Davis JE, Cancilla M, Johnstone RW, Ruefli AA, Sedelies K, Browne KA and Trapani JA (2000) Initiation of apoptosis by granzyme B requires direct cleavage of bid, but not direct granzyme B-mediated caspase activation. J. Exp. Med. 192: 1403–1414
Heibein JA, Goping IS, Barry M, Pinkoski MJ, Shore GC, Green DR and Bleackley RC (2000) Granzyme B-mediated cytochrome c release is regulated by the Bcl-2 family members bid and Bax. J. Exp. Med. 192: 1391–1402
Waterhouse NJ, Finucane DM, Green DR, Elce JS, Kumar S, Alnemri ES, Litwack G, Khanna K, Lavin MF and Watters DJ (1998) Calpain activation is upstream of caspases in radiation-induced apoptosis. Cell Death Differ. 5: 1051–1061
Hiwasa T, Sawada T and Sakiyama S (1990) Cysteine proteinase inhibitors and ras gene products share the same biological activities including transforming activity toward NIH3T3 mouse fibroblasts and the differentiation-inducing activity toward PC12 rat pheochromocytoma cells. Carcinogenesis 11: 75–80
Hegde R, Srinivasula SM, Zhang Z, Wassell R, Mukattash R, Cilenti L, DuBois G, Lazebnik Y, Zervos AS, Fernandes-Alnemri T and Alnemri ES (2001) Identification of Omi/HtrA2 as a mitochondrial apoptotic serine protease that disrupts IAP–caspase interaction. J. Biol. Chem 277: 432–438
Verhagen AM, Silke J, Ekert PG, Pakusch M, Kaufmann H, Connolly LM, Day CL, Tikoo A, Burke R, Wrobel C, Moritz RL, Simpson RJ and Vaux DL (2001) HtrA2 promotes cell death through its serine protease activity and its ability to antagonise inhibitor of apoptosis proteins. J. Biol. Chem 277: 445–454
Martins LM, Iaccarino I, Tenev T, Gschmeissner S, Totty NF, Lemoine NR, Savopoulos J, Gray CW, Creasy CL, Dingwall C and Downward J (2001) The serine protease Omi/HtrA2 regulates apoptosis by binding XIAP through a Reaper-like motif. J. Biol. Chem 277: 439–444
van Loo G, van Gurp M, Depuydt B, Srinivasula SM, Rodriguez I, Alnemri ES, Gevaert K, Vandekerckhove J, Declercq W and Vandenabeele P (2002) The serine protease Omi/HtrA2 is released from mitochondria during apoptosis. Omi interacts with caspase-inhibitor XIAP and induces enhanced caspase activity. Cell Death Differ. 9: 20–26
Acknowledgements
We thank René Medema for providing the rat fibroblasts, Bob van de Water, Arnoud van der Laarse and Merlijn Bazuine for reagents, and Jennifer Rohn and Corrie Marijnen for critical reading of this manuscript. This work was supported by grants from the Vanderes Foundation, the J.A. Cohen Institute, the Dutch Science Organization and the Foundation Clinical Oncology Leiden.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by RA Knight
Rights and permissions
About this article
Cite this article
de Bruin, E., Meersma, D., de Wilde, J. et al. A serine protease is involved in the initiation of DNA damage-induced apoptosis. Cell Death Differ 10, 1204–1212 (2003). https://doi.org/10.1038/sj.cdd.4401296
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401296
Keywords
This article is cited by
-
Removal of uracil by uracil DNA glycosylase limits pemetrexed cytotoxicity: overriding the limit with methoxyamine to inhibit base excision repair
Cell Death & Disease (2012)
-
Non-caspase proteases: triggers or amplifiers of apoptosis?
Cellular and Molecular Life Sciences (2010)
-
Betulinic acid induces cytochrome c release and apoptosis in a Bax/Bak-independent, permeability transition pore dependent fashion
Apoptosis (2009)
-
Mechanistic insight into taxol-induced cell death
Oncogene (2008)
-
Pro-apoptotic activity of oncogenic H-Ras for histone deacetylase inhibitor to induce apoptosis of human cancer HT29 cells
Journal of Cancer Research and Clinical Oncology (2007)