Abstract
We evaluated the diagnostic utility of the histological characteristics ascribed in the literature to serrated adenomas and developed a practical working model to allow their reliable identification. We also documented the frequency and location of serrated adenomas identified in an unselected series of individuals undergoing colonoscopic evaluation, as well as the clinical characteristics of those individuals. One hundred forty consecutive individuals (prospective polyp data set; 97 male, 43 female; age mean: 63.3 y; age range: 29–98 y) with 255 polyps were identified from 919 individuals undergoing colonoscopy. Further polyps previously removed from these individuals were added for the purpose of histological assessment (extended polyp data set, n = 380). All polyps were assessed by two independent examiners for eight selected architectural and cytological features of serrated adenomas. In the prospective polyp data set, 56 patients had 72 hyperplastic polyps, 7 had 9 serrated adenomas, 3 had 4 admixed polyps, and 98 had 170 conventional adenomas. There was no difference in the age, sex, or cancer association of the seven patients with serrated adenomas when compared with the case of other individuals with polyps. The prevalence of serrated adenomas was 9/919 (1%) in our population, with an average size of 5.8 mm. When assessing serrated adenomas histologically, the combination of nuclear dysplasia and serration of ≥20% of crypts provided the most accurate model for detection of these lesions (sensitivity 100%, specificity 97%). Other criteria provided supportive evidence but did not increase the diagnostic yield. The optimum model for the histological identification of the serrated adenoma includes the presence of a serrated architecture in ≥20% of crypts in association with surface epithelial dysplasia.
Similar content being viewed by others
INTRODUCTION
The term serrated adenoma was first coined in 1990 by Longacre and Fenoglio-Preiser (1) to describe a discrete neoplastic lesion with a distinctive serrated architecture that contained areas of epithelial dysplasia. This terminology has now largely replaced the label “mixed hyperplastic adenomatous polyp,” which was used by Urbanski et al. (2) in their 1984 description of these lesions. Jass, working alone and in concert with others (3, 4, 5, 6), subsequently positioned this lesion as a key element in the serrated neoplasia pathway, and its role in the development of colorectal cancer has been the subject of considerable research interest. The serrated neoplasia pathway suggests that dysplasia can arise within hyperplastic colonic polyps, resulting in the formation of a serrated adenoma and potentially the development of colorectal carcinoma. The polyps of this pathway differ morphologically and genetically from polyps associated with the traditional adenoma–carcinoma sequence. They are characterized microscopically by the presence of crypts with prominent serrations and are characterized by certain genetic changes, including the presence of microsatellite instability in many cases (4, 5, 6, 7, 8, 9). Uncommonly, features of both hyperplastic polyps and conventional adenomas coexist as discrete elements within a single polyp. These lesions were described by Longacre as hyperplastic polyp/adenomas (1) and more recently by Jass as “admixed polyps” (10). Because microsatellite instability is a feature of both serrated adenomas and admixed polyps (5, 6, 11), Jass et al. (5) and Iino et al. (6) have postulated that these two lesions may share a common etiology and that together with hyperplastic polyps, they form a related group of lesions best referred to as serrated polyps.
Our knowledge of the frequency and distribution of the serrated adenoma arises solely from retrospective reviews using variable diagnostic and inclusion criteria. These data are also incomplete in the context of the vastly improved endoscopic diagnostic and therapeutic techniques available today. Most studies have reported a prevalence of 0.6 to 1.3%, but due to the difficulties with accurate data collection and histological definition, they are likely to be underestimates (1, 8). The predilection of serrated adenomas for the proximal colon, as reported by Longacre (1), is consistent with the concept of the serrated neoplasia pathway, because sporadic microsatellite unstable colorectal cancers favor a similar colonic distribution. However, this pattern of distribution remains to be confirmed in studies where colonoscopic assessment of the full colon has been made.
Much of the uncertainty regarding the epidemiology of serrated adenomas reflects the fact that the lesion itself has been incompletely defined and thus probably underdiagnosed. Longacre and Fenoglio-Preiser (1) have described several characteristics thought to aid in the differentiation of serrated adenomas from conventional adenomas and hyperplastic polyps. Likewise, in a 1996 study of patients with serrated adenomatous polyposis, Torlakovic and Snover (12) enumerated seven criteria characteristic of serrated adenomas. To date, none of these criteria have been formally tested with respect to accuracy or reproducibility of diagnosis.
The consistent morphological identification of serrated adenomas is prerequisite to gaining a clearer understanding of the serrated neoplasia pathway of colorectal carcinogenesis. In this study, we sought to evaluate the diagnostic utility of those histological characteristics that have been ascribed in the literature to serrated adenomas and sought to develop a practical working model to allow the reliable identification of serrated adenomas. We also documented the frequency and location of serrated adenomas identified in an unselected series of individuals undergoing colonoscopic evaluation, as well as the clinicopathological characteristics of those individuals.
METHODS
Study Population
The study population consisted of 919 consecutive patients who underwent colonoscopy with examination of the entire colon at the St Vincent's Hospital from July 1999 to December 2000. The indications for colonoscopy were typical of those seen in a general colonoscopy practice. From this population, 140 individuals (15%, 97 male, 43 female, mean age: 63.3 y, age range: 29–98 y) had a total of 255 histologically proven, nonmalignant, noninflammatory polyps resected (mean 2.0, median 1.0, range 1–13 per patient). These individuals and their polyps were referred to as the prospective polyp data set, and this was used for clinicopathological assessment. Nine individuals (7 male, 2 female) from the prospective polyp data set were found to have a colorectal carcinoma in association with their polyps. In these cases, polyps identified in subsequent colectomy specimens were also included in the prospective polyp data set, so as to avoid the potential undersampling of benign polyps that may occur at colonoscopy in the presence of a clearly malignant lesion.
In order to increase the number of serrated adenomas available for assessment of histological features, case records of the Department of Anatomical Pathology, St Vincent's Hospital were searched for any other colorectal polyps obtained between 1995 and 2001 from individuals in the prospective polyp data set. All histologically proven nonmalignant, noninflammatory polyps sampled at colonoscopy or colectomy from these individuals were added to those in the prospective polyp data set, and the resultant 380 polyps were referred to as the extended polyp data set.
In all cases, the size of polyps was recorded from the macroscopic pathological description, or in the case of polyps removed in fragments, from the reported size of the lesion as seen at colonoscopy.
Histological Assessment of the Extended Polyp Data Set
In order to define the histological criteria useful in characterizing serrated adenomas, three examiners (CB, NH, JT) independently reviewed 20 slides including serrated polyps and conventional adenomas, using the guidelines outlined by Longacre (1) and Torlakovic and Snover (12). A number of histological criteria had been suggested in the literature as relevant to the diagnosis of serrated adenomas, and in the preliminary phase of this study these criteria were evaluated in terms of their practicality and appropriateness for routine clinical practice. Several of these criteria involved quantitative traits not routinely evaluated by pathologists, including the degree of cytoplasmic eosinophilia, thickness of the collagen table, goblet cell dystrophy, differentiation, percentage per crypt zone, total mucin content and endocrine cell count. Although complex qualitative ranking systems have been proposed for the description of some of these criteria (12), we considered that their assessment was likely to be impractical, or at least poorly reproducible, in routine clinical practice. For this reason they were excluded, and as outlined below a final set of eight histological characteristics was agreed on and tested in a blinded fashion. For each polyp in the extended polyp data set, these eight architectural and cytological characteristics were independently assessed by two examiners (CB, NH).
Five architectural features were assessed. They included (1) serration of the epithelial crypt, characterized by infolding of the epithelium in a sawtooth fashion within the crypt lumen; (2) architectural atypia, characterized by nonuniformity of the crypt structure, and in particular by branching, budding and complexity of the crypt; (3) horizontal crypt orientation, defined as the horizontal alignment of the long axis of the crypt or part of the crypt when compared with the surface epithelium; (4) basal crypt dilatation, where the luminal diameter of the crypt was significantly wider at its base; and (5) surface tufting, in which apical protrusions in the cytoplasm of surface epithelial cells produced a tufted or budded appearance in the presence of an even basement membrane.
The three cytological features assessed included the following: (1) surface epithelial dysplasia, characterized by the presence in surface epithelial cells of pleomorphic, hyperchromatic nuclei, nuclear elongation and pseudostratification, and prominent and/or irregular nucleoli; (2) increased surface mitoses, as evidenced by an equal or greater number of mitotic figures in upper crypt or surface epithelium in comparison with basal crypt zones; and (3) mucin depletion within crypt or surface epithelium in comparison to adjacent normal epithelium (1, 12, 13, 14, 15). All parameters were scored as either present or absent, with the exception of serration, which was ranked on the basis of the percentage of lesional crypts that showed at least some evidence of serration at some point along their length. The percentage of serration was arbitrarily assigned to the following categories: 0, 1–19%, 20–49%, ≥50%.
Where polyps contained areas of dysplasia associated with a serrated architecture, histological characteristics of that specific area were recorded. In admixed polyps, which were characterized by foci of dysplastic but nonserrated epithelium in immediate proximity to serrated but nondysplastic epithelium, data from the area with maximal dysplasia and the area with maximal serration were recorded. The diagnosis of each polyp was recorded as hyperplastic polyp, conventional adenoma, serrated adenoma, or admixed polyp.
After completion of the independent assessment of each polyp, the diagnoses of all lesions were compared. Where there was disagreement (n = 4), the slide was jointly re-assessed, a consensus reached, and a final diagnosis agreed upon for the purpose of later comparison.
Statistics
An independent sample t test was used when comparing the ages of individuals with different polyp types, as well as polyp size. Categorical variables including sex, mode of presentation, association with cancer, polyp distribution, and the presence of other types of polyps were compared using a χ2 test. Where any cell had a frequency of less than five, a Fisher's exact probability test was performed.
A κ score was used to assess the measure of agreement between examiners for each histological characteristic evaluated. A score of 0–0.2 was considered to represent slight agreement; 0.2–0.4, fair; 0.4–0.6, moderate; 0.6–0.8, substantial; and >0.8, almost perfect agreement (16, 17).
RESULTS
Extended Polyp Data Set—assessment of Histological Criteria
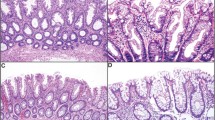
In the histological assessment of polyps, the presence of serrated crypts was reliably detected when it was present to a substantial degree. Likewise, surface epithelial dysplasia, increased surface mitoses, and surface epithelial tufting were also reliably detected (Fig. 1). Kappa scores reflected these findings (Table 1), with surface epithelial tufting and increased surface mitoses scoring moderate or higher levels of agreement between examiners, whereas surface epithelial dysplasia and the presence of luminal serrations in ≥20% of crypts scored an almost perfect level of agreement between examiners.
Photomicrograph of typical serrated lesions showing some of the features examined in this study. The top panel shows a serrated adenoma with (A) serrations seen within all crypt lumens, as well as surface tufting. A higher power view (B) shows detail of surface dysplasia, as well as surface tufting (convex cytoplasmic protrusions along the luminal surface formed by several cells and separated by shallow notched indentations). The bottom panel shows a hyperplastic polyp with prominent basal crypt dilation (C) and a serrated adenoma showing marked architectural atypia, as evidenced by complex branching papillary structures (D). Hematoxylin and eosin; magnification: A = 120×, B = 360×, C = 30×, D = 24×.
In contrast, the assessment of other histological characteristics showed poor interobserver correlation. These included basal crypt dilatation and horizontal crypt alignment, which were difficult to report because of uncertainty regarding the extent to which these changes should be considered significant. Likewise, mucin depletion proved difficult to assess accurately, largely because of marked variation in the density of goblet cells in adjacent normal and lesional epithelium.
The most sensitive tests for the identification of a serrated adenoma when used in isolation were surface epithelial dysplasia, surface epithelial tufting, and the presence of at least low levels of luminal serration. When used alone, each of these criteria had a high negative predictive value, but none were very specific for their diagnosis (Table 2). The combination of surface epithelial dysplasia and crypt serration markedly improved the sensitivity and specificity of the tests; a result of little surprise given that these are the accepted hallmarks of the diagnosis of serrated adenomas. The precise degree of serration necessary to define serrated adenoma, however, has never been specified. When the lesions were defined by the presence of serration in any crypt within the polyp that also shows dysplasia, then all serrated adenomas were correctly identified (sensitivity 100%). However, these criteria had a 19% false-positive rate because of the inclusion of numerous conventional adenomas with minor degrees of serration, yielding a specificity of 81%. The identification of serration in ≥20% of crypts, again in association with dysplasia, provided the most accurate set of diagnostic criteria (sensitivity 100%, specificity 97%). Where dysplasia was associated with the finding of luminal serration in at least half of all crypts within the polyp, the diagnosis of serrated adenoma could be made with high specificity, but sensitivity was reduced to 89%, because 2 of the 17 serrated adenomas were excluded using these criteria.
The optimum model for the diagnosis of serrated adenomas therefore included the presence of serrations in ≥20% of the lesion crypts in association with surface epithelial dysplasia. A flow chart outlining a proposed diagnostic schema for serrated adenomas is shown in Figure 2.
Patient Demographics
Using the 919 individuals undergoing colonoscopy who formed the prospective polyp data set, we were able to make the following observations regarding the clinicopathological features of serrated polyps. We found that overall, 15% (140/919) of the individuals in this group had at least one nonmalignant, noninflammatory polyp. Hyperplastic polyps were found in 6% (56/919) of these individuals, with serrated adenomas in 1% (9/919) and conventional adenomas in 11% (98/919).
A total of 117 (13%) individuals had only one polyp (38 hyperplastic polyps, 78 conventional adenomas, 1 serrated adenoma). A further 23 individuals (3%) had multiple lesions, with 15 having hyperplastic polyps and conventional adenomas; 4 having serrated adenomas and hyperplastic polyps; 2 having conventional adenomas and admixed polyps; 1 having conventional adenomas, serrated adenomas, and admixed polyps; and 1 having hyperplastic polyps as well as conventional and serrated adenomas. Of the seven individuals with serrated adenomas, one had three of these lesions, and the remainder had a single lesion each. Patients with serrated adenomas were no more likely to harbor associated hyperplastic polyps than they were conventional adenomas.
The most common causes for presentation in patients with a serrated adenoma were anemia (30%) and a personal history of colonic polyps or cancer (30%). Common presentations for those with other lesions were a past history of colonic polyp or colorectal carcinoma (31%) and rectal bleeding (19%), but there was no statistically significant difference between the groups. There was no difference in the age (mean: 64 y, range: 54–87 y) or sex (4 male and 3 female) of the seven patients with serrated adenomas when compared with other individuals with polyps.
Of the nine patients found to have colorectal cancer, two were female and seven male, with a mean age of 70 years (range: 59–87 y). One of these patients had 15 polyps, including 11 conventional adenomas, 3 serrated adenomas, and 1 admixed polyp. The remaining eight individuals had between one and four polyps. Four of these had only conventional adenomas, three had both conventional adenomas and hyperplastic polyps, and one had only hyperplastic polyps.
Polyp Characteristics
Of the 255 polyps identified in the prospective polyp data set, nine (3.5%) were serrated adenomas, four (1.5%) were admixed polyps, 72 (28%) were hyperplastic polyps, and 170 (67%) were conventional adenomas. Serrated adenomas identified within the prospective polyp data set showed no statistical differences in terms of polyp size or location within the bowel when compared with admixed polyps, hyperplastic polyps, or conventional adenomas, either alone or in combination (Table 3).
DISCUSSION
This study has evaluated the histological features of serrated adenomas and in doing so has demonstrated, at least in the current data set, that the presence of dysplasia and a serrated architecture alone are the cornerstones of reliable and accurate diagnosis.
We found that although serrations were present in the majority of lesional crypts in most serrated adenomas (15/17), some lesions considered to be serrated adenomas showed lower levels of serration. It was noteworthy that in accepting a level of serration as low as 20% of lesional crypts, we were able to increase the sensitivity of the diagnostic criteria, without compromising specificity. The extent of serration has not been reported in this semiquantitative manner in previous histological reviews but instead has been described qualitatively, using terms such as “prominent” (12) or “marked in most cases” (1). Variation in the degree of serration present in serrated adenomas may be attributable to differences in the extent of dysplasia in individual lesions or may reflect variation in the plane of section relative to crypt length. In any event, we would argue that it is reasonable to include within the category of serrated adenoma any lesion showing clear evidence of serration within ≥20% of lesional crypts. The validity of this claim will require evaluation by other investigators, using other sets of lesions.
Surface epithelial dysplasia is the key feature differentiating serrated adenomas from hyperplastic polyps. It has been assessed in detail in past histological reviews of serrated adenomas (1, 12) and its recognition has not previously been problematic. In Longacre and Fenoglio-Preiser's review (1) of 110 serrated adenomas, 50% had formerly been diagnosed as conventional adenomas, although only 28% were diagnosed as hyperplastic polyps. This suggests that the presence of serration was the histological feature more likely to be discounted than the presence of dysplasia. In our assessment of 380 polyps, there was strong agreement in the identification of dysplasia and subsequently, 100% sensitivity for the diagnosis of serrated adenomas.
We found that surface epithelial tufting and increased surface mitoses were reproducible features in the assessment of polyps, with both having substantial levels of agreement between study examiners. Surface epithelial tufting, which may well represent a superficial manifestation of crypt serration, was easily recognized in our study. However, these characteristics added little in terms of sensitivity and specificity to the diagnostic model for serrated adenomas and should therefore be viewed only as supporting the diagnosis. Other criteria previously reported in the literature as diagnostic features of serrated adenoma, including basal crypt dilatation, horizontal crypt alignment, and mucin depletion, were included for evaluation as their presence or absence should in theory be readily identifiable by the pathologist. However, we found that they were unreliable as diagnostic criteria, as evidenced by the low levels of agreement between study examiners.
In terms of patient demographics and the frequency of polyp types, the prospective polyp data set used in this study was broadly consistent with other colonoscopy-based studies (1, 18, 19, 20). Individuals with serrated adenomas in our study showed similar demographics, including age and gender, to those reported in other large colonoscopy groups (1, 18). Likewise, the average size of serrated adenomas identified in our study (5.8 mm) was consistent with the finding of other groups (2–10 mm; 1, 12, 21, 22, 23, 24).
It is interesting to note however that our diagnostic model detected a greater frequency of serrated adenomas (3.5%) when compared with the findings of Matsumoto et al. (18; 1.3%) and Longacre and Fenoglio-Preiser (0.6%; 1). One important explanation for this apparent discrepancy may relate to the methodology of polyp accrual. Notably, Matsumoto and colleagues (18) did not examine the colectomy samples of study patients found to have carcinoma, and this may have reduced their yield of polyps, whereas in the Longacre and Fenoglio-Preiser (1) study, patients were included regardless of the extent of colonoscopic examination. Interestingly, one of the eight individuals whose colectomy sample was examined was found to have an additional three serrated adenomas. Their inclusion in the prospective polyp data set was a source of significant bias in terms of serrated adenoma frequency. When serrated adenomas found at colectomy (n = 3) were excluded from our data set, the frequency of serrated adenomas was reduced to 2.4%.
Despite this, we consider the expanded criteria used in our study to be reasonable in view of the considerable uncertainty in the literature regarding the biological significance of serrated adenomas. Only when clear biological markers of serrated adenoma and the serrated-neoplasia pathway are available will their true morphological characteristics be established. In this study we have explored the diagnostic criteria proposed in the histopathological literature, and have identified those criteria most likely to perform reliably and accurately in clinical practice. Our results confirm that the serrated adenoma is an infrequent but distinctive lesion and is one that is associated with colorectal cancer. Our findings may help to both clarify and simplify the ongoing recognition of these lesions.
References
Longacre TA, Fenoglio-Preiser CM . Mixed hyperplastic adenomatous polyps/serrated adenomas. A distinct form of colorectal neoplasia. Am J Surg Pathol 1990; 14: 524–37.
Urbanski SJ, Kossakowska AE, Marcon N, Bruce WR . Mixed hyperplastic adenomatous polyps—an underdiagnosed entity. Report of a case of adenocarcinoma arising within a mixed hyperplastic adenomatous polyp. Am J Surg Pathol 1984; 8: 551–6.
Jass JR . Serrated route to colorectal cancer: back street or super highway? J Pathol 2001; 193: 283–5.
Jass JR, Biden KG, Cummings MC, Simms LA, Walsh M, Schoch E, et al. Characterisation of a subtype of colorectal cancer combining features of the suppressor and mild mutator pathways. J Clin Pathol 1999; 52: 455–60.
Jass JR, Young J, Leggett BA . Hyperplastic polyps and DNA microsatellite unstable cancers of the colorectum. Histopathology 2000; 37: 295–301.
Iino H, Jass JR, Simms LA, Young J, Leggett B, Ajioka Y, et al. DNA microsatellite instability in hyperplastic polyps, serrated adenomas, and mixed polyps: a mild mutator pathway for colorectal cancer? J Clin Pathol 1999; 52: 5–9.
Jass JR, Iino H, Ruszkiewicz A, Painter D, Solomon MJ, Koorey DJ, et al. Neoplastic progression occurs through mutator pathways in hyperplastic polyposis of the colorectum. Gut 2000; 47: 43–9.
Makinen MJ, George SM, Jernvall P, Makela J, Vihko P, Karttunen TJ . Colorectal carcinoma associated with serrated adenoma—prevalence, histological features, and prognosis. J Pathol 2001; 193: 286–94.
Hawkins NJ, Ward RL . Sporadic colorectal cancers with microsatellite instability and their possible origin in hyperplastic polyps and serrated adenomas. J Natl Cancer Inst 2001; 93: 1307–13.
Jass JR . Serrated adenoma of the colorectum. Curr Diag Pathol 2002; 8: 42–9.
Loukola A, Salovaara R, Kristo P, Moisio AL, Kaariainen H, Ahtola H, et al. Microsatellite instability in adenomas as a marker for hereditary nonpolyposis colorectal cancer. Am J Pathol 1999; 155: 1849–53.
Torlakovic E, Snover DC . Serrated adenomatous polyposis in humans. Gastroenterology 1996; 110: 748–55.
Wiebecke B, Brandts A, Eder M . Epithelial proliferation and morphogenesis of hyperplastic adenomatous and villous polyps of the human colon. Virchows Arch A Pathol Anat Histol 1974; 364: 35–49.
Estrada RG, Spjut HJ . Hyperplastic polyps of the large bowel. Am J Surg Pathol 1980; 4: 127–33.
Fenoglio-Preiser C . Colonic polyp histology. Semin Colon Rectal Surg 1991; 2: 234–45.
Landis J, Koch G . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74.
Armitage P, Berry G, Matthews J . Statistical methods in medical research. 4th ed. Oxford, United Kingdom: Blackwell; 2002.
Matsumoto T, Mizuno M, Shimizu M, Manabe T, Iida M . Clinicopathological features of serrated adenoma of the colorectum: comparison with traditional adenoma. J Clin Pathol 1999; 52: 513–6.
Coode PE, Chan KW, Chan YT . Polyps and diverticula of the large intestine: a necropsy survey in Hong Kong. Gut 1985; 26: 1045–8.
Williams AR, Balasooriya BA, Day DW . Polyps and cancer of the large bowel: a necropsy study in Liverpool. Gut 1982; 23: 835–42.
Tateyama H, Li W, Takahashi E, Miura Y, Sugiura H, Eimoto T . Apoptosis index and apoptosis-related antigen expression in serrated adenoma of the colorectum: the saw-toothed structure may be related to inhibition of apoptosis. Am J Surg Pathol 2002; 26: 249–56.
Yao T, Kouzuki T, Kajiwara M, Matsui N, Oya M, Tsuneyoshi M . “Serrated” adenoma of the colorectum, with reference to its gastric differentiation and its malignant potential. J Pathol 1999; 187: 511–7.
Iwabuchi M, Sasano H, Hiwatashi N, Masuda T, Shimosegawa T, Toyota T, et al. Serrated adenoma: a clinicopathological, DNA ploidy, and immunohistochemical study. Anticancer Res 2000; 20: 1141–7.
Fogt F, Brien T, Brown CA, Hartmann CJ, Zimmerman RL, Odze RD . Genetic alterations in serrated adenomas: comparison to conventional adenomas and hyperplastic polyps. Hum Pathol 2002; 33: 87–91.
Acknowledgements
We thank the Gastroenterology Department of St Vincent's Hospital for their generous support of this study.
This project was supported by grants from St Vincent's Hospital Clinic Foundation, the Ernest Heine Foundation, and the NSW State Cancer Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bariol, C., Hawkins, N., Turner, J. et al. Histopathological and Clinical Evaluation of Serrated Adenomas of the Colon and Rectum. Mod Pathol 16, 417–423 (2003). https://doi.org/10.1097/01.MP.0000068236.47471.DB
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.MP.0000068236.47471.DB
Keywords
This article is cited by
-
Can the rate and location of sessile serrated polyps be part of colorectal Cancer disparity in African Americans?
BMC Gastroenterology (2019)
-
The significance of ectopic crypt formation in the differential diagnosis of colorectal polyps
Diagnostic Pathology (2014)
-
Traditional serrated adenoma has two pathways of neoplastic progression that are distinct from the sessile serrated pathway of colorectal carcinogenesis
Modern Pathology (2014)
-
Defined morphological criteria allow reliable diagnosis of colorectal serrated polyps and predict polyp genetics
Virchows Archiv (2014)
-
Serrated Lesions of the Colorectum: Review and Recommendations From an Expert Panel
American Journal of Gastroenterology (2012)