Abstract
The distinction between acute rejection and early recurrent hepatitis C infection (RHCV) in the setting of orthotopic liver transplantation is often difficult. In liver biopsies acidophil bodies and lobular hepatitis are used to suggest a diagnosis of RHCV over rejection, however, the reliability of this practice has not been established. Because portal tract changes in RHCV and rejection often overlap, we sought to determine whether the degree of hepatocyte acidophil body formation seen on liver biopsies could be used to distinguish between these two conditions. Methods: Quantification of acidophil bodies was performed on liver biopsies in orthotopic liver transplant patients with RHCV (n = 10), non-hepatitis C orthotopic liver transplant patients with uncomplicated rejection episodes (n = 10) and non-transplant patients with chronic hepatitis C infection (n = 10). Hematoxylin and Eosin stained slides from all three groups were randomized and tissue segments 1.0 cm in length and of variable width (0.04–0.13 cm) were examined at 200 × magnification in a blinded fashion by two pathologists in order to quantify the number of acidophil bodies/cm2. Lobular chronic inflammation was also graded on a 0–3+ scale. Results: Liver biopsies taken at the onset of RHCV exhibited 606 ± 101 acidophil bodies/cm2 (mean ± standard error of mean, range 200–1390). These counts were significantly greater (P = .0061, paired 2-tailed t-test) than the 241 ± 53 acidophil bodies/cm2 (range 80–514) for acute rejection, and the 194 ± 21 acidophil bodies/cm2 (range 100–333) for non-liver transplant chronic hepatitis C infection (P = .0013). No difference in lobular inflammation between index RHCV and rejection biopsies was detected. Conclusions: Although there is overlap, on average there are twice as many acidophil bodies in the initial stage of RHCV when compared with acute rejection (average of 55 per linear cm in RHCV versus 21 per linear cm for rejection). Lobular inflammation was not a reliable indicator of the initial onset of RHCV.
Similar content being viewed by others
INTRODUCTION
End stage liver disease due to chronic hepatitis C (HCV) infection is the commonest indication for orthotopic liver transplantation (OLT) in the United States, accounting for 25–35% of all patients on the waiting lists of major transplant centers (1, 2, 3, 4). In spite of the almost 80% incidence of recurrent hepatitis in the engrafted liver (5), excellent long-term graft and patient survival justify OLT as the preferred modality of therapy for end-stage HCV infection (6, 7, 8, 9, 10). This satisfactory outcome however, mandates judicious use of immunosuppression in the treatment of rejection, since such therapy can trigger or enhance viral replication and accelerate graft loss (7, 8, 9, 11, 12, 13, 14). The emphasis is therefore on accurate diagnosis of recurrent hepatitis C (RHCV), and its distinction from other causes of elevated liver enzymes or disordered liver function. Reinfection of the allograft as detected by the presence of hepatitis C RNA by RT-PCR is universal, and can occur within weeks of transplantation (15, 16, 17, 18). This however does not necessarily imply hepatitis, so that liver biopsy remains the only available tool to distinguish reinfection from recurrent hepatitis.
The extensive literature on the histology of hepatitis C predominantly characterizes the chronic phase of the infection in the native liver (19, 20), since acute hepatitis C is rarely encountered in clinical practice or on biopsy material. On the other hand, biopsies of the liver allograft in the early stages of recurrent hepatitis chronicle the acute phase of the infection, which can itself be expected to have been modified by the immunological milieu of the graft and host. In addition, the allograft is subject to other concomitant processes in the post-transplant period that could further complicate the histological findings. Especially distressing is the histological overlap between RHCV and cellular rejection, as these two conditions dictate opposite therapeutic management. Both can show chronic portal inflammation, duct damage and apoptosis of hepatocytes. Even endothelialitis is occasionally seen in RHCV (20, 21). It is also well known that rejection and hepatitis can occur in the same patient and can both be present in a single biopsy (14, 21, 22). Several studies attempting to distinguish these two entities highlight steatosis, lobular inflammation, and spotty necrosis as features that favor hepatitis over rejection (23, 25). One such study compared the histology of acute rejection and RHCV infection by evaluating 44 histologic changes in portal tracts and lobules. While several portal tract changes were significantly associated with acute rejection, there were no specific histologic correlates to recurrent hepatitis (23).
Given the histological overlap that can occur between rejection and RHCV infection, we sought to determine whether the assessment of lobular changes, especially acidophil body formation, is helpful both in detecting RHCV and in distinguishing it from rejection. Liver biopsies from three groups of patients were evaluated: OLT patients with well documented RHCV infection, non-hepatitis C OLT patients with typical rejection episodes, and non-OLT chronic hepatitis C patients who underwent biopsies for staging. Acidophil bodies and lobular inflammation were compared between these three groups.
METHODS
The database of the Department of Medicine, Division of Digestive Diseases at Yale New-Haven Hospital was searched for all patients transplanted for end-stage liver disease due to chronic Hepatitis C infection. The pathology files of these patients were reviewed revealing 10 patients who had RHCV in their grafts but no other post-transplantation complications, and long-term follow-up.
An average of 4.5 serial biopsies on each patient (range 2–7) was examined and the persistence of hepatitis in serial biopsies was confirmed in all 10 patients. All biopsies in this group and the rejection group (see below) had been obtained to evaluate the cause of increased liver function tests (no protocol biopsies). The first biopsy that showed evidence of RHCV was designated as the index biopsy. The index and all subsequent biopsies of these patients were also included in order to evaluate the trend of acidophil bodies over time.
Two comparison groups were included. The first consisted of 10 biopsies showing rejection as the sole pathology from patients who had been transplanted for reasons other than chronic hepatitis C infection. The biopsies were reviewed to confirm the diagnosis of rejection and to rule out other co-existing complications. The degree of rejection was graded in each biopsy according to the recommendations published in the Banff consensus document (26). The medical records of these patients were reviewed to confirm normalization of liver function tests following appropriate immunosuppressive therapy. Liver biopsies taken within the first 2 weeks of transplantation (present only in the rejection group) were excluded to avoid acidophil bodies associated with reperfusion injury. The second comparison group consisted of 10 biopsies from patients being followed for chronic hepatitis C infection who had not been transplanted.
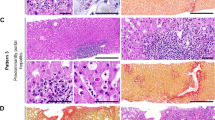
A total of 65 Hematoxylin and Eosin (H and E) stained slides were obtained, representing formalin fixed, paraffin embedded liver tissue cut at 3 μm. These included 45 slides from recurrent hepatitis C patients (10 index biopsies and 35 additional serial biopsies), 10 biopsies showing rejection and 10 from the non-transplanted hepatitis C group. After coding and randomization of all 65 slides, a 1 cm intact segment of liver tissue, free of tears was marked off on each biopsy and the average width of the biopsy measured. Aside from the above technical considerations, the 1 cm length of tissue was selected randomly, and was not chosen on the basis of histologic findings therein. The number of acidophil bodies in this area was counted simultaneously by two pathologists at 200 × magnification. Acidophil bodies were defined as well demarcated, eosinophilic cytoplasmic globules, either anuclear or possessing nuclear fragments lying within the lobules, sinusoids or in periportal areas. The results are expressed as absolute values; that is, the number of acidophil bodies counted in a 1 cm length of tissue, (AB/cm) and as AB/cm2. Statistical significance was tested by the paired student 2-tailed t-test.
Biopsies were also assessed for the degree of lobular inflammation independently from the acidophil body quantitation. For each of these parameters, randomized slides were examined simultaneously by the same two hepatopathologists at 100 × magnification. Lobular inflammation was defined by the presence of mononuclear inflammatory cells (lymphocytes and plasma cells) within the hepatic lobules. Portal and interface inflammatory cells were excluded from this assessment. Using these criteria, a score of 0–3+ was given for the degree of lobular inflammation present. The biopsies from non-transplant patients with chronic hepatitis C infection were graded and staged using established criteria (27).
RESULTS
Clinical Data
The 10 patients transplanted for end-stage liver disease due to chronic hepatitis C infection that had RHCV without other concomitant pathology consisted of eight men and two women. They ranged in age from 35–53 years at the time of transplantation (mean 45.2 years). The follow-up period ranged from 1.3 to 8 years (mean 4.2 years). These 10 patients had 45 biopsies in all, taken from 6 weeks to 5 years following transplantation. The first or index biopsies were taken between 3 and 20 months after transplantation. Following transplantation, three patients had received tacrolimus and prednisone for immunosuppression; one patient had received mycophenolate in addition to tacrolimus and prednisone, five patients had received cyclosporin and prednisone, and one patient had received Imuran in addition to cyclosporin and prednisone (Table 1).
The 10 biopsies showing rejection were taken from eight patients. Two separate rejection episodes occurring more than 4 months apart in two patients were included, the patients having responded completely to steroid therapy following each episode of rejection. There were four males and four females ranging from 2–64 years of age (mean 26 years). They had been transplanted for biliary atresia, alpha-1 antitrypsin deficiency, hepatoblastoma, primary biliary cirrhosis, primary sclerosing cholangitis, paracetamol overdose, Wilson's disease and autoimmune hepatitis (1 patient each). In the patient with a history of autoimmune hepatitis, both the histology and clinical follow-up after biopsy were characteristic of rejection. There was no evidence of recurrent autoimmune hepatitis. The biopsies ranged from 4 weeks to over 2 years following transplantation. Four biopsies showed mild, five showed moderate and one showed severe rejection (Table 2).
The 10 patients being followed up for chronic HCV consisted of seven men and three women. They ranged in age from 36 to 48 years (mean 42.5 years). Three patients had used intravenous drugs 8, 28, and 32 years prior to the biopsy. Two patients had received blood transfusions 22 and 26 years before the biopsy was taken. The time interval in a third patient who received a blood transfusion is not known. One of the patients was a phlebotomist who remembered inadvertent needle-stick injuries approximately 10 years ago. In the remaining three patients the risk factor for acquiring hepatitis C infection was unknown (Table 3).
Pathology
The index biopsies of patients with RHCV infection had on average more than twice as many AB/cm2 than the rejection and non-transplanted hepatitis C groups (Table 4, Fig. 1). The index liver biopsies of patients with RHCV exhibited between 200–1390 AB/cm2 (606 + 101 AB/cm2, mean ± standard error of mean). The biopsies with acute cellular rejection showed 80–514 AB/cm2(241 + 53 AB/cm2) and those of non-transplanted HCV showed 100–333 (194 + 21 AB/cm2). This difference in acidophil bodies between the index biopsies from RHCV patients and the two other groups was statistically significant (rejection, P = .0061; HCV, P = .0014, 2-tailed t-test). When serial biopsies from RHCV patients were combined (Table 5) and compared with the rejection group the difference persisted and continued to be significant (P < .0014, 2-tailed t-test). Also shown in Table 4 is the absolute number of AB/cm. While AB/cm do not take into account the width of the needle biopsies, they provide a snapshot of the number of acidophil bodies that were observed at the microscope in a 1 cm length of tissue.
The number of acidophil bodies/cm2 in liver biopsies from patients with non-transplanted chronic hepatitis C infection (HCV), acute rejection (AR) and recurrent hepatitis C infection (RHCV) are compared. On average there were twice as many acidophil bodies in biopsies from patients with RHCV than in either AR or HCV. See Table 4 for statistical analysis.
Table 5 shows the trend in the number of acidophil bodies over time in patients with RHCV. In four patients, the acidophil bodies seemed to increase over time whereas in another 4, they seemed to decrease over the duration of follow-up. The remaining two patients had only two biopsies at the time of this study. Thus, there appeared to be no definite trend in the number of acidophil bodies over time in RHCV infection.
The number of acidophil bodies in patients with acute rejection showed no relationship to the time after transplant; high numbers of acidophil bodies were found at both 6 weeks and at 2 years post-transplant (Table 2, cases 5 and 9). No correlation was found between the grade of rejection and number of acidophil bodies in this small sample. The difference between the number of acidophil bodies in staging biopsies for HCV and rejection was not statistically significant.
The stage and grade of biopsies for HCV in non-transplant patients were as follows. The inflammatory activity was grade one in two, grade two in five, and grade three in three patients. The degree of fibrosis was stage one in four and stage two in six patients (Table 3). No definite correlation was found between the number of acidophil bodies and grade or stage in this sample.
There was no difference in the degree of lobular inflammation in the index biopsies of patients with RHCV when compared with rejection or non-transplanted HCV infection. Only 4/10 RHCV patients had a score greater than 0, and only one of these had a score greater than 1 for lobular inflammation. Three patients each from the rejection and non-transplanted chronic hepatitis C groups had a score of 1 for lobular inflammation. The remaining patients in all three groups had a score of 0 for this parameter.
DISCUSSION
Studies documenting the histology of early RHCV and its distinction from acute rejection are few. Specific histological features that have been attributed to RHCV are sinusoidal dilatation, steatosis, chronic portal inflammation, Kupffer cell activation, spotty necrosis and acidophil bodies (23, 24, 25). However, except for acidophil bodies, these parameters are not easily quantifiable and are therefore subjective and difficult to evaluate uniformly in practice. To our knowledge this study represents the first quantitative comparison of acidophil bodies between recurrent hepatitis C infection and acute cellular rejection after orthotopic liver transplantation. We found a significant difference in acidophil bodies between these two groups; namely that index biopsies of RHCV (the first biopsy obtained at the onset of recurrent hepatitis) have on average twice as many acidophil bodies as biopsies showing acute rejection in non-hepatitis C patients. Serial biopsies in patients with RHCV continued to show significantly more acidophil bodies than the rejection biopsies.
A substantial number of acidophil bodies (range 80–514 AB/cm2) were present on routine H and E sections in acute rejection. These were present to such a degree that the number of acidophil bodies found in acute rejection, both early and late after transplantation, overlapped with that found in RHCV (Table 4). Although there was no correlation between rejection grade and number of acidophil bodies in this study, a larger series of biopsies showing rejection would have to be evaluated to rigorously evaluate such a correlation.
The criteria for the diagnosis of acute rejection described in the Banff International Consensus Document (26) consist of the triad of mixed portal inflammation, cholangiolitis and endothelialitis. Hepatocyte necrosis is mentioned as a significant feature only in severe rejection. Apoptosis, the molecular correlate of the acidophil body, is not specifically mentioned. However, a number of studies have documented the presence of apoptosis in both acute and chronic rejection using in situ nick end labeling (28, 29). In particular, apoptosis was documented in 65 biopsies showing acute rejection of mild to severe degree, and occurred randomly throughout the hepatic lobules, within bile ducts and in inflammatory cells (29). However, in the study by Tannapfel et al. (28), the number of apoptotic cells by in situ nick end labeling in 18 biopsies from patients with RHCV was significantly greater than in that found in acute rejection. Thus, it appears that histologic assessments of acidophil bodies correlate with the molecular detection of apoptosis in both acute rejection and recurrent hepatitis C infection. Of note, apoptosis is not found to a significant degree in stable liver allografts (28).
Significantly fewer acidophil bodies were found in non-transplanted chronic hepatitis C biopsies than in biopsies from OLT patients with RHCV. These results may reflect differences in active hepatocyte injury seen in longstanding disease (range of 8–32 years in non-transplant group) compared with acute infection of a previously negative liver in the RHCV group (range 6–81 weeks post-OLT). The difference between these two groups could also be secondary to immunosuppression in OLT patients, which provides a permissive environment for viral replication.
No difference in lobular inflammation was found between index RHCV, rejection and non-transplanted HCV biopsies. In fact, with one exception, lobular inflammation was very mild across all three groups. Similar data has previously been reported by Khettry et al. (25), who found that apoptosis may be one of the early indicators of recurrent hepatitis C, before the onset of lobular inflammation. This is not entirely unexpected, as the recipient of a transplant, unlike the immunocompetent individual with hepatitis C infection, may not mount an adequate immune response to virally infected cells. This finding highlights the fact that although mild to moderate lobular inflammation is usually found in chronic HCV, initial biopsies demonstrating acute reinfection of liver grafts may not show this feature. Reliance on lobular inflammation for the diagnosis of recurrent hepatitis may therefore not be sufficient.
The lack of a trend in the number of acidophil bodies in serial biopsies over the follow-up period (6 weeks to 5 years) is likely related to several factors. The most important factor is therapeutic modulation of immunosuppressive regimens among patients with suspected RHCV. Alternatively, this may be a reflection of the waxing and waning course of the disease itself.
Our study is interesting in view of previous studies documenting overlapping histology in the portal tracts between RHCV and rejection (14, 21, 23), as it reveals the overlap in the number of acidophil bodies in these two conditions. However, in spite of the overlap, the index RHCV group had on an average twice as many acidophil bodies as that seen in acute rejection, which supports the practice of using acidophil bodies as an indicator of recurrent hepatitis C. It may be possible to improve diagnostic accuracy by using rough estimates of AB/cm obtained by scanning the length of the biopsy core at medium magnification (200 ×). The addition of width measurements, while important for study purposes, is not necessary in daily practice.
CONCLUSION
Although one should not be dogmatic in using quantitation, our data suggest that >35 apoptotic hepatocytes per cm would favor a diagnosis of RHCV, and >50 apoptotic hepatocytes per cm would strongly implicate RHCV (Table 4). While AB/cm cannot stand alone as a criterion for differentiating allograft rejection from RHCV, our data demonstrate that there is value in including such data in the histopathologic assessment algorithm. As the occurrence of allograft rejection versus RHCV is heavily influenced by clinical treatment, future studies will be required to evaluate the progression of hepatocellular apoptosis in patients who fluctuate between these two conditions or have them simultaneously. The data presented in this study demonstrate that acidophil body estimates, in conjunction with portal tract histologic changes, do have value as an early indicator of RHCV infection and can be used to discriminate between rejection and RHCV.
References
Belle SH, Beringer KC, Detre KM . Trends in liver transplantation in the United States. Clin Transplant 1993; 19–35.
Ascher NL, Lake JR, Emond J, Roberts J . Liver transplantation for hepatitis C virus-related cirrhosis. Hepatology 1994; 20(1 Pt 2): 24S–27S.
Terrault NA, Wright TL . Hepatitis C virus in the setting of transplantation. Semin Liver Dis 1995; 15: 92–100.
Araya V, Rakela J, Wright T . Hepatitis C after orthotopic liver transplantation. Gastroenterology 1997; 112: 575–582.
Greenson JK, Svoboda-Newman SM, Merion RM, Frank TS . Histologic progression of recurrent hepatitis C in liver transplant allografts. Am J Surg Pathol 1996; 20: 731–738.
Rosen HR, O'Reilly PM, Shackleton CR, Christopher R, McDiarmid S, Holt C, et al. Graft loss following liver transplantation in patients with chronic hepatitis C. Transplantation 1996; 62: 1773–1776.
Boker KHW, Dalley G, Bahr MJ, Maschek H, Tillmann HL, Trautwein C, et al. Long-term outcome of hepatitis C virus infection after liver transplantation. Hepatology 1997; 25: 203–210.
Shuhart MC, Bronner MP, Gretch DR, Thomassen LV, Wartelle CF, Tateyama H, et al. Histological and clinical outcome after liver transplantation for hepatitis C. Hepatology 1997; 26: 1646–1652.
Casavilla FA, Rakela J, Kapur S, Irish W, McMichael J, Demetris AJ, et al. Clinical outcome of patients infected with hepatitis C virus infection on survival after primary liver transplantation under tacrolimus. Liver Transplant Surg 1998; 4: 448–454.
Ghobrial RM, Farmer DG, Baquerizo A, Colquhoun S, Rosen HR, Yersiz H, et al. Orthotopic liver transplantation for hepatitis C: outcome, effect of immunosuppression, and causes of retransplantation during an 8-year single-center experience. Ann Surg 1999; 229: 824–833.
Rosen HR, Shackleton CR, Higa L, Gralnek IM, Farmer DA, McDiarmid SV, et al. Use of OKT3 is associated with early and severe recurrence of hepatitis C after liver transplantation. Am J Gastroenterol 1997; 92: 1453–1457.
Collier J, Heathcote J . Hepatitis C viral infection in the immunosuppressed patient. Hepatology 1998; 27: 2–6.
Papatheodoridis GV, Patch D, Dusheiko GM, Burroughs AK . The outcome of hepatitis C virus infection after liver transplantation: is it influenced by the type of immunosuppression? J Hepatol 1999; 30: 731–738.
Prieto M, Berenguer M, Rayon JM, Cordoba J, Arguello L, Carrasco D, et al. High incidence of allograft cirrhosis in hepatitis C virus genotype 1b infection following transplantation: relationship with rejection episodes. Hepatology 1999; 29: 250–256.
Thung SN, Shim K-S, Shieh C, Schwartz M, Theise N, Borcich A, et al. Hepatitis C in liver allografts. Arch Pathol Lab Med 1993; 117: 145–149.
Guerrero RB, Batts KP, Poterucha JJ, Barrett SL, Germer JJ, Wiesner RH, et al. Detection of hepatitis C RNA in liver tissue by reverse-transcriptase polymerase chain reaction: analysis of sequential post-transplant biopsy specimens [abstract]. Mod Pathol 1997; 10: 160A.
Svoboda-Newman SM, Greenson JK, Singleton TP, Sun R, Frank TS . Detection of hepatitis C by RT-PCR in formalin-fixed paraffin-embedded tissue from liver transplant patients. Diag Mol Pathol 1997; 6: 123–129.
Guerrero RB, Batts KP, Germer JJ, Perez RG, Wiesner RH, Persing DH . Reverse transcriptase-polymerase chain reaction fails to detect peripheral-blood hepatitis C RNA in formalin-fixed liver tissue. Liver Transplant Surg 1998; 4: 455–460.
Scheuer PJ, Ashrafzadeh P, Serlock S, Brown D, Dusheiko GM . The pathology of hepatitis C. Hepatology 1992; 15: 567–571.
Dhillon AP, Dusheiko GM . Pathology of hepatitis C virus infection. Histopathology 1995; 26: 297–309.
Ferrell LD, Wright TL, Roberts J, Ascher N, Lake J . Hepatitis C viral infection in liver transplant recipients. Hepatology 1992; 16: 865–876.
Mueller AR, Platz K-P, Berg T, Guckelberger O, Neuhaus R, Hopf U, et al. Association between hepatitis and rejection: upregulation of cytokines and extracellular matrix parameters. Transplant Proc 1997; 29: 2843–2845.
Petrovic LM, Villamil FG, Vierling JM, Makowka L, Geller SA . Comparison of histopathology in acute allograft rejection and recurrent hepatitis C infection after liver transplantation. Liver Transplant Surg 1997; 3: 398–406.
Baiocchi L, Tisone G, Palmieri G, Rapicetta M, Pisani F, Orlando G, et al. Hepatic steatosis: a specific sign of hepatitis C reinfection after liver transplantation. Liver Transplant Surg 1998: 441–447.
Khettry U, Robiou C, Jenkins RL, Loda M, Lewis WD . Recurrent hepatitis C in liver allografts: early histologic indicators. Intern J Surg Pathol 1998; 6: 197–204.
Demetris AJ, Batts KP, Dhillon AP, Ferrell L, Fung J, Geller SA, et al. Banff schema for grading liver allograft rejection: an international consensus document. Hepatology 1997; 25: 658–663.
Scheuer PJ . Classification of chronic viral hepatitis: a need for reassessment. J Hepatol 1991; 13: 372–374.
Afford SC, Hubscher S, Strain AJ, Adams DH, Neuberger JM . Apoptosis in the human liver during allograft rejection and end-stage liver disease. J Pathol 1995; 176: 373–380.
Tannapfel A, Kohlhaw K, Schwarz R, Wenzke M, Kockerling F, Ebelt J, et al. Apoptosis and the expression of Fas and Fas-ligand antigen after orthotopic liver transplantation. Transplant Proc 1998; 30: 2358–2359.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saxena, R., Crawford, J., Navarro, V. et al. Utilization of Acidophil Bodies in the Diagnosis of Recurrent Hepatitis C Infection after Orthotopic Liver Transplantation. Mod Pathol 15, 897–903 (2002). https://doi.org/10.1038/modpathol.3880626
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880626
Keywords
This article is cited by
-
Concurrent increase in mitosis and apoptosis: a histological pattern of hepatic arterial flow abnormalities in post-transplant liver biopsies
Modern Pathology (2012)
-
What is expected from the pathologist in the diagnosis of viral hepatitis?
Virchows Archiv (2011)
-
Viral Diseases of the Liver in Children: Diagnostic and Differential Diagnostic Considerations
Pediatric and Developmental Pathology (2004)