Abstract
The renal outcome of 34 patients with Henoch-Schönlein purpura nephritis was assessed clinically and by grading acute and chronic renal lesions using a system we applied to primary IgA nephropathy. On a median follow-up period of 65 months, hypertension and the serum levels of creatinine and proteinuria at the time of renal biopsy were correlated with renal survival. Acute glomerular lesions including mesangial hypercellularity, endocapillary proliferation, necrosis, cellular crescents, and leukocytes infiltration were observed, respectively, in 41%, 12%, 50%, 29%, and 32% of the cases. Of these, only glomerular necrotizing lesion and cellular crescent were correlated with the renal survival. Chronic renal lesions based on a grading system applied to primary IgA nephropathy and assessing the extent of glomerular sclerosis (glomerular grading), of tubular loss and interstitial fibrosis (tubulointerstitial grading), and of hyaline arteriolosclerosis demonstrated correlation between these lesions, as well as with renal survival. On follow-up, these chronic renal lesions were predictors of subsequent clinical events associated with disease progression, such as impaired renal function, significant proteinuria, and development of hypertension. Despite some limitations related to the relatively small size, this series indicates that distinction of acute and chronic lesions of Henoch-Schonlein purpura nephritis is important for both the prognosis and management of patients.
Similar content being viewed by others
INTRODUCTION
Despite a good deal of clinical and immunologic supporting evidence, the possible link between primary IgA nephropathy and Henoch-Schonlein purpura (HSP) remains controversial, though the pathogenesis in both conditions is obscure (1, 2, 3, 4). Both primary IgA nephropathy and HSP share many clinical and immunologic features, such as an elevated serum IgA levels or detectable IgA-containing circulating immune complexes and, most strikingly, an almost identical renal lesion (3, 5, 6, 7, 8, 9, 10). However, renal disease is clinically isolated in primary IgA nephropathy, whereas in HSP, multisystem manifestations are most common, with skin purpura, arthritis, gastrointestinal complications, and renal involvement at rates varying between 25 to 85% of the patients from the literature (5, 6, 8, 9, 11, 12). Although most patients with HSP nephritis generally have a good prognosis, larger series showed that some of them follow a chronic progressive course and reach end-stage renal failure (3, 9, 11, 12). Contrary to earlier notions, the long-term renal outcome was found to be similar in children and adults, and HSP nephritis may lead to chronic renal failure in children (3, 9, 11, 12, 13).
Although corticosteroids and cytotoxic drugs have been shown to be effective in active renal as well as extrarenal disease in HSP, the significance of such therapy in long-term renal prognosis remains undetermined (6, 7, 8, 9, 10, 11, 12, 13). This study examined HSP patients undergoing renal biopsy for symptomatic renal manifestations, based on the assumption that such patients may be associated with higher risk to develop chronic renal failure and may share with primary IgA nephropathy similar factors in disease progression (3, 9, 11, 13). The aim of this study is to determine whether acute and chronic renal lesions and the grading system used in primary IgA nephropathy are applicable to HSP nephritis and are endowed with predictive value about the renal outcome (14, 15, 16).
MATERIALS AND METHODS
Patient Selection and Clinical Parameters
We reviewed the record of 52 patients with both the diagnosis of IgA nephropathy and purpura or HSP from the 2680 renal biopsy cases in our files from 1984 and on. The selection criteria included the following: (1) a diagnosis of IgA nephropathy based on predominant mesangial IgA-containing immune complexes in immunofluorescent and electron microscopies, excluding patients with diabetes, systemic lupus erythematosus, chronic liver diseases, and renal allograft (14, 15); (2) a nonthrombocytopenic purpura, with or without arthritis or gastrointestinal symptoms; (3) a minimum follow-up of 12 months; and (4) for light microscopy, ≥5 mm of renal cortex, 10 glomeruli, and 3 arterioles. Excluded were three patients who died within 6 months (of septicemia, severe vasculitis, and liver failure), two who underwent repeat biopsy, seven who were lost to follow-up, three who had insufficient biopsy materials, and three with <12 months of follow-up. Finally, 34 patients were studied. The clinical features analyzed included sex, age, serum creatinine, proteinuria, and blood pressure status at the time of renal biopsy. Proteinuria was graded as 1, 2, and 3, respectively, from 0.4 g/day to 1.0 g/day, >1.0 g/day to 3 g/day, and >3 g/day. Significant proteinuria was referred to when this exceeded 1 g/day. The serum creatinine was considered normal for a level <70 umol/L in children and <120 umol/L in adults. Hypertension was defined when diastolic and systolic pressures were respectively equal or >80 and 130 in children and 90 and 140 mm Hg in adults. The same clinical features were recorded during the follow-up period. End-stage renal disease was defined as a patient requiring maintenance dialysis or with a serial serum creatinine >700 umol/L.
Pathology Assessment
The pathology assessment and grading were reported elsewhere (14, 15). In brief, the biopsy sections were independently scored by two of us (PCLC, FMML), and the results were correlated by κ values.
The grading of chronic lesions included a glomerular grading (GG), a tubulointerstitial grading (TIG), and hyaline arteriolosclerosis (HA). In a first step, each glomerulus of a biopsy was classified into one of the five following categories: 0% (absence of sclerosis), 25% (≤25% sclerosis), 50% (26 to 50% sclerosis), 75% (51 to 75% sclerosis), or 100% (76 to 100% sclerosis). In a second step, the mean percentage of sclerosis per glomerulus was calculated and classified as GG1 (for <25% per glomerulus), GG2 (25% to <50% per glomerulus), and GG3 (>50% per glomerulus). The tubular atrophy and interstitial fibrosis in cortex were also estimated in percentages and were graded as TIG1 (when these were absent or <5%), TIG2 (when these were 5% to <50%), and TIG3 (when these were ≥50%). HA was recorded for arteriolar hyaline changes, with or without smooth muscle hyperplasia (14).
The grading of acute glomerular lesions was done according to the following criteria: 1) mesangial hypercellularity with a score of 0, 1, or 2, respectively, for up to three mesangial cells per area, for four to six cells per area, and for seven or more cells per area; 2) endocapillary proliferation scored as absent, involving <50%, or involving >50% of glomeruli; 3) necrosis, assessed by the percentage of glomeruli affected; 4) cellular crescent, assessed by the percentage of glomeruli affected; and 5) leukocyte infiltration that was significant for five or more polymorphonuclears and mononuclears detected (15).
Statistical Analysis
Statistical analysis was performed using the SPSS statistical software for Windows, version 8.0. The Kaplan-Meier univariate analysis for survival functions was used to compare the different histological grades; the significance of these differences was determined by the Breslow test for a P value < .05. Multivariate analysis of the morphologic and clinical parameters was not done because of the small number of patients studied.
RESULTS
Twenty-one patients were female, and 13 were male. The ages ranged from 5 to 74 years, with a mean age of 29; there were 8 pediatric patients (age <15 yr) and 26 adults. The follow-up period ranged from 25 to 147 months, with a median follow-up of 65 months. The period between clinical presentation and the time of renal biopsy ranged from 2 to 71 months, with a median of 7 months. At the time of renal biopsy, all patients (100%) had microscopic hematuria, 11 (32%) had gross hematuria, 31 (91%) patients had proteinuria (>0.3 g/day), 10 (29%) had significant proteinuria (>1 g/day), 5 (15%) had nephrotic range (>3 g/day), 4 (12%) showed a raised serum creatinine level, and 6 (18%) were hypertensive. Fourteen patients were treated with steroids, and 5 of these also received cyclophosphamide or azathioprine. Of the 34 patients, 3 (9%) reached end-stage renal failure at 48, 60, and 60 months, respectively.
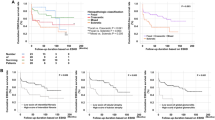
Univariate analysis of the clinical parameters showed that an elevated serum creatinine level, significant proteinuria, and hypertension at presentation were correlated with renal survival and with P values of .0000, .0067, and .0000 (Breslow test), respectively, whereas nephrotic-range proteinuria, gross hematuria, steroids therapy with or without cytotoxic agents, and age and sex of patients were not predictive of the renal outcome (Table 1). The elevated serum creatinine, significant proteinuria, and hypertension at presentation were also predictive of disease progression as reflected by impaired renal function, persistent significant proteinuria, and hypertension on follow-up (Table 1). The renal outcome in this series showed no difference between treated and untreated patients.
For the acute glomerular lesions, mesangial hypercellularity (Fig. 1) was present in 14 (41%), all with four to six cells per mesangial area. Endocapillary proliferation (Fig. 2) was observed in 4 (12%) cases; all were focal and involved <50% of glomeruli. Segmental necrosis (Fig. 3) was seen in 17 (50%) cases, affecting 5 to 39% of glomeruli, with a mean of 18%. Cellular crescents (Figure 4) were identified in 10 (29%) biopsies, affecting 5 to 31% of glomeruli, with a mean of 12%. Leukocyte infiltration was seen in 11 (32%) biopsies. Both necrosis and cellular crescents, but not the other acute glomerular lesions were correlated with renal survival; respectively, these involved P values of .0272 and .0382 (Table 1). However, none of the acute glomerular lesions correlated with the significant clinical events, such as impaired renal function, development of significant proteinuria, and hypertension in this series.
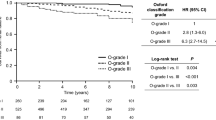
Table 1 also depicts the grading and distribution of the chronic renal lesions. GG1, GG2, and GG3 were observed in, respectively, 26 (76%), 6 (18%), and 2 (6%) patients (Fig. 5). TIG1, TIG2, and TIG3 were seen in 20 (59%), 13 (38%), and 1 (3%) patients. HA was present in 6 (18%) patients. These chronicity-based histological parameters, GG, TIG, and HA, were all statistically correlated with renal survival, and P values of .0257, .0011, and .0382, respectively. On follow-up, GG was predictive of the development of hypertension but not of impaired renal function or significant proteinuria. TIG was predictive of impaired renal function and hypertension but not of proteinuria. The detection of HA was predictive of disease progression associated with impairment of renal function, development of significant proteinuria, and hypertension.
The κ values for the grading system used ranged from 0.834 to 1.0 with a P < .0001 for all histological parameters examined in HSP nephritis and were similar to the results observed in previous studies in primary IgA nephropathy (14, 15).
DISCUSSION
The wide variation in the prevalence of renal involvement in HSP, ranging from 25 to 85% in the literature, may reflect the different approaches to renal manifestations and indications for renal biopsy rather than genuine geographical difference (5, 7, 8, 9, 11, 12). However, it is clear that not all patients with HSP will demonstrate significant renal symptoms or develop nephritis, and it has been suggested that patients with nephritis may have distinctive immunologic markers that set them apart from those without nephritis (4, 7, 12, 17, 18). Despite its much lower prevalence as compared with primary IgA nephropathy, some of the patients with HSP nephritis will unquestionably experience a slowly progressive course and reach end-stage renal failure (3, 7, 8, 9, 11, 13). Many possible factors contributing to disease progression and renal failure in HSP nephritis have been discussed in the literature, but they remain to be established (3, 5, 7, 8, 11, 12, 13). We examined the clinical and morphologic features of HSP patients who underwent biopsy for renal manifestations and assume that these selected patients carry a higher risk of disease progression, similar to that of many patients with primary IgA nephropathy (6, 7, 8, 9, 11, 12, 13). Our objective was to determine whether the histological grading of primary IgA nephropathy can also apply to HSP nephritis and whether the distinction between acute and chronic renal lesions can be predictive of the renal outcome (3, 7, 11, 14).
Of the clinical features examined, the elevated serum creatinine, significant proteinuria, and hypertension at presentation were significantly correlated with the renal outcome, which not only confirms previous observations but also further stresses the similarity between HSP nephritis and primary IgA nephropathy by way of their clinical prognostic features (3, 7, 9, 11, 13, 14, 16, 19). Furthermore, these same clinical features at presentation were also correlated with the risk of disease progression, as determined by the subsequent occurrence of clinical events such as impairment of renal functio and development of significant proteinuria and hypertension on follow-up. Such observations are also similar to those in primary IgA nephropathy (15, 16, 19). Although end-stage renal failure only affected three patients in this series and is in keeping with the observations in the literature, such an infrequent outcome remains to be confirmed by larger series (3, 8, 10, 11, 12, 13). Therefore, features of disease progression such as impaired renal function, proteinuria, or hypertension constitute prognostic indicators of practical importance. Gross hematuria was not associated with an adverse prognosis. Although significant proteinuria at presentation is an adverse risk factor, it is interesting to note that nephrotic range proteinuria subsided in two of the five patients on follow-up, but the prognostic significance of nephrotic range proteinuria needs to be assessed by larger series. Although multivariate analysis and the relative prognostic values of clinical and pathologic factors were not assessed here, it has been suggested that histological parameters are stronger predictors of renal survival than clinical features, which have a tendency to fluctuate (9, 11).
Although the clinical importance of acute renal lesions such as endocapillary proliferation and cellular crescents have been emphasized in HSP nephritis, this semiquantitative series confirmed that such acute lesions not only affect a minority of patients but also constitute a focal disease (3, 8, 11, 12, 13). For example, cellular crescents were detected in 31% of the cases and, when present, affected not more than 31% of the glomeruli or a mean of 12% of glomeruli (3, 8, 9, 11). Moreover, of the acute glomerular lesions examined, only necrosis and cellular crescent were found to carry a prognostic significance and to correlate with an adverse renal outcome. It is possible that therapy may have altered such glomerular lesions and thus the clinical course or disease progression, but no prospective studies have yet been reported to confirm such possibilities (3, 7, 8, 9, 11, 13). Although the renal outcome in this series was not different between treated and untreated patients, such an apparent contradiction may be due to selection and possibly treatment of patients with more severe extrarenal manifestations.
By univariate analysis, all chronic renal lesions in HSP, including GG, TIG, and HA, were predictive of the renal outcome and represent an important prognostic factor, as in primary IgA nephropathy (14, 15, 16, 19). However, multivariate analysis cannot be carried out to assess whether they represent independent variables of renal survival. These chronic lesions were also associated with increased risk of subsequent renal impairment, and with development of significant proteinuria and hypertension. Therefore, in both HSP nephritis and primary IgA nephropathy, glomerular sclerosis, interstitial fibrosis, and hyaline arteriolosclerosis not only are important features predictive of disease progression but also are, in and of themselves, signs of disease progression (14, 15, 16, 19). As already noted, the relatively small cohort did not permit the determination of independent prognostic factors among the clinical and morphologic features and represents a limitation in this study (14). However, we think the grading system showed informative results, the significance of which will be enhanced by longer follow-up of these patients.
From this study, the distinction of acute and chronic renal lesions appears to be a good and useful approach to assess the nephritis of HSP, both for prognosis and management. The detection of acute lesions such as glomerular necrosis and cellular crescent is clinically significant, as these may exacerbate and aggravate the course of nephritis and call for treatment to prevent or to reduce the risk of renal failure (3, 6, 7, 9, 11). Although, there is no specific curative therapy for HSP nephritis, the presence of chronic renal lesions mandates therapy directed toward the control of hypertension and significant proteinuria to limit or slow down disease progression (3, 6, 9, 11, 12, 13, 14). Finally, further therapeutic trials based on this well-defined histological grading system need to be conducted.
References
Meadow SR, Scott DG . Berger disease: Henoch-Schönlein syndrome without the rash. J Pediatr 1985; 106: 27–32.
Silverstein DM, Greifer I, Folkert V, Bennett B, Corey HE, Spitzer A . Sequential occurrence of IgA nephropathy and Henoch-Schonlein purpura: support for common pathogenesis. Pediatr Nephrol 1994; 8: 752–753.
Coppo R, Mazzucco G, Cagnoli L, Lupo A, Schena FP . Long-term prognosis of Henoch-Schonlein nephritis in adults and children. Italian Group of Renal Immunopathology Collaborative Study on Henoch-Schonlein purpura. Nephrol Dial Transplant 1997; 12: 2277–2283.
Liu ZH, Cheng ZH, Yu YS, Tang Z, Li LS . Interleukin-1 receptor antagonist allele: is it a genetic link between Henoch-Schonlein nephritis and IgA nephropathy? Kidney Int 1997; 51: 1938–1942.
Blanco R, Martinez-Taboada VM, Rodriguez-Valverde V, Garcia-Fuentes M, Gonzalez-Gay MA . Henoch-Schonlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum 1997; 40: 859–864.
Niaudet P, Levy M, Broyer M, Habib R . Clinicopathologic correlations in severe forms of Henoch-Schonlein purpura nephritis based on repeat biopsies. Contrib Nephrol 1984; 40: 250–254.
Niaudet P, Murcia I, Beaufils H, Broyer M, Habib R . Primary IgA nephropathies in children: prognosis and treatment. Adv Nephrol Necker Hosp 1993; 22: 121–140.
Habib R, Niaudet P, Levy M . Schonlein-Henoch purpura nephritis and IgA nephropathy. In: Tisher C, Brenner BM, editors. Renal pathology: with clinical and functional correlations. 2nd ed. Philadelphia: Lippincott; 1994. p. 472–523.
Rai A, Nast C, Adler S . Henoch-Schonlein purpura nephritis. J Am Soc Nephrol 1999; 10: 2637–2644.
Coyle JM, Kumwenda MJ, Wright FW . Henoch Schoenlein nephritis. Clin Nephrol 1999; 52: 326–328.
Saulsbury FT . Henoch-Schonlein purpura in children. Report of 100 patients and review of the literature. Medicine 1999; 78: 395–409.
Kaku Y, Nohara K, Honda S . Renal involvement in Henoch-Schonlein purpura: a multivariate analysis of prognostic factors. Kidney Int 1998; 53: 1755–1759.
Scharer K, Krmar R, Querfeld U, Ruder H, Waldherr R, Schaefer F . Clinical outcome of Schonlein-Henoch purpura nephritis in children. Pediatr Nephrol 1999; 13: 816–823.
To KF, Choi PCL, Szeto CC, Li PKT, Tang NLS, Leung CB, et al. Outcome of IgA nephropathy in adults graded by chronic histological lesions. Am J Kidney Dis 2000; 35: 392–400.
Lai FM, Szeto CC, Choi PCL, Li PKT, Chan AWH, Tang NLS, et al. Characterization of early IgA nephropathy. Am J Kidney Dis 2000; 36: 703–708.
Nieuwhof C, Kruytzer M, Frederiks P, van Breda Vriesman PJ . Chronicity index and mesangial IgG deposition are risk factors for hypertension and renal failure in early IgA nephropathy. Am J Kidney Dis 1998; 31: 962–970.
Allen AC, Willis FR, Beattie TJ, Feehally J . Abnormal IgA glycosylation in Henoch-Schonlein purpura restricted to patients with clinical nephritis. Nephrol Dial Transplant 1998; 13: 930–934.
Amoroso A, Danek G, Vatta S, Crovella S, Berrino M, Guarrera S, et al. Polymorphisms in angiotensin-converting enzyme gene and severity of renal disease in Henoch-Schoenlein patients. Italian Group of Renal Immunopathology. Nephrol Dial Transplant 1998; 13: 3184–3188.
D’Amico G . Influence of clinical and histological features on actuarial renal survival in adult patients with idiopathic IgA nephropathy, membranous nephropathy, and membranoproliferative glomerulonephritis: survey of the recent literature. Am J Kidney Dis 1992; 20: 315–323.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Szeto, C., Choi, P., To, K. et al. Grading of Acute and Chronic Renal Lesions in Henoch-Schönlein Purpura. Mod Pathol 14, 635–640 (2001). https://doi.org/10.1038/modpathol.3880364
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880364
Keywords
This article is cited by
-
IgA vasculitis with nephritis: update of pathogenesis with clinical implications
Pediatric Nephrology (2022)
-
Risk factors associated with renal crescentic formation in pediatric Henoch–Schönlein purpura nephritis: a retrospective cohort study
BMC Pediatrics (2020)
-
Updated Oxford classification and the international study of kidney disease in children classification: application in predicting outcome of Henoch-Schönlein purpura nephritis
Diagnostic Pathology (2019)
-
Does MEST-C score predict outcomes in pediatric Henoch-Schönlein purpura nephritis?
Pediatric Nephrology (2019)
-
Presentation of pediatric Henoch–Schönlein purpura nephritis changes with age and renal histology depends on biopsy timing
Pediatric Nephrology (2018)