Abstract
Hematopoietic cell transplantation-associated renal injury may be related to a combination of factors including chemotherapy, radiation, infection, immunosuppressive agents, ischemia, and graft-versus-host disease. Renal biopsy specimens from hematopoietic cell transplant recipients at two institutions (Stanford University Medical Center and Oregon Health & Science University) were reviewed in correlation with clinical data. Fifteen cases were identified (post hematopoietic cell transplant time 0.7–14.5 years), including six with autologous hematopoietic cell transplant. Indications for renal biopsy included proteinuria (n=13; nephrotic range in 8), increased serum creatinine (n=10), or both (n=6). Many patients had multiple pathologic findings on renal biopsy. Membranous glomerulonephritis was the most common diagnosis (n=7), including two patients with autologous hematopoietic cell transplant and five with evidence of chronic graft-versus-host disease elsewhere. Four membranous glomerulonephritis patients achieved sustained remission with rituximab therapy. Other glomerular pathology included focal segmental glomerulosclerosis (n=1) and minimal change disease (n=1). Evidence of thrombotic microangiopathy was common (in isolation or combined with other pathology), as was acute tubular necrosis and tubulointerstitial nephritis. Of 14 patients with follow-up (2–64 months, mean 19 months), 6 had chronic renal insufficiency (serum creatinine >1.5 mg/dl), 2 had end stage renal disease, and 6 had essentially normal renal function. Our retrospective study shows that renal dysfunction in hematopoietic cell transplant recipients is often multifactorial, and biopsy may reveal treatable causes. Membranous glomerulonephritis is seen in autologous and allogeneic hematopoietic cell transplant recipients, and may respond to anti-B-cell therapy, which has implications regarding pathogenesis and relationship to graft-versus-host disease.
Similar content being viewed by others

Main
Hematopoietic cell transplantation is a proven treatment for hematopoietic malignancies, some solid tumors, and other marrow or immune disorders. Hematopoietic cell transplantation protocols are variable and are undergoing continual refinement, including autologous transplantation, peripheral blood stem cell transplantation, and non-myeloablative transplantation, among many others. However, the pathophysiology of and differing susceptibilities to complications, including renal injury, remain elusive. It is suggested that severe acute renal failure is more common in allogeneic bone marrow transplantation as compared to peripheral blood stem cell transplantation, whereas chronic graft-versus-host disease is more common in peripheral blood stem cell transplantation.1, 2, 3
In the acute setting, renal failure may be due to renal toxicity of medications (chemotherapeutic, antibiotic, or immunosuppressive), tumor lysis syndrome, renal ischemia (including hypovolemia, veno-occlusive disease, etc), sepsis, infection (bacterial, fungal, or viral), or effects of radiation.4, 5, 6 A hemolytic-uremia-like syndrome, often referred to as bone marrow transplant nephropathy, may manifest later (3–6 months or post-transplantation later), and classically shows histopathologic features of thrombotic microangiopathy with endothelial injury.4, 5, 6, 7 Although exposure of kidneys to radiation during hematopoietic cell transplantation has been hypothesized as a risk factor for bone marrow transplant nephropathy, studies have shown conflicting data regarding renal shielding and long-term renal insufficiency.5, 8, 9, 10, 11, 12 Other causes of thrombotic microangiopathy must be considered in hematopoietic cell transplant recipients, including exacerbation of endothelial injury by chemotherapy, immune-mediated injury, and perhaps most notably, cyclosporine inhibitor toxicity, given as prophylaxis or treatment for graft-versus-host disease.
Recent studies have provided insight into possible effects of graft-versus-host disease on the kidney. Graft-versus-host disease may occur in the acute (1–3 months post-transplantation), or chronic setting (delayed until 4–12 months post hematopoietic cell transplantation), and most commonly involves skin, liver, and gut; chronic graft-versus-host disease may also manifest features of autoimmune collagen-vascular disease.2, 3, 13 Brukamp et al4 recently summarized evidence suggesting that membranous glomerulonephritis is a glomerular manifestation of chronic graft-versus-host disease.
Other forms of glomerulonephritis have been reported in hematopoietic cell transplantation patients, including minimal change disease, membranoproliferative glomerulonephritis, focal segmental glomerulosclerosis (FSGS), ANCA-associated glomerulonephritis, proliferative glomerulonephritis, and IgA nephropathy.4, 5, 6, 14, 15, 16 Although most studies in the literature have focused on glomerulonephritis in hematopoietic cell transplant recipients, tubulointerstitial and vascular pathology is not uncommon.5 We report the pathologic findings and corresponding clinical data, treatment, and outcome in a series of consecutive renal biopsy specimens in hematopoietic cell transplantation patients from two institutions, including the first cases of membranous glomerulonephritis post autologous stem cell transplantation documented with immunofluorescence and ultrastructural studies.
Materials and methods
Case Selection
The computerized files of the Departments of Pathology at Stanford University Medical Center (SUMC) and Oregon Health & Science University (OHSU) were searched for renal biopsy specimens (1998–2006) in patients with a reported history of bone marrow or peripheral blood stem cell transplantation. The 11 cases from Stanford were derived from 2208 hematopoietic cell transplants performed during this time period (952 allogeneic, 1256 autologous). Clinical history was retrospectively compiled from electronic records, for correlation with pathologic findings. Treatment administered prior to transplantation was not available. Acute renal failure within 3 months of transplantation was defined as increase in serum creatinine 25% over baseline. Diagnosis of chronic graft-versus-host disease was recorded as reported in medical records, derived primarily from clinical findings; biopsy data were available in a subset (Table 1).
Light Microscopic Evaluation
Formalin or Zenker's fixed, paraffin-embedded tissue was sectioned at 2–3 μm, and then the prepared slides were stained with hematoxylin and eosin or periodic acid Schiff (PAS); some had trichrome and Jones Methenamine Silver sections available. On average, 16–32 levels were prepared for light microscopic evaluation. Histopathologic findings were evaluated by two renal pathologists using standard criteria, and tabulated, including evaluation of glomeruli, tubules/interstitium, and vessels.
Immunofluorescence and Electron Microscopy
Frozen sections of tissue transported in Zeus or Michel's medium were stained using standard procedures with directly fluoresceinated antibodies to IgG, IgA, IgM, C3, and C1q. A subset of cases were stained for κ- and λ-light chains, or albumin. Indirect immunofluorescence staining was performed with antisera to fibrinogen.
Tissue for electron microscopic analysis was fixed and processed using standard procedures, including immediate fixation in 1.5% glutaraldehyde/paraformaldehyde in 0.1 M sodium cacodylate buffer, post-fixation in osmium tetroxide, and embedding in plastic resin. Thick sections (1 μm) were stained with toluidine blue, and ultrathin sections were stained with uranyl acetate and lead citrate.
Immunohistochemical Staining
Formalin-fixed, paraffin-embedded tissue was sectioned at 3–4 μm, and stained with polyclonal antiserum to C4d (n=9; Biomedica Gruppe, Austria, distributed by ALPCO, Windham NH) as described previously.17 Staining was attempted on tissue fixed in Zenker's, but results were deemed inconclusive.
Results
Patients and Hematopoietic Cell Transplantation
A total of 15 renal biopsies from 15 patients who had previously undergone hematopoietic cell transplantation were identified. Patient and hematopoietic cell transplant parameters are detailed in Table 1. The underlying disease leading to hematopoietic cell transplantation was a hematolymphoid malignancy in the majority of patients; two women underwent transplantation for stage IV breast carcinoma (Table 1). Patients with allogeneic hematopoietic cell transplants received graft-versus-host disease prophylaxis; nevertheless, clinical evidence of chronic graft-versus-host disease of the gastrointestinal tract, skin, oral mucosa, or lung was documented in eight patients, all but one of the allogeneic transplant recipients (Table 1).
During routine clinical follow-up, renal insufficiency (increased serum creatinine), proteinuria or both was identified, prompting renal biopsy. Renal biopsies were performed 8 months to 14.5 years after hematopoietic cell transplantation (mean=4.17 years; Table 1). Eight patients presented with nephrotic range proteinuria (>3.5 g/day), seven with features of the nephrotic syndrome such as low-serum albumin and edema (Table 1). Ten patients had serum creatinine greater than 1.5 mg/dl, and serum creatinine was greater than 4.0 mg/dl in three of these patients. Thus, six patients had both nephrotic range proteinuria and elevated serum creatinine at presentation (Table 1). At the time of biopsy, all patients were in clinical remission from their primary (pre-hematopoietic cell transplant) disease. Of the patients with chronic graft-versus-host disease, most had ongoing manifestations at the time of renal biopsy.
Renal Biopsy Findings
A variety of renal pathologic lesions were identified, with many biopsies demonstrating multiple histopathologic abnormalities, including membranous glomerulonephritis, FSGS, minimal change disease, thrombotic microangiopathy, acute tubular injury/necrosis, tubulointerstitial nephritis, calcineurin inhibitor toxicity, and arteriolar hyalinosis (Table 2), described in detail below. In our series, none of the biopsies showed evidence of pathology attributable to recurrent disease, including manifestations of excess light chains.
Nearly half of the biopsies in the study cohort demonstrated membranous glomerulonephritis (cases 1–7, Table 2, Figure 1a and c), including all seven patients with full nephrotic syndrome. Classic pathologic features of membranous glomerulonephritis were seen, including thickening of the glomerular basement membrane at the level of light microscopy, and granular capillary loop IgG and/or C3 deposits on immunofluorescence analysis. The subepithelial deposits were highlighted by immunohistochemical staining for C4d, but no C4d staining was detected in peritubular capillaries in cases of membranous glomerulonephritis (Table 2). Characteristic subepithelial electron dense deposits were seen in every case on ultrastructural analysis (Figure 1, Table 2). All five allogeneic hematopoietic cell transplant recipients with membranous glomerulonephritis had clinical evidence of chronic graft-versus-host disease. Interestingly, two patients with membranous glomerulonephritis had received an autologous transplant.
(a) Membranous glomerulonephritis with mesangial proliferation (case 6); the inset shows subepithelial electron dense deposits by electron microscopy. (b) Acute tubular injury and tubulointerstitial nephritis (case 6; arrows: eosinophils, interstitial neutrophils are also seen); the inset shows proximal tubular epithelial cell mitotic figures and simplification with reactive nuclei. (c) Autologous hematopoietic cell transplantation, with membranous glomerulonephritis and endothelial cell injury (case 2), seen as a capillary microaneurysm containing foam cells (arrows), fragmented red blood cells, and delicate fibrin strands (arrowheads). (d) Focal segmental glomerulosclerosis (FSGS, case 8); arterioles demonstrate medial muscular hypertrophy and/or hyalinosis. (e) Thrombotic microangiopathy (case 10), including diffuse endothelial cell swelling and abundant karyorrhectic debris. (f) Features of chronic thrombotic microangiopathy (case 10), including reduplication of glomerular basement membranes and afferent arteriolar basement membrane. Arteriolar hyalinosis is prominently seen (left, arrows) as well as interstitial calcification (upper right, arrowheads) (a, d and f—PAS; b, c and e—H&E; original magnifications light microscopy × 400; electron microscopy × 6000).
Within the membranous glomerulonephritis cohort, many biopsies demonstrated other concurrent pathologic lesions (Table 2). Case 2 showed one glomerulus with a microaneurysm containing fibrin, red blood cells, including fragmented red blood cells, and foam cells, evidence of endothelial injury (Figure 1c). Concomitant acute tubular injury/necrosis was seen in four cases, with interstitial inflammation (tubulointerstitial nephritis) in two of these. For example, patient 6 had active interstitial nephritis along with marked acute tubular injury, including tubular mitotic figures and vacuolization of tubular epithelial cells (Figure 1b). Features of calcineurin inhibitor toxicity were also seen in case 3 (described below).
FSGS and minimal change disease were seen in one case each. Case 8 showed FSGS, with segmental sclerosis in three glomeruli (Figure 1d), one with endocapillary foam cells. Further, endothelial injury and mesangiolysis was seen, along with severe arteriolar hyalinosis (no calcineurin inhibitor exposure or diabetes mellitus, although the patient was hypertensive, see hyalinosis below). Biopsy 9 revealed diffuse podocyte foot process effacement by electron microscopy, consistent with minimal change disease. Additionally, subendothelial neo-basement membrane formation suggested prior endothelial injury; this, together with mesangiolysis was suggestive of prior thrombotic microangiopathic injury.
Cases 10 and 11 also showed histologic features of endothelial injury/thrombotic microangiopathy (Table 2). The biopsy from patient 10 showed dramatic histologic findings (Figure 1e and f), with four glomeruli containing capillary luminal fibrin, karyorrhectic debris, and endothelial cell swelling. Further, glomerular basement membrane reduplication was seen in several loops, indicative of chronicity. Evidence of vascular thrombi or vasculitis was not seen. However, arterioles demonstrated intimal mucoid edema along with prominent intimal and medial hyaline, resulting in near occlusion of some sampled arterioles; arteries were involved to a lesser degree. This patient had recently started calcineurin inhibitor therapy, and was diabetic. Case 11 showed mesangiolysis, with focal double contouring of glomerular basement membranes on light microscopy, whereas ultrastructural studies showed segmental separation of endothelium from glomerular basement membrane, and fibrin tactoids present within a microaneurysm. Once again, severe arteriolar hyalinosis was present, though there was no calcineurin inhibitor exposure in this patient (autologous transplant). None of the patients with histological features of thrombotic microangiopathy had malignant hypertension, systemic features of hemolytic uremia syndrome or thrombotic thrombocytopenic purpura (TTP), or schistocytes on blood smear. C4d immunohistochemical staining was negative in these biopsies as well (Table 2).
Renal biopsy specimens from nine patients showed evidence of acute tubular injury/necrosis or tubulointerstitial nephritis, including four patients with concomitant membranous glomerulonephritis, as described above (Table 2). The diagnosis of acute tubular injury/necrosis was based on findings of ectatic tubules, with loss of brush border and simplification of tubular epithelial cells. Reactive–regenerative nuclear atypia and tubular mitotic figures were also noted in most specimens. Biopsies with tubulointerstitial nephritis demonstrated sparse interstitial inflammatory cell infiltrates in non-atrophic areas of cortex, comprised predominantly of lymphocytes, some with accompanying eosinophils, neutrophils, and/or plasma cells. Tubulitis was frequently identified; and edema was variably present (Figure 1b). Cases with evidence of active tubulointerstitial nephritis generally also showed a greater degree of tubular atrophy and interstitial fibrosis, consistent with chronicity (Table 2). None of the patients except case 15 had interstitial or tubular basement membrane deposits by immunofluorescence or electron microscopy. Although medication histories are incomplete, possible association with medications was derived in only three patients (case 4 past history of ibuprofen use; case 13 herbal treatment, and case 14 exposure to several anti-fungal agents).
Tubular epithelial cell nuclear atypia was seen in biopsy 12 but there was no evidence of BK polyoma virus by electron microscopic or immunohistochemical analysis (serum PCR titer peak 130 000 copies/ml 10 weeks post-biopsy). Interestingly, patient 15 had hemorrhagic cystitis with PCR documented urine JC virus, treated with cidofovir (1 mg/kg, with concomitant cyclosporine 100 mg twice a day) 6 months prior to biopsy. At the time of biopsy, there was no evidence of viral cytopathy, but significant tubular atrophy and interstitial fibrosis was seen, with a sparse lymphocytic infiltrate and occasional tubulitis.
Of the six patients with documented exposure to calcineurin inhibitors, two biopsies (cases 3 and 10) showed findings compatible with calcineurin inhibitor toxicity. In case 3, there was arteriolar hyalinosis, and a ‘striped’ pattern of interstitial fibrosis and tubular atrophy, with clinical suspicion of calcineurin inhibitor toxicity (serum drug levels not available). Biopsies from six patients demonstrated arteriolar hyaline; only three of these had exposure to calcineurin inhibitor (Tables 1, 2), whereas one was diabetic (case 10) and two others were hypertensive (cases 8 and 10).
Endothelial cell tubuloreticular inclusions were identified on electron microscopy in biopsies 7 and 13. In terms of known associations with tubuloreticular inclusions, case 7 had positive anti-nuclear antibody (ANA) and rheumatoid factor, but no known symptoms of systemic lupus erythematosus, and each patient and donor had tested negative for HIV prior to transplantation. Other than both receiving peripheral blood stem cell transplantation, common features of hematopoietic cell transplantation or subsequent clinical course were not identified in these two patients.
Treatment and Outcome
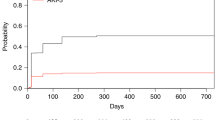
At least five of seven patients with membranous glomerulonephritis were treated with immunosuppressive therapy (Table 1). One patient (case 6) had a slow response to prednisone and mycophenolate mofetil, with proteinuria normalization after 5 months, and remission sustained for at least 4 years. Four patients were treated with rituximab (anti-CD20) as initial therapy (cases 2 and 7) or as second-line therapy (cases 4 and 5) due to lack of improvement with prednisone +/− mycophenolate mofetil. Complete and sustained remission was attained in each rituximab treated patient, including the autologous hematopoietic cell transplantation recipient (patient 2; Tables 1, 2). Treatment data are unavailable for one membranous glomerulonephritis patient, and another (case 3) presented with extensive chronic damage and rapidly progressed to dialysis without institution of any therapy, and died 38 months later.
Among the patients with non-membranous glomerulonephritis, three patients were treated with immunosuppressive therapy (Table 1). The patient with FSGS (case 8) was treated with prednisone and mycophenolate mofetil, and had progressively increasing serum creatinine and paradoxical resolution of proteinuria (Table 1). Patient 9 (minimal change disease, clinical Sjögren's with positive anti-Ro/SSA and anti-La/SSB, ANA of 1:320 and negative anti-ds DNA) was treated with steroids and mycophenolate mofetil with rapid improvement of proteinuria and renal function, as well as resolution of rash. Of patients with acute tubular injury/necrosis and/or tubulointerstitial nephritis, renal function improved with decadron and plasmapheresis in one (case 14), whereas discontinuation of an herbal agent correlated with decreased serum creatinine in another (case 13). The remainder of the patients had no record of specific treatment, and had progressively increasing serum creatinine.
Discussion
Previous studies in the literature have focused primarily on biopsies from hematopoietic cell transplantation patients presenting with nephrotic syndrome, or on clinical studies of patients with chronic kidney disease with little correlative biopsy data. We studied a series of consecutive renal biopsies in hematopoietic cell transplant recipients from two institutions, encompassing patients with nephrotic and non-nephrotic presentation, including a number of patients with autologous hematopoietic cell transplantation.
Our study confirms and extends previous reports of membranous glomerulonephritis in allogeneic hematopoietic cell transplantation patients, adding 7 additional cases to the 50 cases previously reported in the literature.4, 5, 6, 14, 15, 16, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29 In our series, among seven patients with membranous glomerulonephritis, all five patients with allogeneic transplants had evidence of chronic graft-versus-host disease, (in the non-membranous glomerulonephritis cohort, only three out of eight patients had chronic graft-versus-host disease). Importantly, we also present two patients with biopsy proven membranous glomerulonephritis after autologous hematopoietic cell transplantation.
Current evidence has led to the suggestion that membranous glomerulonephritis is a glomerular manifestation of chronic graft-versus-host disease; this notion is primarily based on temporal relationship between cessation of immunosuppressive therapy, manifestation of renal symptoms, and association with chronic graft-versus-host disease in other organs.4 Paradoxically, idiopathic membranous glomerulonephritis is considered to be the result of autoantibodies,30, 31 whereas graft-versus-host disease had historically been attributed primarily to T cells.2, 3, 32, 33 However, a role for B cells and antibodies in chronic graft-versus-host disease is being increasingly recognized. Chronic graft-versus-host disease shares clinical manifestations with various autoimmune diseases, and anti-nuclear antibodies are often demonstrable.34 Studies have demonstrated a correlation of chronic graft-versus-host disease with antibodies to Y-chromosome encoded minor histocompatibility antigens, called H-Y antigens, in male hematopoietic cell transplant recipients with female donors.35 Others demonstrated the development of anti-nephrin autoantibodies and mesangioproliferative glomerulonephritis in a mouse model of chronic graft-versus-host disease after non-myeloablative transplantation.36
Small studies have separately characterized efficacy of the anti-CD20 agent rituximab in treatment of chronic graft-versus-host disease,37 and idiopathic membranous glomerulonephritis.38, 39, 40, 41 Thus, it is not unexpected that rituximab-treated hematopoietic cell transplantation recipients with biopsy proven membranous glomerulonephritis responded well (three allogeneic and one autologous transplant). Although other reports have demonstrated treatment response with rituximab in hematopoietic cell transplantation patients with membranous glomerulonephritis/nephrotic syndrome, many previously reported patients had only partial remission, and in one case a biopsy was not performed.4, 6, 22, 29 Nevertheless, resolution of graft-versus-host disease and post hematopoietic cell transplant membranous glomerulonephritis with this anti-B-cell agent supports the hypothesis that B-cell alloreactivity may play a role in both of these entities.16, 35, 37
Interestingly, our study also identified two patients with biopsy proven membranous glomerulonephritis after autologous hematopoietic cell transplantation. As these patients have not received foreign cells, classic graft-versus-host disease is, by definition, not possible. Although we cannot entirely rule out the possibility of coincident occurrence of two increasingly common problems: hematopoietic cell transplantation and membranous glomerulonephritis; it is proposed that immune dysregulation attributable to exposure to chemical, antibiotic, and radiologic manipulation can result in graft-versus-host disease-like manifestations. Although none of the autologous transplant patients in our study showed such symptoms (Table 1), a syndrome with clinical and biopsy findings similar to graft-versus-host disease affecting skin, gastrointestinal tract, and liver, has been described in few patients who have undergone autologous hematopoietic cell transplantation.42, 43, 44, 45, 46 This syndrome may be preferentially associated with immune manipulation such as cyclosporine, interferon, or alemtuzumab treatment during and after transplantation, and current hypotheses include auto-effector T cells recognizing MHC class II antigens.42, 43, 44, 45 Notably, we report one patient with membranous glomerulonephritis post autologous transplantation treated with rituximab who achieved complete renal remission, again suggesting a role for B cells.
Chronic kidney disease occurs less often in recipients of autologous as compared to allogeneic hematopoietic cell transplantation;12 however, renal pathology has been little studied in this setting. Our study highlights the renal biopsy pathology in autologous hematopoietic cell transplantation. In addition to the two patients with membranous glomerulonephritis, we also report one patient with minimal change disease, one with chronic thrombotic microangiopathy, and two with acute tubular injury/necrosis-tubulointerstitial nephritis. Like membranous glomerulonephritis, minimal change disease may be associated with graft-versus-host disease-like autoimmunity, and T-cell alloreactivity has been hypothesized as a cause of minimal change disease.5, 47 Indeed, the patient with minimal change disease had a positive ANA, other autoimmune manifestations, and responded to immunosuppressive therapy. Chang et al18 described six autologous hematopoietic cell transplant recipients in their case series, and found thrombotic microangiopathy, polyoma virus nephropathy, tubulointerstitial nephritis, and recurrent amyloidosis, but no other glomerular pathology. Other individual case reports post autologous hematopoietic cell transplantation in the renal literature include type I membranoproliferative glomerulonephritis,48 mesangial proliferative glomerulonephritis,49 and endothelial injury.50 Interestingly, a patient with TTP achieved remission with rituximab therapy (no renal biopsy performed).51 An autopsy series also reported membranous glomerulonephritis in a patient 7 months after autologous transplantation for breast carcinoma; however, special stains, electron microscopic, and immunofluorescence studies were not performed.52
Hematopoietic cell transplantation patients have exposure to many factors known to contribute to endothelial injury including radiation, chemotherapy, pathogens, sepsis, immune dysregulation, and calcineurin inhibitors.5, 51, 53 None of our thrombotic microangiopathy patients had either malignant hypertension or evidence of metastatic carcinoma at the time of biopsy; only one thrombotic microangiopathy patient (case 10) had reported exposure to calcineurin inhibitor. Several thrombotic microangiopathy patients also had marked arteriolar hyalinosis on biopsy. Although hyalinosis is not one of the common pathognomonic features of thrombotic microangiopathy, it is perhaps the result of insudative lesions at prior sites of thrombosis;54 alternatively, these findings may be coincidental. No trends were discernible in terms of primary disease, peripheral blood vs bone marrow-derived stem cells, autologous or allogeneic transplant, exposure to radiation, calcineurin inhibitors, or intensity of chemotherapeutic conditioning regimen among our small number of patients with thrombotic microangiopathy or endothelial injury (cases 2, 8–11).
Polyoma virus cystitis and nephritis is a known complication post hematopoietic cell transplantation.5, 15, 18 In our series, one patient (case 15) had mild renal insufficiency prior to intermediate dose cidofovir treatment for JC viral cystitis. Treatment correlated with acute increase in serum creatinine, leading to ESRD. Case reports have documented cidofovir-induced end stage renal failure, most commonly in HIV patients treated with high-dose cidofovir (5 mg/kg per dose), and in patients with elevated pretreatment serum creatinine.55, 56, 57
In conclusion, renal dysfunction late after hematopoietic cell transplantation has a wide spectrum of etiologies and possible pathogenesis. Renal biopsy is helpful in elucidating the nature of the renal insult, and identifying potentially treatable disease processes. Multiple pathologies are frequently seen, and correlation with clinical history including primary disease, type of transplant, immunosuppressive, and other medications is important. This series suggests that a subset of patients could benefit from anti-B-cell targeted therapy.
References
Schrier RW, Parikh CR . Comparison of renal injury in myeloablative autologous, myeloablative allogeneic and non-myeloablative allogeneic haematopoietic cell transplantation. Nephrol Dial Transplant 2005;20:678–683.
Baird K, Pavletic SZ . Chronic graft versus host disease. Curr Opin Hematol 2006;13:426–435.
Cutler C, Antin JH . Chronic graft-versus-host disease. Curr Opin Oncol 2006;18:126–131.
Brukamp K, Doyle A, Bloom R, et al. Nephrotic syndrome after hematopoietic cell transplantation: do glomerular lesions represent renal graft versus host disease. Clin J Am Soc Nephrol 2006;1:685–694.
Hingorani S . Chronic kidney disease in long-term survivors of hematopoietic cell transplantation: epidemiology, pathogenesis, and treatment. J Am Soc Nephrol 2006;17:1995–2005.
Rao PS . Nephrotic syndrome in patients with peripheral blood stem cell transplant. Am J Kidney Dis 2005;45:780–785.
Ho V, Cutler C, Carter S, et al. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2005;11:571–575.
Weiss AS, Sandmaier BM, Storer B, et al. Chronic kidney disease following non-myeloablative hematopoietic cell transplantation. Am J Transplant 2006;6:89–94.
Frisk P, Bratteby LE, Carlson K, et al. Renal function after autologous bone marrow transplantation in children: a long-term prospective study. Bone Marrow Transplant 2002;29:129–136.
Miralbell R, Bieri S, Mermillod B, et al. Renal toxicity after allogeneic bone marrow transplantation: the combined effects of total-body irradiation and graft-versus-host disease. J Clin Oncol 1996;14:579–585.
Lawton CA, Cohen EP, Murray KJ, et al. Long-term results of selective renal shielding in patients undergoing total body irradiation in preparation for bone marrow transplantation. Bone Marrow Transplant 1997;20:1069–1074.
Hingorani S, Guthrie KA, Schoch G, et al. Chronic kidney disease in long-term survivors of hematopoeitic cell transplant. Bone Marrow Transplant 2007;39:223–229.
Gilman A, Serody J . Diagnosis and treatment of chronic graft-versus-host disease. Semin Hematol 2006;43:70–80.
Colombo AA, Rusconi C, Esposito C, et al. Nephrotic syndrome after allogeneic hematopoietic stem cell transplantation as a late complication of chronic graft-versus-host disease. Transplantation 2006;81:1087–1092.
Stevenson WS, Nankivell BJ, Hertzberg MS . Nephrotic syndrome after stem cell transplantation. Clin Transplant 2005;19:141–144.
Reddy P, Johnson K, Uberti JP, et al. Nephrotic syndrome associated with chronic graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2006;38:351–357.
Troxell ML, Sibley R, Higgins J, et al. Comparison of C4d immunostaining methods in renal allograft biopsies. Clin J Am Soc Nephrol 2006;1:583–591.
Chang A, Hingorani S, Kowalewska J, et al. Spectrum of renal pathology in hematopoietic cell transplantation: a series of 20 patients and review of literature. Clin J Am Soc Nephrol 2007;2:1014–1023.
Lam MF, Tse KC, Chan G, et al. De novo glomerulonephritis after hematopoietic stem cell transplantation. J Am Soc Nephrol 2006;17:733A.
Chan GS-W, Chim S, Fan YS, et al. Focal segmental glomerulosclerosis after membranous glomerulonephritis in remission: temporal diversity of glomerulopathy after bone marrow transplantation. Hum Pathol 2006;37:1607–1610.
Romagnani P, Lazzeri E, Mazzinghi B, et al. Nephrotic syndrome and renal failure after allogeneic stem cell transplantation: novel molecular diagnostic tools for a challenging differential diagnosis. Am J Kidney Dis 2005;46:550–556.
Srinivasan R, Balow JE, Sabnis S, et al. Nephrotic syndrome: an under-recognised immune-mediated complication of non-myeloablative allogeneic haematopoietic cell transplantation. Br J Haematol 2005;131:74–79.
Akar H, Keven K, Celebi H, et al. Nephrotic syndrome after allogeneic peripheral blood stem cell transplantation. J Nephrol 2002;15:79–82.
Lin J, Markowitz GS, Nicolaides M, et al. Membranous glomerulopathy associated with graft-versus-host disease following allogeneic stem cell transplantation. Report of 2 cases and review of the literature. Am J Nephrol 2001;21:351–356.
Rossi L, Cardarelli F, Vampa ML, et al. Membranous glomerulonephritis after haematopoietic cell transplantation for multiple myeloma. Nephron 2001;88:260–263.
Nergizoglu G, Keven K, Ates K, et al. Chronic graft-versus-host disease complicated by membranous glomerulonephritis. Nephrol Dial Transplant 1999;14:2461–2463.
Oliveira JSR, Bahia D, Franco M, et al. Nephrotic syndrome as a clinical manifestation of graft-versus-host disease (GVHD) in a marrow transplant recipient after cyclosporine withdrawal. Bone Marrow Transplant 1999;23:99–101.
Yorioka N, Taniguchi Y, Shimote K, et al. Membranous nephropathy with chronic graft-versus-host disease in a bone marrow transplant recipient. Nephron 1998;80:371–372.
Terrier B, Delmas Y, Hummel A, et al. Post-allogeneic haematopoietic stem cell transplantation membranous nephropathy: clinical presentation, outcome and pathogenic aspects. Nephrol Dial Transplant 2007;22:1369–1376.
Kerjaschki D . Molecular pathogenesis of membranous nephropathy. Kidney Int 1992;41:1090–1105.
Debiec H, Guigonis V, Mougenot B, et al. Antenatal membranous glomerulonephritis due to anti-neutral endopeptidase antibodies. N Engl J Med 2002;346:2053–2060.
Copelan EA . Hematopoietic stem-cell transplantation. N Engl J Med 2006;354:1813–1826.
Lee SJ . New approaches for preventing and treating chronic graft-versus-host-disease. Blood 2005;105:4200–4206.
Perruche S, Kleinclauss F, Tiberghien P, et al. B Cell allogeneic responses after hematopoietic cell transplantation: is it time to address this issue? Transplantation 2005;79:S37–S39.
Miklos DB, Kim HT, Miller KH, et al. Antibody responses to H-Y minor histocompatibility antigens correlate with chronic graft-versus-host disease remission. Blood 2005;105:2973–2978.
Nagahama K, Maru K, Kanzaki S, et al. Possible role of autoantibodies against nephrin in an experimental model of chronic graft-versus-host disease. Clin Exp Immunol 2005;141:215–222.
Cutler C, Miklos DB, Kim HT, et al. Rituximab for steroid-refractory chronic graft-versus-host disease. Blood 2006;108:756–762.
Ruggenenti P, Chiurchiu C, Abbate M, et al. Rituximab for idiopathic membranous nephropathy: who can benefit. Clin J Am Soc Nephrol 2006;1:738–748.
Jacobson SH, van Vollenhoven R, Gunnarsson I . Rituximab-induced long-term remission of membranous lupus nephritis. Nephrol Dial Transplant 2006;21:1742–1743.
Ruggenenti P, Chiurchiu C, Brusegan V, et al. Rituximab in idiopathic membranous nephropathy: a one-year prospective study. J Am Soc Nephrol 2003;14:1851–1857.
Remuzzi G, Chiurchiu C, Abbate M, et al. Rituximab for idiopathic membranous nephropathy. Lancet 2002;360:923–924.
Cheney RT, Sprent J . Capacity of cyclosporine to induce auto-graft-versus-host disease and impair intrathymic T cell differentiation. Transplant Proc 1985;17:528–531.
Zenz T, Ritgen M, Dreger P, et al. Autologous graft-versus-host disease-like syndrome after an alemtuzumab-containing conditioning regimen and autologous stem cell transplantation for chronic lymphocytic leukemia. Blood 2006;108:2127–2130.
Kline J, van Besien K, Nathanson J, et al. Severe intestinal graft-versus-host disease following autologous stem cell transplantation. Bone Marrow Transplant 2006;38:391–392.
Holmberg L, Kikuchi K, Gooley TA, et al. Gastrointestinal graft versus host disease in recipients of autologous hematopoietic stem cells: Incidence, risk factors and outcome. Biol Blood Marrow Transplant 2006;12:226–234.
Saunders MD, Shulman HM, Murakami CS, et al. Bile duct apoptosis and cholestasis resembling acute graft-versus-host disease after autologous hematopoietic cell transplantation. Am J Surg Pathol 2000;24:1004–1008.
Sato Y, Hara S, Fujimoto S, et al. Minimal change nephrotic syndrome after allogenic hematopoietic stem cell transplantation. Intern Med 2004;43:512–515.
Sakarcan A, Neuberg RW, McRedmond KP, et al. Membranoproliferative glomerulonephritis develops in a child with autologous stem cell transplant. Am J Kidney Dis 2002;40:E19.
Forslund T, Anttinen J, Hallman H, et al. Mesangial proliferative glomerulonephritis after autologous stem cell transplantation. Am J Kidney Dis 2006;48:314–320.
Takeuchi M, Tamaoki A, Tada A, et al. Crescentic glomerulonephritis developing 3 months after autologous peripheral blood stem cell transplantation for non-Hodgkin's lymphoma. Bone Marrow Transplant 1998;22:725–727.
Gallerani E, Lerch E, Romagnani E, et al. Thrombotic thrombocytopenic purpura associated with renal failure after autologous transplantation for multiple myeloma successfully treated for rituximab. Eur J Haematol 2006;77:527–529.
El-Seisi S, Gupta R, Clase CM, et al. Renal pathology at autopsy in patients who died after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2003;9:683–688.
Chan GS-W, Lam M-F, Au WY, et al. Renal impairment after bone marrow transplantation. Arch Pathol Lab Med 2004;128:233–234.
Lasik ZG, Silva FG . Hemolytic uremia syndrome, thrombotic thrombocytopenic purpura, and other thrombotic microangiopathies. In: Jeannette JC, Olson JL, Schwartz MM, Silva FG (eds). Heptinstall's Pathology of the Kidney, 6th edn. Lippincott Williams & Wilkins: Philadelphia, 2007, pp 715–723.
Meier P, Dautheville-Guibal S, Ronco PM, et al. Cidofovir-induced end-stage renal failure. Nephrol Dial Transplant 2002;17:148–149.
Kay TD, Hogan PG, McLeod SE, et al. Severe irreversible proximal tubular acidosis and azotaemia secondary to cidofovir. Nephron 2000;86:348–349.
Ljungman P, Ribaud P, Eyrich M, et al. Cidofovir for adenovirus infectious after allogeneic hematopoietic stem cell transplantation: a survey by the infectious diseases working party of the European group for blood and marrow transplantation. Bone Marrow Transplant 2003;31:481–486.
Acknowledgements
This study was presented in abstract form at the United States and Canadian Academy of Pathology Meeting March 27, 2007, San Diego, CA, USA. We are grateful to referring clinicians for helpful clinical correlation and follow-up. We acknowledge the expert technical assistance of Linda Anderson, Palmira Makeef, and Anita Reynon (SUMC Pathology), and Donald Andersen, Gayle Countryman, Dornald Myles, Cary Brady, Kay Larkin and Elizabeth Geltz (OHSU Pathology).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Troxell, M., Pilapil, M., Miklos, D. et al. Renal pathology in hematopoietic cell transplantation recipients. Mod Pathol 21, 396–406 (2008). https://doi.org/10.1038/modpathol.3801011
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3801011
Keywords
This article is cited by
-
Pathological evaluation of renal complications in children following allogeneic hematopoietic stem cell transplantation: a retrospective cohort study
BMC Pediatrics (2023)
-
Renal pathology in hematopoietic cell transplant recipients: a contemporary biopsy, nephrectomy, and autopsy series
Modern Pathology (2016)
-
Chronic kidney disease after autologous stem cell transplantation: analysis of a single center experience
International Urology and Nephrology (2014)
-
Glomerular diseases seen with cancer and chemotherapy: a narrative review
Kidney International (2013)
-
A case of membranous nephropathy associated with chronic GVHD successfully treated with rituximab
Bone Marrow Transplantation (2012)