Abstract
The clinicopathological significance of loss of heterozygosity (LOH) in gastric carcinoma remains poorly understood. We and other researchers have previously demonstrated that LOH is fairly common in intestinal- and solid-type gastric carcinomas, but rare in diffuse-type tumors. In this study, we investigated the relationship between clinicopathological variables and LOH status in intestinal- and solid-type gastric carcinomas. The crypt isolation technique was utilized to analyze LOH at 1p36, 3p14, 4p15, 5q21–22, 8p11–12, 9p21, 13q22, 17p13.1 18q21 and 22q13.31 in 113 intestinal- and solid-type gastric carcinomas using a polymerase chain reaction assay. Immunostaining with D2–40 and Elastica van Gieson staining were used to detect lymphatic invasion and vessel invasion, respectively. High LOH rates (49–71%) were observed in all chromosomal regions tested. 1p36 loss was significantly associated with advanced tumors and lymph node metastasis. 8p11–12 loss was significantly associated with lymph node metastasis, lymphatic invasion, and vessel invasion. 17p13.1 (TP53) loss was significantly associated with vessel invasion. 22q13.31 loss was significantly associated with advanced tumors, lymph node metastasis, lymphatic invasion, vessel invasion and late TNM stage. No significant associations were observed between LOH at other chromosomal regions and aggressive behaviors. In addition, significantly higher LOH rates at 1p36, 9p21, 18q21 and 22q13.31 were observed in cardiac tumors compared with noncardiac tumors. These results suggest that in intestinal- and solid-type gastric carcinomas, LOH on 3p14, 4p15, 5q21–22, 9p21, 13q22 and 18q21 is associated with carcinogenesis, while LOH on 1p36, 8p11–12, 17p31.1 and 22q13.31 is associated with tumor progression.
Similar content being viewed by others
Main
Gastric adenocarcinoma is still one of the most common cancers and a leading cause of cancer death in the world. Although multiple genetic and epigenetic alterations, such as mutations of the p53 and E-cadherin genes, loss of heterozygosity (LOH), DNA methylation and microsatellite instability (MSI), have been described in gastric carcinomas, the significance of these alterations with respect to the carcinogenesis or progression of gastric carcinomas remains largely unclear.1, 2
LOH studies in gastric cancer have discovered several chromosomal regions with significant allelic loss, suggesting that these regions harbor several candidate or putative tumor suppressor genes important in the development of gastric cancer.3, 4 To date, several studies have attempted to investigate the relationship between various clinicopathological characteristics or outcomes and LOH status in gastric carcinoma.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 However, these studies substantially disagree among themselves with regard to the frequency of LOH, and the relationships between LOH and various clinicopathological factors or outcomes remain controversial. Some of these studies have focused on the relationship between clinicopathological factors and the extent of chromosomal loss (fractional allelic loss (FAL)).9, 10, 13, 14 Most studies investigating the relationship between single chromosomal loss and clinicopathological variables have only evaluated tumor stage (depth of invasion).5, 6, 8, 11 Therefore, the clinicopathological significance of LOH, especially single chromosomal region loss, with respect to the initiation and progression of gastric carcinoma remains poorly understood.
In previous studies, one inevitable limitation of LOH analysis using conventional isolation methods is that the preparations of tumor DNA are always contaminated with normal DNA, making it difficult to accurately assess LOH status due to the increased likelihood of false-negative results with respect to allelic losses.3, 4 To date, only two reports have reported a significantly higher LOH rate (>50%) at multiple chromosomes in primary gastric carcinomas: one study used the crypt isolation technique,3 and the other used xenografted gastric carcinomas.4 In addition, some of these previous studies examined a relatively small number of samples and relatively few early cancers, which may also have limited analysis of the relationship between LOH status and clinicopathological factors.5, 14
Moreover, two main histological gastric carcinoma types, intestinal and diffuse, appear to be associated with different genetic pathways.6, 16, 17 Many studies have demonstrated that LOH is fairly common in intestinal type gastric cancer but rare in diffuse type tumors.3, 6, 8, 10, 12, 17 These findings suggest that diffuse type tumor is a separate entity from intestinal gastric carcinoma with its own initiation and progression mechanisms. The Japanese classification of gastric adenocarcinoma divides poorly differentiated adenocarcinomas into solid-type and non-solid-type subgroups.18 Solid-type gastric carcinoma, which shows solid, sheet-like proliferation with an alveolar pattern with indistinct or no tubular differentiation and has a well-defined boundary, shows clearly different histologic appearance and growth pattern compared with intestinal (glandular formation) type and diffuse (non-solid, clustered or single cells with diffuse infiltration) type cancers. By applying the crypt isolation technique, which can isolate normal or tumor crypts from the mucosa propria and separate tumor tissue from stromal tissue, and thus enable us to obtain pure normal epithelium and tumor tissues,3, 19, 20, 21 we recently demonstrated a significantly higher LOH frequency in several chromosomal regions in solid-type gastric adenocarcinomas as well as in intestinal-type tumors, suggesting that LOH may also contribute to carcinogenesis and progression in solid-type tumors.3
In the present study, therefore, we utilized the crypt isolation technique to comprehensively analyze the relationship between clinicopathological variables and LOH status in a large number of intestinal- and solid-type gastric carcinomas.
Materials and methods
Patients
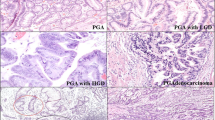
Between March 2000 and February 2005, 113 intestinal- (n=83) and solid (n=30)-type gastric adenocarcinomas and corresponding normal tissues were obtained surgically from 113 patients, ranging in age from 31 to 93 years (69.7±9.3; mean±s.d.), undergoing resection of the stomach at the Iwate Medical University Hospital and related city hospitals. Patients who underwent radiotherapy and chemotherapy before surgery were not included in the study. The Japanese histological criteria18 combined with Lauren's classification22 were used to determine histological type and tumor stage. Intestinal-type tumors were considered as well or moderately differentiated, according to the degree of glandular formation of the cancer epithelium. Solid-type tumors consisted of solid-type poorly differentiated adenocarcinomas. Early cancer was defined as tumor limited to the mucosa and the submucosa; advanced cancer was defined as tumor invading into or beyond the muscularis propria. We performed immunostaining with D2–40 (Dako Cytomation, Kyoto)23 to more accurately assess lymphatic invasion, which is difficult to detect in hematoxylin and eosin sections (Figure 1a). Elastica van Gieson (EVG) staining was used to detect vessel invasion (Figure 1b). Adenocarcinoma of the gastric cardia was defined as a tumor whose epicenter was located 20 mm or less distally to the gastro-esophageal junction and which did not have an associated Barrett's intestinal metaplasia.24 As only seven of the 113 study patients had metastases to distant organs, the relationship between LOH status and distant organ metastasis was not analyzed.
All procedures were performed in accordance with university ethical standards (approval no. H 13-9) and our hospital criteria. All participants gave informed consent to the study.
Crypt Isolation Method
Crypt isolation was performed as described previously.19, 21 Briefly, fresh normal and tumor tissues were sampled immediately after surgical resection. Normal mucosa and tumor tissues were minced with a razor into minute pieces, then incubated at 37°C for 30 min in calcium- and magnesium-free Hanks' balanced salt solution (CMFH) containing 30 mmol/l ethylene-diaminetetraacetic acid (EDTA). Following this, the tissue was stirred in CMFH for 30–40 min. Normal and tumor crypts were separated from the lamina propria mucosa or fibrous stroma. The isolated crypts were immediately fixed in 70% ethanol and stored at 4°C. Fixed crypts were observed and collected under a dissecting microscope (SZ60, Olympus, Tokyo). Several crypts from each case were subjected to routine histologic examination to confirm their origin (Figure 2). The morphologic findings of normal crypts and crypts from different types of gastric carcinoma have been described previously.21
(a) Normal crypts (× 175). (b) Histology of a normal crypt (H&E, × 200). (c) A crypt of intestinal-type (well-differentiated) adenocarcinoma (× 100). (d) Histology of an intestinal-type adenocarcinoma (H&E, × 100). (e) A cell clump of solid-type adenocarcinoma (× 200). (f) Histology of a solid-type adenocarcinoma (H&E, × 200).
DNA Extraction and Microsatellite Analysis
DNA was extracted as described previously.20 Twenty microsatellite markers on 10 chromosome regions were used for allelic loss analysis in this study (1p36: D1S228, D1S548; 3p14: D3S2402, D3S1234; 4p15: D4S2639, D4S1601; 5q21–22: D5S346, D5S82, D5S299; 8p11–12: D8S513, D8S532; 9p21: D9S171, D9S1118; 13q22: D13S162; 17p31.1: TP53; 18q21: D18S487, DCC; 22q13.31: D22S274, D22S1140, D22S1168). The sequences of the primers used were obtained from the Genome Database (http://www.gdb.org/gdb/). A polymerase chain reaction (PCR) assay was performed to quantitatively detect allelic loss at each locus, as described previously.20 The ratio of the allele peak areas (q-value) was calculated for paired normal and tumor samples as described by Habano et al.20 When the q-value was 0.60 or lower, the case was interpreted as an allelic loss. Samples were regarded as uninformative if they showed constitutional homozygosity or MSI. When allelic loss was observed for at least one locus of the chromosomal markers examined, the loss of these chromosomal regions was confirmed. LOH rates for each chromosomal region were calculated by dividing the number of tumors that showed allelic loss by the total number of informative cases for that particular region.
Statistical Analysis
LOH frequencies in each chromosome region of the tumors were compared with various clinicopathological characteristics using the χ2 test for independence. Results were considered significant at P<0.05.
Results
All 10 chromosomal regions tested showed a high degree of allelic loss (1p36 (57%), 3p14 (60%), 4p15 (52%), 5q21–22 (59%), 8p11–12 (49%), 9p21 (57%), 13q22 (52%) 17p13.1 (71%), 18q21 (53%), and 22q13.31 (56%)) (Table 1).
The relationship between LOH status in each chromosomal region tested and clinicopathological findings is shown in Table 1. Allelic loss of 1p36 was significantly associated with cardiac carcinomas (P=0.049), advanced tumors (P=0.029) and lymph node metastasis (P=0.012). The 1p36 LOH rate was also higher in tumors with lymphatic and vessel invasion than in those without lymphatic and vessel invasion, but this difference did not reach statistical significance. 8p11–12 loss was significantly associated with lymph node metastasis (P=0.025), lymphatic invasion (P=0.033) and vessel invasion (P=0.008). 9p21 loss was significantly associated with cardiac tumors (P=0.015) and female gender (P=0.017). 17p13.1 loss was significantly associated with vessel invasion (P=0.004). 18q21 loss was significantly associated with cardiac tumors (P=0.0008). 22q13.31 loss was significantly associated with cardiac tumors (P=0.036), advanced tumors (P=0.002), lymph node metastasis (P=0.024), lymphatic invasion (P=0.017), vessel invasion (P=0.003) and late TNM stage (I vs II–IV, P=0.042). No significant association between LOH on 3p14, 4p15, 5q21–22, 13q22 and any clinicopathological variable was observed.
Discussion
The present study represents a detailed and comprehensive investigation of the relationship between LOH status and various clinicopathological variables in a large panel of intestinal- and solid-type gastric adenocarcinomas. Significantly higher LOH rates (49–71%) from tumor samples obtained by the crypt isolation technique suggest the presence of putative or candidate tumor suppressor genes on chromosomal regions 1p36, 3p14, 4p15, 5q21–22, 8p11–12, 9p21, 13q22, 17p31.1, 18q21 and 22q13.31 involved in the development in intestinal- and solid-type gastric carcinomas. This involvement of several chromosomal regions corresponds to the multistep process known to control the malignant transformation of cells.
Several studies have described 1p36 losses in gastric cancer11, 25, 26 Igarashi et al11 reported that deletion at 1p35-pter is associated with advanced gastric carcinomas, but the correlations between LOH in this region and other clinicopathological factors were not described. Two tumor suppressor genes RIZ1 and RUNX3, located in 1p36, were shown to be inactivated in gastric cancers.26, 27 Hemizygous deletions of RUNX3, a growth regulator of gastric epithelial cells, have been reported to be significantly increased in late TMN stage gastric cancers.27 Our data showed that the loss of 1p36 was significantly associated with advanced tumors and lymph node metastasis. These results support the presence of putative tumor suppressor gene(s) at 1p36 involved in the aggressive behaviors of intestinal- and solid-type gastric carcinomas.
LOH on 8p is frequently found in many types of human cancers, and three commonly deleted regions have been defined at 8p23, 8p21–22 and 8p11–12.15, 28, 29 In gastric cancer, LOH at 8p21–22, which harbors the FEZ1 tumor suppressor gene, has been demonstrated to be a frequent event.15, 29, 30 French et al15 demonstrated that allelic imbalance at this region is associated with poorer survival, but no relationship between LOH status and clinicopathological factors was described in their study. In the present study, our data showed an overall allelic loss rate of 49% at 8p11–12 in intestinal- and solid-type tumors, and allelic loss at this region was significantly associated with lymphatic invasion, vessel invasion, and lymph node involvement. There are no previous reports of significant LOH at 8p11–12 in gastric cancers. Although candidate tumor suppressor genes remain unclear, our results support the presence of tumor suppressor genes at 8p11–12 involved in the invasion phenotype of intestinal- and solid-type gastric carcinoma. LOH in this region is reported to be associated with aggressive behaviors in other human cancers, including bladder and prostate cancer.28, 31
22q13.31 is a common target region of allelic loss on chromosome 22q and is frequently lost in human colorectal and breast cancers.32, 33 The present study showed that LOH of 22q13.31 using D22S274, D22S1168 and D22S1140 is significantly associated with advanced tumor, lymphatic and vessel invasion, node involvement and late TMN stage. These findings suggest that the existence of candidate tumor suppressor gene(s) at this region may contribute to tumor progression and a worse prognosis in intestinal- and solid-type gastric cancers. The BIK gene mapped to 22q13.31 is a proapoptotic gene and may function as a tumor suppressor.34 It has been demonstrated that the BIK gene, complexed with a nonviral gene delivery system, significantly inhibited the growth and metastasis of human breast cancer cells implanted in nude mice and prolonged the life span of the treated animals.35 Two recent published reports described LOH on 22q12–13 in gastric cancer.14, 36 Koo et al14 reported a low overall LOH rate (21%) using D22S283 and D22S274 in 38 patients. Their study suggested that 22q loss may be associated with advanced tumor, though the relationship was not statistically significant. Koshiishi et al observed frequent LOH at a region of 22q containing the p300 gene using D22S304, D22S277 and IL2RB in both intestinal- and diffuse-type gastric carcinomas, but found that LOH was significantly correlated with advanced stage and lymph node metastasis only in the intestinal-type tumor (10 early and 24 advanced). Those authors thus concluded that the p300 gene behaves as a tumor suppressor gene in the intestinal type, but not in the diffuse type of gastric carcinoma.36
It is interesting that allelic loss at TP53 had a significant association only with vessel invasion, but not with other aggressive factors in the present study. Wild-type p53 is an inhibitor of angiogenesis,37 and mutant p53 correlates with increased angiogenesis and malignant progression in melanoma.38 In gastric carcinoma, it has been reported that tumors containing p53 mutations are much more likely to metastasize than tumors without mutations.39 Our findings suggest that inactivation of TP53 may contribute to metastatic potential in intestinal- and solid-type gastric carcinomas. Several studies have reported that 17p13 loss was correlated with gastric wall invasion,5, 40 but other studies have failed to find a significant association.8, 13
Allelic losses at 3p14, 4p15, 5q21–22, 9p21, 13q22 and 18q21 did not show a significant association with aggressive behaviors such as stage (depth of invasion), lymphatic or vessel invasion, and lymph node metastasis in the present study, suggesting that putative or candidate tumor suppressor genes at these chromosomal regions may be involved in carcinogenesis of intestinal- and solid-type gastric carcinoma. It is well known that tumor suppressor genes FHIT, APC, p16, DCC and DPC4 have been mapped to 3p14, 5q21–22, 9p21 and 18q21, respectively. On the other hand, no tumor suppressor genes have yet been characterized at 4p15 and 13q22 (D13S162). Aberrant transcripts and loss of protein expression of the FHIT gene were observed in the majority of gastric carcinomas.41, 42 However, the APC, p16, DCC and DPC4 genes did not show significant mutations in gastric carcinomas,43, 44, 45, 46 implying some other tumor suppressor genes in these chromosomal regions may be involved in gastric carcinogenesis.
The clinicopathological significance of LOH at 5q21–22 and 18q21 has been widely investigated in gastric cancer. Although Nishizuka et al8 reported that 5q21 loss was associated with advanced intestinal-type gastric carcinoma, the present study and other published studies6, 13, 40 have not confirmed this finding. Candusso et al12 demonstrated a strong correlation between 18q21 loss and aggressive behaviors such as gastric wall invasion, lymph node involvement or late TMN stage in cohesive (glandular+solid) type tumors; however, 18q21 LOH did not show prognostic power.12 Several other studies also described a positive correlation between 18q21 loss and tumor invasion or late TMN stage.6, 7 However, the present study and other studies5, 13, 14 did not confirm this reported correlation. Reports on the clinicopathological significance of LOH at 3p14,13, 47 4p15,8, 13 9p2113 and 13q2213, 14 are very rare, and no positive correlation has been found except for one study stating that 13q los was weakly correlated with advanced tumor (P=0.049).13
Gastric cardia adenocarcinoma is thought to be a separate clinical entity from other gastric carcinomas. Studies on LOH in cardiac adenocarcinomas are rare.48, 49 Allelotypes of cardiac adenocarcinoma were analyzed by a previous study, and significantly high LOH rates on several chromosomes were found.49 However, that study did not provide a precise definition of cardiac adenocarcinoma. In the present study, we defined cardiac adenocarcinoma as a tumor with its epicenter located 20 mm or less distally to the gastro-esophageal junction and which did not have an associated Barrett's intestinal metaplasia. This definition is similar to type II tumors (adenocarcinoma of the true cardia) in Siewert's classification.24 Against the background of high LOH rates observed in all chromosomal regions tested in this study, allelic losses at 1p36, 9q21, 18q21 and 22q13.31 were significantly higher in tumors located in the cardia than tumors located elsewhere in the stomach. 17p13.1 (TP53) loss was also higher in cardiac tumors than in noncardiac tumors, but this difference did not reach statistical significance (P=0.059). These findings suggest that tumor suppressor genes at these regions are involved in the development of intestinal- and solid- types of gastric cardia adenocarcinoma. No statistical analysis was performed to assess the relationship of LOH status of cardiac tumors with clinicopathological factors, due to the small number of such tumors in this study (n=20).
In conclusion, this comprehensive analysis utilizing the crypt isolation technique in a large numbers of samples demonstrated that LOH at 1p36, 8p11–12, 17p13.1 and 22q13.31 is significantly associated with aggressive behaviors in intestinal- and solid-type gastric adenocarcinomas, whereas LOH at 3p14, 4p15, 5p21–22, 9p21, 13q22 and 18q21 is not associated with aggressive behaviors. These findings suggest that tumor suppressor genes locating at 3p14, 4p15, 5q21–22, 9p21 13q22, and 18q21 may contribute to the initiation of intestinal- and solid-type gastric carcinoma, and that tumor suppressor genes mapping to 1p36, 8p11–12, 17p13.1 and 22q13.31 may be involved in the progression of these tumor types (Figure 3). In addition, tumor suppressor genes at 1p36, 9q21, 18q21 and 22q13.31 may be specially associated with gastric cardia adenocarcinomas.
References
Tamura G . Genetic and epigenetic alterations of tumor suppressor and tumor-related genes in gastric cancer. Histol Histopathol 2002;17:323–329.
El-Rifai W, Powell SM . Molecular biology of gastric cancer. Semin Radiat Oncol 2002;12:128–140.
Jiao YF, Sugai T, Habano W, et al. Analysis of microsatellite alterations in gastric carcinoma using the crypt isolation technique. J Pathol 2004;204:200–207.
Yustein AS, Harper JC, Petroni GR, et al. Allelotype of gastric adenocarcinoma. Cancer Res 1999;59:1437–1441.
Uchino S, Tsuda H, Noguchi M, et al. Frequent loss of heterozygosity at the DCC locus in gastric cancer. Cancer Res 1992;52:3099–3102.
Wu MS, Shun CT, Wang HP, et al. Genetic alterations in gastric cancer: relation to histological subtypes, tumor stage, and Helicobacter pylori infection. Gastroenterology 1997;112:1457–1465.
Fang DC, Jass JR, Wang DX . Loss of heterozygosity and loss of expression of the DCC gene in gastric cancer. J Clin Pathol 1998;51:593–596.
Nishizuka S, Tamura G, Terashima M, et al. Loss of heterozygosity during the development and progression of differentiated adenocarcinoma of the stomach. J Pathol 1998;185:38–43.
Choi SW, Park SW, Lee KY, et al. Fractional allelic loss in gastric carcinoma correlates with growth patterns. Oncogene 1998;17:2655–2659.
Choi SW, Choi JR, Chung YJ, et al. Prognostic implications of microsatellite genotypes in gastric carcinoma. Int J Cancer 2000;89:378–383.
Igarashi J, Nimura Y, Fujimori M, et al. Allelic loss of the region of chromosome 1p35-pter is associated with progression of human gastric carcinoma. Jpn J Cancer Res 2000;91:797–801.
Candusso ME, Luinetti O, Villani L, et al. Loss of heterozygosity at 18q21 region in gastric cancer involves a number of cancer-related genes and correlates with stage and histology, but lacks independent prognostic value. J Pathol 2002;197:44–50.
Kim KM, Kwon MS, Hong SJ, et al. Genetic classification of intestinal-type and diffuse-type gastric cancers based on chromosomal loss and microsatellite instability. Virchows Arch 2003;443:491–500.
Koo SH, Jeong TE, Kang J, et al. Prognostic implications for gastric carcinoma based on loss of heterozygosity genotypes correlation with clinicopathologic variables. Cancer Genet Cytogenet 2004;153:26–31.
French AJ, Petroni G, Thibideau SN, et al. Allelic imbalance of 8p indicates poor survival in gastric cancer. J Mol Diagn 2004;6:243–252.
Tahara E . Genetic pathways of two types of gastric cancer. IARC Sci Publ 2004;157:327–349.
Tamura G, Sato K, Akiyama S, et al. Molecular characterization of undifferentiated-type gastric carcinoma. Lab Invest 2001;81:593–598.
Japanese Research Society for Gastric Cancer. Japanese Classification of Gastric Carcinoma, 1st English edn. Kanehara-Shuppan: Tokyo, 1999, pp 39–65.
Nakamura S, Goto J, Kitayama M, et al. Application of the crypt-isolation technique to flow-cytometric analysis of DNA content in colorectal neoplasms. Gastroenterology 1994;106:100–107.
Habano W, Sugai T, Nakamura S, et al. A novel method for gene analysis of colorectal carcinomas using a crypt isolation technique. Lab Invest 1996;74:933–940.
Jiao YF, Sugai T, Suzuki M, et al. Application of the crypt isolation technique to the flow cytometric analysis of DNA content in gastric carcinoma. Hum Pathol 2004;35:587–593.
Lauren P . The two histological main types of gastric carcinomas: diffuse and so-called intestinal-type carcinoma. Acta Pathol Microbiol Immunol Scand 1965;64:31–49.
Kahn HJ, Marks A . A new monoclonal antibody, D2–40, for detection of lymphatic invasion in primary tumors. Lab Invest 2002;82:1255–1257.
Siewert JR, Stein HJ . Adenocarcinoma of the gastrointestinal junction: classification, pathology and extent of resection. Dis Esophagus 1996;9:173–182.
Ezaki T, Yanagisawa A, Ohta K, et al. Deletion mapping on chromosome 1p in well-differentiated gastric cancer. Br J Cancer 1996;73:424–428.
Tokumaru Y, Nomoto S, Jeronimo C, et al. Biallelic inactivation of the RIZ1 gene in human gastric cancer. Oncogene 2003;22:6954–6958.
Li QL, Ito K, Sakakura C, et al. Causal relationship between the loss of RUNX3 expression and gastric cancer. Cell 2002;109:113–124.
Adams J, Williams SV, Aveyard JS, et al. Loss of heterozygosity analysis and DNA copy number measurement on 8p in bladder cancer reveals two mechanisms of allelic loss. Cancer Res 2005;65:66–75.
Baffa R, Santoro R, Bullrich F, et al. Definition and refinement of chromosome 8p regions of loss of heterozygosity in gastric cancer. Clin Cancer Res 2000;6:1372–1377.
Vecchione A, Ishii H, Shiao YH, et al. Fez1/lzts1 alterations in gastric carcinoma. Clin Cancer Res 2001;7:1546–1552.
Crundwell MC, Chughtai S, Knowles M, et al. Allelic loss on chromosomes 8p, 22q and 18q (DCC) in human prostate cancer. Int J Cancer 1996;69:295–300.
Castells A, Ino Y, Louis DN, et al. Mapping of a target region of allelic loss to a 0.5-cM interval on chromosome 22q13 in human colorectal cancer. Gastroenterology 1999;117:831–837.
Castells A, Gusella JF, Ramesh V, et al. A region of deletion on chromosome 22q13 is common to human breast and colorectal cancers. Cancer Res 2000;60:2836–2839.
Hur J, Chesnes J, Coser KR, et al. The Bik BH3-only protein is induced in estrogen-starved and antiestrogen-exposed breast cancer cells and provokes apoptosis. Proc Natl Acad Sci USA 2004;101:2351–2356.
Zou Y, Peng H, Zhou B, et al. Systemic tumor suppression by the proapoptotic gene bik. Cancer Res 2002;62:8–12.
Koshiishi N, Chong JM, Fukasawa T, et al. p300 gene alterations in intestinal and diffuse types of gastric carcinoma. Gastric Cancer 2004;7:85–90.
Dameron KM, Volpert OV, Tainsky MA, et al. Control of angiogenesis in fibroblasts by p53 regulation of thrombospondin-1. Science 1994;265:1582–1584.
Grant SW, Kyshtoobayeva AS, Kurosaki T, et al. Mutant p53 correlates with reduced expression of thrombospondin-1, increased angiogenesis, and metastatic progression in melanoma. Cancer Detect Prev 1998;22:185–194.
Shiao YH, Palli D, Caporaso NE, et al. Genetic and immunohistochemical analyses of p53 independently predict regional metastasis of gastric cancers. Cancer Epidemiol Biomarkers Prev 2000;9:631–633.
Sugai T, Habano W, Nakamura S, et al. Correlation of histologic morphology and tumor stage with molecular genetic analysis using microdissection in gastric carcinomas. Diagn Mol Pathol 1998;7:235–240.
Ohta M, Inoue H, Cotticelli MG, et al. The FHIT gene, spanning the chromosome 3p14.2 fragile site and renal carcinoma-associated t(3;8) breakpoint, is abnormal in digestive tract cancers. Cell 1996;84:587–597.
Baffa R, Veronese ML, Santoro R, et al. Loss of FHIT expression in gastric carcinoma. Cancer Res 1998;58:4708–4714.
Maesawa C, Tamura G, Suzuki Y, et al. The sequential accumulation of genetic alterations characteristic of the colorectal adenoma-carcinoma sequence does not occur between gastric adenoma and adenocarcinoma. J Pathol 1995;176:249–258.
Igaki H, Sasaki H, Tachimori Y, et al. Mutation frequency of the p16/CDKN2 gene in primary cancers in the upper digestive tract. Cancer Res 1995;55:3421–3423.
Powell SM, Harper JC, Hamilton SR, et al. Inactivation of Smad4 in gastric carcinomas. Cancer Res 1997;57:4221–4224.
Sato K, Tamura G, Tsuchiya T, et al. Frequent loss of expression without sequence mutations of the DCC gene in primary gastric cancer. Br J Cancer 2001;85:199–203.
Noguchi T, Muller W, Wirtz HC, et al. FHIT gene in gastric cancer: association with tumour progression and prognosis. J Pathol 1999;188:378–381.
Marsman WA, Birjmohun RS, van Rees BP, et al. Loss of heterozygosity and immunohistochemistry of adenocarcinomas of the esophagus and gastric cardia. Clin Cancer Res 2004;10:8479–8485.
Gleeson CM, Sloan JM, McGuigan JA, et al. Allelotype analysis of adenocarcinoma of the gastric cardia. Br J Cancer 1997;76:1455–1465.
Acknowledgements
This work was supported, in part, by the Open Translational Research Project, Advanced Medical Science Center, Iwate Medical University. We thank Mr N Yamada, T Kasai and Miss E Sugawara for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiao, YF., Sugai, T., Habano, W. et al. Clinicopathological significance of loss of heterozygosity in intestinal- and solid-type gastric carcinomas: a comprehensive study using the crypt isolation technique. Mod Pathol 19, 548–555 (2006). https://doi.org/10.1038/modpathol.3800561
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800561
Keywords
This article is cited by
-
Solid-type poorly differentiated adenocarcinoma of the stomach: clinicopathological and molecular characteristics and histogenesis
Gastric Cancer (2019)
-
A microsatellite based multiplex PCR method for the detection of chromosomal instability in gastric cancer
Scientific Reports (2018)
-
miR-204 targets Bcl-2 expression and enhances responsiveness of gastric cancer
Cell Death & Disease (2012)
-
APC gene deletions in gastric adenocarcinomas in a Chinese population: a correlation with tumour progression
Clinical and Translational Oncology (2012)