Abstract
Study design:
A case report of spinal arteriovenous malformation presented as chest pain in a child.
Objectives:
To illustrate the atypical clinical presentation as right chest pain in a child with spinal cord arteriovenous malformation.
Setting:
Chang Gung Memorial Hospital and Chang Gung University, Taiwan.
Case report:
An 8-year-old boy was diagnosed with spinal cord arteriovenous malformation after paraplegia. However, early diagnosis was delayed for the atypical initial clinical presentation as chest pain. After surgery and rehabilitation for 6 months, the patient could walk without assistance.
Conclusions:
Correct diagnosis of spinal cord arteriovenous malformations is sometimes difficult in children with atypical presentations. Early diagnosis relies on detailed examination and high index of suspicion.
Similar content being viewed by others
Introduction
Spinal cord arteriovenous malformations (SCAVMs) are relatively rare diseases in children. They account for about 2% of all spinal lesions in children under the age of 10 years.1 In pediatric SCAVMs, the usual clinical presentations are abrupt neurological decline from spinal cord parenchymal hemorrhage and/or subarachnoid hemorrhage.2 Here, we report a case of SCAVM presented atypically as right chest pain in a child.
Case report
A previously healthy 8-year-old boy was noted to have sudden onset of upper back pain and then soon referred to right chest wall. For the persistent right chest pain, he was brought to two hospitals where myofascial pain was diagnosed. The boy felt bilateral limb weakness and tripped and fell several times over the following days. On the fourth day, bilateral lower limb weakness progressed to the point where he could no longer walk. In addition, urinary incontinence was also noted. He was sent to our emergency department for paraplegia.
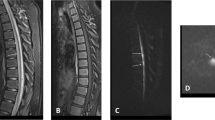
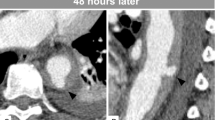
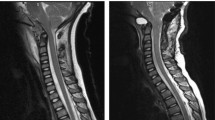
Initial physical examinations in our emergency department showed weakness in bilateral lower limb. There was an increased deep tendon reflex of bilateral knee and bilateral ankle cloni. The American Spinal Injury Association/International Spinal Cord Society (ASIA/ISCoS) International Standard for Neurological Classification of spinal cord injury3 sensory level was at T9. Motor score was 5/25 for right leg and 5/25 for left leg. Deep anal sensation was preserved. The patient was evaluated as ASIA impairment scale grade C with the neurologic level at T9. T–L spine radiograph revealed no significant abnormality. Magnetic resonance imaging of the spine disclosed an intramedullary elongated mass spanning from C5 to C7 levels. Intramedullary hyperintensity T2 signal was noted proximal and distal to the mass extending from C1 to T9 level, which suggested edema or syringomyelia (Figure 1). Another globular lesion was at spinal T1–T2 level (Figure 2). After contrast injection, subtle peripheral enhancement of the mass at the T1–T2 level was revealed (Figure 3).
Magnetic resonance imaging of spine sagittal view disclosed an intramedullary elongated mass spanning from C5 to C7 level with isointense T1 signal (left) and slightly hypointense T2 signal (right, arrow). Intramedullary hyperintense T2 signal was noted proximal and distal to the mass extending from C1 to T9 level.
These findings led to the impression of an intramedullary tumor with hemorrhagic component. Direct neurosurgical intervention was performed for the progressive neurological impairment. Laminectomy was performed from C6–T2 vertebrae. Echo was done and an enlarged cord in T1–T2 level was identified. After the dura was opened, a vascular lesion with a prominent radicular artery feeding from right spinal T1–2 root entry zone was found. The feeding artery was coagulated and incised through the right T1–2 root entry zone. The vascular lesion was totally excised and the surrounding hematoma was also removed. SCAVM was diagnosed postoperatively.
The patient was transferred to our rehabilitation department by 3 weeks postoperatively. ASIA/ISCo motor score of bilateral lower limbs improved to 24/50 (12/25 for the right left leg and 12/25 for the left leg). The sensory level was still at T9. The patient participated in in-patient rehabilitation programs for 6 weeks and outpatient rehabilitation programs regularly after discharge. Six months after surgery the patient could walk without assistance.
Discussion
Spinal cord arteriovenous malformations are relatively rare, comprising about 1/10 of all central nervous system arteriovenous malformations (AVMs) and 3–4% of all spinal cord masses.4 SCAVMs are even less common in children, comprising only 2% of all spinal lesions in children under the age of 10 years and 13% in people under the age of 20 years.1 SCAVMs often result in neurological deficits and disabilities initially and more than 70% of patients will show improvement after adequate treatment and rehabilitation.2, 5
Spinal cord arteriovenous malformations are classified according to their localization and angiographic features. Anson and Spetzler6 classified SCAVMs into four types: type I is dural arteriovenous fistula; type II is intramedullary glomus AVM; type III is intramedullary juvenile type AVM; and type IV is intradural, extramedullary arteriovenous fistula. While type I and IV SCAVMs most commonly occur in elderly and middle-aged adults separately, type II and type III SCAVMs occur more often in pediatric age groups.
Early diagnoses of SCAVMs are important because patients are likely to have better functional statuses after treatment if their pretreatment deficits are relatively mild.7 The present case, however, illustrates the potential difficulty in the early diagnoses of SCAVMs in children. Although the usual clinical presentations of pediatric SCAVMs reported in most studies are abrupt neurological deteriorations,2 our patient presented with the atypical initial symptoms of back pain and the following right chest pain. The pain might have resulted from irritated central and/or radicular nerve fibers from the bleeding of the SCAVM.
Rehabilitation programs for children with spinal cord injury should be made according to their neurologic level, age, development, cognition, neuromuscular ability and family support. Neurologic improvements may continue for a period of time while these children keep growing and developing; periodic re-evaluation and the re-establishment of new goals are very important in these patients.8
Conclusion
Correct diagnosis of pediatric SCAVMs with an atypical presentation relies on a high index of suspicion. Early diagnosis, adequate treatment and comprehensive rehabilitation programs contribute to better functional prognosis in these children.
References
Berand R . Vascular malformation of the spinal cord. In: Vinken PJ, Bruyn GW (eds). Handbook of Clinical Neurology, vol. 12, Elsevier: Amsterdam, North-Holland, 1972, pp. 548–555.
Riché MC, Modenesi-Freitas J, Djindjian M, Merland JJ . Arteriovenous malformations (AVMs) of the spinal cord in children: a review of 38 cases. Neuroradiology 1982; 22: 171–180.
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury. ASIA: Chicago, 2002.
Cogen P, Stein B . Spinal cord arteriovenous malformation with significant intramedullary components. J Neurosurg 1983; 59: 471–478.
Rodesch G, Hurth M, Alvarez H, Ducot B, Tadie M, Lasjaunias P . Angio-architecture of spinal cord arteriovenous shunts at presentation. Clinical correlations in adults and children. The Bicêtre experience on 155 consecutive patients seen between 1981–1999. Acta Neurochir 2004; 146: 217–227.
Anson J, Spetzler R . Interventional neuroradiology for spinal pathology. Clin Neurosurg 1992; 39: 388–417.
Westphal M, Koch C . Management of spinal dural arteriovenous fistulae using an interdisciplinary neuroradiological/neurosurgical approach: experience with 47 cases. Neurosurgery 1999; 45: 451–458.
Massagli TL . Medical and rehabilitation issues in the care of children with spinal cord injury. Phys Med Rehabil Clin N Am 2000; 11: 169–182.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, CC., Wang, CM., Chu, NK. et al. Spinal cord arteriovenous malformation presenting as chest pain in a child. Spinal Cord 46, 456–458 (2008). https://doi.org/10.1038/sj.sc.3102133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102133
Keywords
This article is cited by
-
Spontaneous epidural spinal haematoma in children caused by vascular malformations
European Spine Journal (2016)
-
Intramedullary spinal cord cavernous malformations presenting with unexplained chest pain: case report and review of the literature
Child's Nervous System (2013)