Abstract
Study design:
A case report of spinal cord infarction following endoscopic variceal ligation.
Objectives:
To describe an exceedingly rare case of spinal cord infarction following endoscopic variceal ligation.
Setting:
Department of Orthopaedic Surgery, Kagoshima, Japan.
Methods:
A 75-year-old woman with cirrhosis caused by hepatitis C virus, who was admitted to our hospital for the treatment of esophageal varices, experienced numbness of the hands and lower extremities bilaterally following an endoscopic variceal ligation procedure. Sensory and motor dysfunction below C6 level progressed rapidly, resulting in inability to move the lower extremities the following day. Magnetic resonance imaging of the spine revealed abnormal spinal cord signal on T2-weighted images from approximately C6 through T5 levels, which was diagnosed as spinal cord infarction.
Results:
The patient underwent hyperbaric oxygen treatment. Her symptoms and signs related to spinal cord infarction gradually remitted, and nearly complete disappearance of neurological deficits was noted within 3 months after the start of treatment.
Conclusion:
We speculate that the pathogenesis of the present case may have involved congestion of the abdominal–epidural–spinal cord venous network owing to ligation of esophageal varices and increased thoracoabdominal cavity pressure.
Similar content being viewed by others
Introduction
The spectrum of etiologies of spinal cord infarction is as diverse as that for cerebral infarction. Since the number of reported cases of spinal cord infarctions due to treatment for esophageal varices has been very small, the pathogenesis and prognosis of this condition have remained largely unclear.
Case report
A 75-year-old woman with cirrhosis caused by hepatitis C virus was admitted to our hospital for the treatment of esophageal varices. After a successful endoscopic variceal ligation procedure, the patient experienced numbness of the hands and lower extremities bilaterally. During the procedure, systolic blood pressure transiently increased to 189 mm Hg, though she had no previous history of hypertension. The patient began to experience rapid loss of motor function in the upper and lower extremities bilaterally, resulting in the inability to move her lower extremities the following day. She also exhibited urinary retention.
On physical examination, her right upper extremity strength ranged from 3/5 to 4/5 throughout while left upper extremity strength was 4/5 distally as determined by manual muscle testing. Lower extremity strength was grade 0/5 throughout bilaterally, with absence of deep tendon reflexes. Sensory examination revealed decreased light touch, vibration sensation and proprioception below approximately C6 level. Rectal sphincter tone was absent.
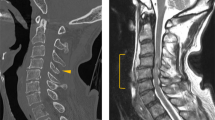
Magnetic resonance imaging (MRI) of the spine performed 18 h after endoscopic variceal ligation revealed abnormal spinal cord signal on T2-weighted images from approximately C6 through T5 levels, which corresponded to the abnormal findings noted on the patient's physical examination and was diagnosed as spinal cord infarction (Figure 1a).
(a) Sagittal T2-weighted magnetic resonance imaging (MRI) of the spine 18 h after endoscopic variceal ligation, demonstrating high-signal intensity within the spinal cord from approximately C6 through T5 levels. (b) Sagittal T2-weighted MRI 6 months after the episode, revealing slight persistence of the hyperintense change within the spinal cord, though with clear decrease in intensity compared with 18 h after variceal ligation.
The patient underwent once-daily hyperbaric oxygen (HBO) treatment for 20 days. Each treatment involved pressurization to 2 atm for 1 h with 15 min for descent and 15 min for ascent. Her symptoms and signs related to spinal cord infarction remitted gradually, and both the muscle weakness and sensory deficits in the upper and lower extremities and neurogenic bladder had almost completely remitted within 3 months after the start of treatment. MRI examination performed 6 months after the episode revealed slight persistence of the hyperintense change within the spinal cord on T2-weighted images, but with clear decrease in intensity compared with the previous MRI (Figure 1b).
Discussion
Spinal cord infarction commonly occurs due to arterial ischemia associated with systemic hypotension, aortic diseases such as dissection, aneurysm or thrombosis or aortic surgery. Spinal venous infarction is much rarer than spinal arterial infarction, and well-recognized causes of it include vascular malformation, epidural hematoma and decompression sickness. Iatrogenic spinal cord infarction is quite rare, and there are only a few reported cases of neurological deficits due to spinal cord infarction following endoscopic sclerotherapy or ligation of esophageal varices.1, 2, 3 Although the etiology of this condition is still unclear, inflow of the sclerosant from the esophagus to the anterior spinal artery or the spinal vein and hemodynamic changes have been suggested as possible causes of it. Giangaspero et al.4 reported a case of myelopathy due to degeneration of the corticospinal tract associated with diffuse infarction of the spinal gray matter following a portocaval shunt for hepatic cirrhosis and esophageal varices, and suggested that modification of the spinal blood flow caused by creation of portosystemic shunts might be the basic pathogenetic mechanism of this rare complication.
In the case of portal hypertension due to cirrhosis, redistribution of portal flow occurs along the left gastric vein and, subsequently, into the esophageal veins, leading to formation of esophageal varices. The spinal cord venous network depends directly on the epidural venous network, which is extensively linked with the abdominal veins. We speculate that ligation of esophageal varices may have increased portal hypertension and induced congestion of abdominal veins, leading to congestion of the spinal cord venous network and resulting in spinal cord infarction. Moreover, the increase in arterial pressure observed during the procedure in the present case suggests the possibility of increased thoracoabdominal cavity pressure, which might have increased spinal venous congestion.
Although to our knowledge, there have been few reports of the use of HBO therapy in treatment of spinal cord infarction, HBO is an attractive method of treatment that has frequently been used for patients with cerebral ischemia. It has been speculated that the neuroprotective effect of HBO treatment after ischemia involves rapid restoration of oxygen and improvement of energy supply to ischemic tissue.5 Although there are no clear guidelines for the treatment of spinal cord infarction, the present case suggests the usefulness of HBO treatment in patients with spinal cord infarction.
References
Seidman E, Weber AM, Morin CL, Ethier R, Lamarche JB, Guerguerian AJ et al. Spinal cord paralysis following sclerotherapy for esophageal varices. Hepatology 1984; 4: 950–954.
Heller SL, Meyer JR, Russell EJ . Spinal cord venous infarction following endoscopic sclerotherapy for esophageal varices. Neurology 1996; 47: 1081–1085.
Debette S, Gauvrit JY, Desseaux G, Nibbio A, Henon H, Pruvo JP et al. Paraplegia after ligation of esophageal varices. Neurology 2003; 60: 879–880.
Giangaspero F, Dondi C, Scarani P, Zanetti G, Marchesini G . Degeneration of the corticospinal tract following portosystemic shunt associated with spinal cord infarction. Virchows Arch A Pathol Anat Histopathol 1985; 406: 475–481.
Hossmann KA . Viability thresholds and the penumbra of focal ischemia. Ann Neurol 1994; 36: 557–565.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tofuku, K., Koga, H., Yamamoto, T. et al. Spinal cord infarction following endoscopic variceal ligation. Spinal Cord 46, 241–242 (2008). https://doi.org/10.1038/sj.sc.3102092
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102092