Abstract
Objective:
To demonstrate the prospective construct validity of the walking index for spinal cord injury (WISCI) in US/European clinical population.
Design:
Prospective Cohort in Denmark, Germany, Italy and the USA.
Participants/Method:
Participants with acute complete/incomplete (ASIA Impairment Scale (AIS) A, B, C and D) traumatic spinal cord injuries were enrolled from four centers. Lower extremity motor scores (LEMS), WISCI level and Locomotor Functional Independence Measure (LFIM) levels were assessed with change in ambulatory status. WISCI progression was assessed for monotonic direction of improvement (MDI). LEMS were correlated to WISCI/LFIM. Use of walking aids/braces were analyzed.
Results:
One hundred and seventy participants were enrolled and 20 excluded. Of the 150 participants (USA 112/150; Europe 38/150) (AIS A=59, B=19, C=32, D=40), LEMS and WISCI assessments were performed initially and at final assessment (3–12 months post injury) or until maximum WISCI score of 20. Eighty-five percent of motor complete (66/78) and 10% (7/72) of motor incomplete participants showed no progression (73/150). Of the remaining participants (77/150) who improved, 81% (62/77) showed MDI. However, the deviation from MDI occurred only at one time-point in 10/15 participants. LEMS correlated with WISCI at initial and final assessment (0.47 and 0.91 P<0.001). Parallel bar use differed between the US and Europe possibly due to patterns of care. Use of braces also differed.
Conclusion:
The results support the hierarchical ranking of the WISCI scale and the correlation of WISCI levels to impairment (LEMS) in a clinical setting of four nations. Differences in practice between the US and Europe need consideration in design of trials.
Similar content being viewed by others
Introduction
Outcome measures for use in clinical trials for spinal cord injury (SCI) to establish efficacy must be valid and reliable.1 The walking index for spinal cord injury (WISCI) was introduced in 20002 and modified3 the following year as a walking capacity measure, which incorporates the use of walking aids, braces and physical assistance on a 21 level scale (Table 1). It was ranked by an international group of SCI clinicians and investigators from most impaired level to least impaired level and demonstrated construct (theoretical) and face validity. It was subsequently compared to four other scales in a clinical population of mixed SCI and spinal cord lesions for demonstration of retrospective criterion validity (compared to other scales).4 Recently, it was utilized in a multicenter randomized clinical trial, assessed by blinded observers, and showed high correlations with lower extremity motor score (LEMS), balance, walking speed, 6-min walk and locomotor FIM illustrating prospective criterion validity.5 The prospective construct validity or validation of the theoretical formulation of monotonic function has not been published but preliminary results have been presented.6 The rationale of this prospective study was first to demonstrate validation for the formulation of hierarchical ranking in more than one center and second, to show a correlation of WISCI levels (functional capacity) with the LEMS (impairment). We hypothesized that the 21-level WISCI scale would follow a monotonic progression and correlate with LEMS at initial and final assessment. The secondary objectives were to show a correlation between WISCI and Locomotor Functional Independence Measure (LFIM) levels and the utility of the WISCI in the United States compared to Europe.
Participants/Method
The US group
Eligible participants included acute complete and incomplete ASIA Impairment Scale (AIS) A/B/C/D) traumatic spinal cord injuries, levels C2 to L3 (International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI),7 admitted within 1 month of injury and followed 6–12 months after discharge from the hospital. AIS A participants at initial report8 showed little or no progression of WISCI, therefore, recruitment was limited to AIS B/C/D for the remainder of the study. Excluded participants included those with significant head injury, upper/lower extremity fracture, an immobilization device that interfered with neurological assessment and/or ambulation or those with WISCI 20 on initial evaluation.
To validate the hierarchical ranking of the WISCI,2 change in ambulation status, the LFIM Score9 and the LEMS according to the ISNCSCI were recorded.7 The LEMS were assessed by physicians and the WISCI levels by the therapist independently at admission and discharge. Change of walking status did not always correspond to a defined WISCI level. Participants were encouraged to walk at their maximal WISCI level, safely, for 10 m on a level surface.
Descriptive data (Table 1 Descriptors) were recorded for the type of walking aids used (parallel bars, standard or rolling walker, forearm, axillary crutches or canes) and braces (short leg, long leg or equivalents such as ankle ace bandage, knee stabilizer). Physical assistance of one ranged from contact guarding to not equal or greater than moderate assistance (min/mod).
European group (Denmark, Germany and Italy)
The inclusion/exclusion criteria were similar to the US group. Descriptive data for use of parallel bars, walkers, crutches and canes were collected to compare the frequency of use between the European centers and the United States. WISCI levels, LEMS and LFIM, were performed at the same time period, and use of devices and physical assistance were recorded. Physicians performed the neurological assessment, and therapists did the LFIM and WISCI assessments independently. The use of walking aids and braces were recorded at each assessment based on the descriptors previously published.2 (Table 1 Descriptors).
Statistical analysis
Descriptive analysis of the monotonic (one direction) progression of participants and the frequency of deviations and the number of levels deviated was performed for the US and European centers separately for all traumatic SCI. Descriptive analysis was also performed on the frequency of use of walking aid devices and braces in the US and European centers during rehabilitation and at discharge.
Spearman's correlations were performed between changes in LEMS and WISCI levels from the initial assessment to 1-year follow-up or until the participants reach a level of 20 on the WISCI. Spearman's correlations were also performed for initial LEMS/WISCI levels and final LEMS/WISCI levels. Similar analyses were performed for the LFIM. P-value <0.05 was considered statistically significant. In addition, the frequency and level of the seven LFIM levels were compared to the 21 WISCI levels for all 77 participants whenever there was a change in ambulatory status (either a change in the WISCI or LFIM).
Results
Of the 170 participants who were enrolled in the study, 11 dropped out, four died and five were excluded because of a WISCI 20 at their initial evaluation. The remaining 150 participants were followed for 6–12 months or until a maximum WISCI of 20 (Table 2). Eighty-five percent of motor complete and 10% of motor incomplete participants showed no progression from wheelchair. For those participants who showed improvement, 81% demonstrated monotonic directional improvement (MDI). In 10/15 participants who failed to show MDI, this occurred at only one-time point and typically, occurred when a device such as a walker was removed too early and then was required again in subsequent assessment.
AIS A participants showed little or no progression in the United States and Europe, but those who progressed were low thoracic or lumbar levels (T12-L3), as expected.10 Severity of injury was similar in the United States and Europe, except for AIS B (Table 2).
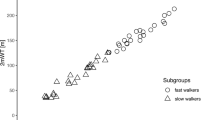
The correlations of the initial and final LEMS/WISCI levels were significant. Similarly, all correlations were significant between LFIM and WISCI at initial and final assessments for those who progressed. The correlation for LEMS with WISCI final assessment for those who progressed, however, was significant for the US group but not for the Europe group (Table 3a and 3b).
Table 4a reflects the use of walking aids at any time during the rehabilitation process. Typically, participants used multiple types of walking aids as they progressed to ambulation through the WISCI levels. For example, a specific participant might initially use parallel bars, progress to a walker and then a cane, which would total three walking aids for this participant. The majority of US and European participants used walking aids during their rehabilitation. In the United States, only 32% and in Europe 50% used a walking aid at their final assessment. Parallel bars were used more frequently in Europe (78%) than United States 19% (Table 4a). Rolling walkers were used more frequently than standard walkers in both groups.
Table 4b illustrates the use of braces at any time during the rehabilitation process, and typically, participants used multiple braces as they progressed through the WISCI levels. Fewer participants used braces in Europe than the United States (Table 4b), but the United States had more AIS A/B participants to ambulate. Although brace use during rehabilitation was higher in the United States, it was similar to Europe at the final exam.
The most commonly utilized WISCI levels during rehabilitation for the US group were 20, 17, 8, 0, 19, 6, 13, 15 and 4 (ranging from 47 to 10 assessments). The remaining WISCI levels (16, 12, 14, 1, 2, 9, 11, 18, 7 and 10) were utilized less than 10 times, and two levels (WISCI 3 and 5) were not scored at all. The most common WISCI levels scored in the European group were 20, 19, 8, 4 and 13. WISCI levels 17, 0 and 15, which were used commonly in the US group were not used at all in the European group. Since each participant was scored at any change in ambulatory status, the number of assessments will exceed the number of participants.
The frequency of WISCI scores in relation to LFIM is illustrated in Table 5. This table represents a comparison of WISCI levels to LFIM scores based on 77 subjects at any time there is a change in walking status (change in either WISCI or LFIM score). Often a specific LFIM level has 3–7 WISCI levels.
Discussion
MDI
These findings support the first hypothesis of MDI for a prospective cohort of consecutive admissions of traumatic participants with SCI to a regional center in the US and three centers in Europe. Only 19% of cases deviated from the hierarchy established in the original WISCI report and subsequently modified. The European Centers showed a higher proportion of MDI than the United States (94 vs 76%), but the assessments were less frequent and the health care delivery system differs. In the United States, the length of stay is shorter than Europe (typically 4–6 weeks for paraplegics and 8–10 weeks for tetraplegics vs 4 months for paraplegics and 6 months for tetraplegics).11, 12, 13 Therefore, in the United States, therapists are required to progress patients more aggressively. The therapists may progress the participant to walking without a device (walking aid or brace) or physical assistance in order to expedite discharge at one assessment, but later find that they are unable to maintain this level and need to restore the device or physical assistance. As a result, 10 of 14 participants in the United States deviated from the MDI. This difference in practice should be considered in planning an international trial involving different nations with different health care systems.
WISCI correlation to LEMS
The second hypothesis is based on a clear relationship of WISCI levels with the severity of the motor impairment as determined by LEMS. Such a relationship has been previously reported by Waters et al.10 for community compared to household ambulation and has also been shown to correlate with the speed of walking.14, 15 The randomized clinical trial of locomotor training5 for 146 participants assessed by blinded observers from six centers showed an average LEMS of 45/50 and a WISCI of 18/20 at 6 months, and a high correlation of LEMS to WISCI levels at 3, 6 and 12 months for both the experimental and control arms combined.15 The WISCI Scale ranking by a group of international experts, designed for use in clinical trials, was based on severity from most impaired to least impaired, which integrated physical assistance with walking aids and braces. For that reason, levels such as 14 and 17, which require physical assistance but less aids or devices, may be ranked above levels 9, 12 and 13 which require no physical assistance but more aids/devices. The correlation of WISCI levels to LEMS at initial and final assessment was highly significant in this prospective study and supports our second hypothesis.
Use of devices
Use of parallel bars differed significantly, with the European centers assessing participants in parallel bars 78% compared to 22% in the United States. This is a likely reflection of differences in the health care systems, due to length of stay, but is an important consideration for international multicenter trials. Since walking aids may be required in as many as 86% of participants, any functional capacity scale (speed, distance, efficiency), which measures walking improvement should consider standardization of aids. Without standardization of treatment practice, use of aids, braces and physical assistance may alter the reliability of functional capacity outcome measures such as the WISCI, speed and distance.
The use of rolling walkers was common in all centers and the only walker used in Europe. This will require a change in the standardization of walking aids in our original description,2 as we recommended the standard walker.
Use of braces by participants during rehabilitation (Table 4b) was greater in the United States than in Europe, but it was similar at discharge. The difference in use during rehabilitation is probably related to the 20% of AIS A/B participants in the United States who progressed to walking compared with none among the AIS A/B participants in Europe. This difference may reflect the method of training/assessment for a short leg brace (SLB) in Europe, whereas in the United States ace bandages for ankle stability is equivalent to an SLB.
All 21 levels of the WISCI scale were assessed in the total sample of participants, but only the United States recorded no assessments of a WISCI 5 (parallel bars with or without a brace), which again may reflect the pattern of use of walking aids based on the health care system. The WISCI levels at discharge were similar for the United States and Europe, with WISCI levels 0, 20, 14 and 8 common to both groups but 17 being more frequent in the United States. Level 17 (no device, no braces and physical assistance of 1) would probably be discharged home at 16, which is the most common level following 0 and 20 reported by Morganti et al.4 based on a retrospective discharge analysis. This aspect of testing is an important consideration for a functional capacity scale as compared to a disability scale, and the level of function required at discharge and follow-up in the community should not be substituted. This may explain the deviation from monotonic progression in several US participants who decreased their WISCI level at discharge with no change in motor score.
WISCI vs LFIM
There is a good correlation between the WISCI and LFIM at final assessment for those participants who progressed in both the US and Europe (Table 3a). On closer examination, however, Table 5 shows major discrepancies with participants in levels 4 and 5 of the LFIM, which have 11 to 12 levels of the WISCI, respectively. The strong correlations likely reflect the clustering of scores at the WISCI 0 and 20 levels, whereas the discrepancies reflect the major differences between the two scales. The WISCI is a measure based on the MDI related to less impairment with 21 gradations of use of walking aids, braces and physical assistance.2, 3 The LFIM has only seven gradations based on burden of care. In addition, the LFIM 5, defined as supervision, does not appear in the WISCI scale and is often used in the United States in a broader context to justify continued hospitalization. Patients who achieve a level 6 (independent with a device) in the United States frequently must be discharged to home, whereas in Europe, a plateau of all function is the basis for discharge.16 Again, one must be cautious in designing trials, so that these differences in practice are taken into consideration.
Although the sample of European participants was small and did not entirely match the US sample, the descriptive data were helpful in demonstrating differences in the pattern of care and the monotonic progression.
In summary, the hierarchical ranking of the WISCI scale has been validated in a clinical setting by demonstration of monotonic progression of walking capacity in a prospective population of acute participants with SCI during recovery. The correlation of this walking capacity recovery with the LEMS (impairment) improvement supports the theoretical validation of the development of the scale. Differences in the use of walking aids and braces during rehabilitation, not previously reported, should be considered in the plan of clinical trials.
References
Steeves JD, Lammertse D, Curt A, Fawcett J, Tuszinski M, Ditunno J et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP Panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Ditunno Jr JF, Ditunno PL, Graziani V, Scivoletto G, Bernardi M, Castellano V et al. Walking index for spinal cord injury (WISCI): an international multicenter validity and reliability study. Spinal Cord 2000; 38: 234–243.
Ditunno PL, Ditunno Jr JF . Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord 2001; 39: 654–656.
Morganti B, Scivoletto G, Ditunno P, Ditunno JF, Molinari M . Walking index for spinal cord injury (WISCI): criterion validation. Spinal Cord 2005; 43: 27–33.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D et al. Weight-supported treadmill vs. over-ground training for walking after acute incomplete SCI. Neurology 2006; 66: 484–493.
Patrick M, Ditunno JF, Biering-Sorensen F, Scivoletto G, Ranier A, Marino RJ . Validation of the Walking Index for Spinal Cord Injury (WISCI) in a USA and European Clinical Population. J Spinal Cord Med 2006; 29: 340 (Abstract).
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26: S50–S56.
Ditunno JF, Burns AS, West C, Patrick M . Clinical validation of the walking index for spinal cord injury (WISCI) scale: a preliminary report. J Spinal Cord Med 2003; 26: S37 (Abstract).
Keith RA, Granger CV, Hamilton BB, Sherwin FS . The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil 1987; 1: 6–18.
Waters RL, Adkins R, Yakura J, Vigil D . Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994; 75: 756–760.
McKinley WO, Seel RT, Gadi RK, Tewksbury MA . Nontraumatic vs. traumatic spinal cord injury: a rehabilitation outcome comparison. Am J Phys Med Rehabil 2001; 80: 693–699.
Biering-Sorensen F, Pederson V, Clausen S . Epidemiology of spinal cord lesions in Denmark. Paraplegia 1990; 28: 105–118.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil 2003; 84: 1266–1275.
van Hedel HJ, Wirz M, Dietz V . Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil 2005; 86: 190–196.
Ditunno Jr JF, Dobkin B, Spinal Cord Injury Locomotor Trial (SCILT) Study Group. Prospective Validity and Responsiveness to Change in Walking Scale for Spinal Cord Injury (WISCI) in a Randomized Clinical Trial. ISCOS proceedings Athens 2004. Abstract 055.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M . Effects on age on spinal cord lesion patients' rehabilitation. Spinal Cord 2003; 41: 457–464.
Acknowledgements
We thank the staff of each rehabilitation center who helped with this study including: Lori Nicolini, Cheryl West, Mary Schmidt-Read and Susan Sammartino (Pennsylvania); Barabara Morganti (Italy); Hanne Knudsen, Janni Steen and Mette Molin Nefling (Denmark); and Dominique Jehle (Germany). This study was supported in part by grant #H133N000023 from the National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitation, US Department of Education, Washington, DC and the generosity of the European Centers.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ditunno, J., Scivoletto, G., Patrick, M. et al. Validation of the walking index for spinal cord injury in a US and European clinical population. Spinal Cord 46, 181–188 (2008). https://doi.org/10.1038/sj.sc.3102071
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102071
This article is cited by
-
Validity and reliability of the 2-minute walk test in individuals with spinal cord injury
Spinal Cord (2023)
-
Orthotic walking outcome of persons with motor complete low thoracic spinal cord injury—a retrospective study
Spinal Cord (2023)
-
Effect of pelvic laparoscopic implantation of neuroprosthesis in spinal cord injured subjects: a 1-year prospective randomized controlled study
Spinal Cord (2022)
-
Using a logarithmic model to predict functional independence after spinal cord injury: a retrospective study
Spinal Cord (2019)
-
Lower extremity outcome measures: considerations for clinical trials in spinal cord injury
Spinal Cord (2018)