Abstract
Study Design:
Case control.
Objective:
To test the reported correlation of hypotension, polydipsia, and hyponatremia with higher levels of spinal cord injury (SCI).
Setting:
A Veterans Administration Hospital, USA.
Methods:
The records of men who were paralyzed owing to trauma at any spinal cord level with motor complete lesions (ASIA A or B) and who received an annual physical and laboratory examination were reviewed for age, duration of paralysis, level of paralysis, blood pressure (BP), serum sodium, and 24 h urinary volume, creatinine, and sodium. Creatinine clearance and fractional excretion of sodium (FcNa) were calculated. Spearman rank-order correlations (rs) were carried out.
Results:
Patients were aged 25 to 88 years, median 56 years, paralyzed 2–61 years, median 26 years, with levels of paralysis ranging from C2 to L4, median T4, n=111. From lower to higher levels of paralysis FcNa increased (0.4–7.3%), mean BP diminished (132–66 mmHg), urine volume increased (600–5400 ml), and serum sodium was reduced (148–129 mEq/l) – rs=0.29, 0.49, −0.22, and 0.23, respectively. Increasing 24 h urinary volumes correlated with lower serum sodium concentrations but higher creatinine clearance, rs=−0.28, 0.24. Increasing 24 h urinary sodium improved creatinine clearance, rs=0.37. P-values ranged from <0.05 to <0.001.
Conclusion:
Higher levels of SCI correlate with reduced sodium conservation, hypotension, polydipsia, and hyponatremia. Greater water intake raises creatinine clearance but lowers serum sodium. Greater salt intake increases creatinine clearance.
Similar content being viewed by others
Introduction
Formerly, patients with spinal cord injury (SCI) were encouraged by their caregivers to drink much fluid to maintain urine flow and reduce infection of the urinary tract. This advice is no longer given with much consistency; but many patients, notably the more severely paralyzed, produce large amounts of urine.1 Excessive fluid intake has, in addition, been invoked to explain the hyponatremia associated with higher levels of paralysis.2 Still another effect of higher levels of paralysis is diminished blood pressure (BP).3 It is asked, therefore, whether a syndrome of hypotension, polydypsia, and hyponatremia at higher levels of paralysis can be demonstrated in a single cohort and whether it can be explained.
Methods
Subjects
The records of subjects who were registered for continuing care at this institution and who attended the SCI clinic for an annual evaluation were reviewed. To more clearly test the association of the level of paralysis with the proposed syndrome, only patients with the more severe grades of paralysis, ASIA Impairment Scale A or B, were selected. For purposes of calculations, the levels of paralysis were numbered 1 through 25 for levels C1 to L5. Subjects with assisted ventilation, antihypertensive medication, or acute illness were excluded. Subjects with untreated hypertension, cardiovascular disease, or autonomic dysreflexia were not excluded. BP was recorded with the patient sitting in his wheelchair soon after arriving at the outpatient clinic. In the event of stress from travel or apprehension, BP recording was delayed. Supine BP was not recorded because recumbent position might obscure orthostatic hypotension in some patients. All patients had been instructed to take usual medication but to drink no coffee and eat no breakfast. Urine specimens were collected by the patient for 24 h before the morning of the check-up appointment. The items reviewed for this survey were age, cause of paralysis, duration of paralysis, level and grade of paralysis, BP, 24 h urine volume, serum sodium, 24 h urine sodium, and creatinine clearance. Fractional excretion of sodium (FcNa) was calculated by urinary sodium (mmol/l)/serum sodium(mEq/l)/urine creatinine (mg/dl)/serum creatinine (mg/dl) × 100 and expressed as percent. The record review was approved by the Institutional Review Board for this institution.
Comparisons
The level of paralysis, FcNa, BP, 24 h urine volume, serum sodium, 24 h urine sodium, and creatinine clearance were compared non-parametrically. Coefficients of correlation were calculated by the Spearman rank-order method. A probability of 0.05 was considered a significant correlation. Calculations were carried out by the Primer of Biostatistics.4
Results
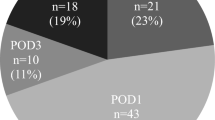
Ten subjects were excluded from data collection because of ventilator dependence (three), diaphragmatic pacing (three), antihypertensive medication (two), and fever (two). One hundred and eleven subjects remained; all were male; all but two were paralyzed due to trauma. The age of the subjects at review was 25–88 years, median 56 years, and the duration of paralysis was 2–61 years, median 26 years. The data collected from the records of these subjects have been summarized in Table 1.
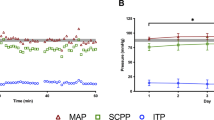
Comparison of parameters reveals that a high level of paralysis is correlated with a high FcNa, low BP, high urine output, and low serum sodium (Table 2). The correlation between the level of paralysis and FcNa, BP, and urine volume are shown in Figures 1, 2 and 3. FcNa and serum sodium are inversely related; FcNa and urinary sodium are directly related. As urine volume increases serum sodium decreases (Figure 4), but creatinine clearance increases (Figure 5). Similarly, greater urinary excretion of sodium, reflecting greater salt intake, enhances creatinine clearance (Figure 6).
Discussion
The association between the higher levels of paralysis owing to SCI and hypotension, polydipsia, and hyponatremia – noted separately in previous reports1, 2, 3 – has been confirmed collectively in this report. In addition, impaired sodium conservation has been found at the higher levels of paralysis. This association could not be explained by sodium intake, which was not related to level of paralysis. The reduced retention of sodium in the presence of hyponatremia at the higher levels of paralysis suggests salt wasting on the basis of a central nervous system lesion, comparable to that noted with some cases of severe brain injury.5 Such a myelopathic form of salt wasting might play a role in the syndrome of hypotension, polydipsia, and hyponatremia.
The recovery of sodium from glomerular filtrate is under hormonal control – the renin–angiotensin–aldosterone system (RAS) – but is permitted by renal innervation. When the sympathetic innervation of the kidney is disabled, the control of renal blood flow, tubular secretion of angiotensin II, and the production of renin by the juxtaglomerular granular cells are impaired, reducing the recovery of sodium from the glomerular filtrate.6, 7 Thus, although the RAS of the tetraplegic man is activated to super normal levels by orthostasis,8 its continued effectiveness may be blunted by a denervation of the sympathetic supply to the kidneys. The RAS does not prevent hyponatremia at the higher levels of paralysis. In addition, as recovery of filtered sodium is a metabolically intense activity, the possibility that the reduced BP of the severely paralyzed impedes renal tubular activity might be considered.9 However, no correlation between FcNa and BP was found in this survey. Instead, the correlation between a high FcNa and a low creatinine clearance was found, suggesting that diminished renal blood flow may have contributed to impaired conservation of sodium.
The hypotension of higher levels of paralysis is related to the disability of both the sympathetic and the somatic nervous systems in these subjects. First, the somatic nervous system lesion impairs breathing ability, manifested by decreasing vital capacity with progressively higher levels of paralysis.10 Breathing is the pulmonary pump that determines venous return and cardiac output and supports BP.11, 12 The lowering of BP coincides with the loss of vital capacity as the level of paralysis becomes higher.3, 10, 13 Second, this somatic disability also inactivates the assistance of leg muscle contraction in the return of venous blood from the lower extremities.14 Third, although the centrally disabled sympathetic system reacts by reflex to noxious stimuli with autonomic dysreflexia, it fails to respond to orthostasis with vasoconstriction to protect the circulation against gravity.15 Fourth, although the venous capacity of the lower extremities is constricted and may oppose venous pooling with sitting, the reservoir of venous blood volume available to the pulmonary pump for support of BP with orthostasis is reduced.16 Fifth, intravascular volume is diminished.17 This reduction is explainable by the reported leakage of osmotically active material, albumin, from the intravascular space, greater at higher levels of paralysis.18 The relative importance of these factors on the protection of the circulation against gravity is uncertain. An end result of these hypotensive factors is the reduction of cardiac output and heart size as found in the tetraplegic subject.19 In summary, the hypotension of severe SCI is multifactorial.
Polydipsia has been assumed in the presence of polyuria, which cannot be sustained in the absence of increased fluid intake. Although patients were not questioned regarding thirst, the mechanisms of the polydipsia of the higher levels of paralysis can be considered from the list of reported causes of thirst – depletion of intracellular volume or of extracellular volume, central nervous system lesions, and hormonal effects.20 Taking the first consideration, total water per body weight in the spinal cord injured subject is reportedly comparable to controls, but intracellular volume is diminished and extracellular volume is expanded (although intravascular volume is constricted).17, 21, 22 Furthermore, the intracellular volume is more constricted in the tetraplegic than in the paraplegic subject, thus coinciding with the polydipsia of higher levels of paralysis in the current survey. The first mechanism, thirst induced by diminished intracellular volume, may apply to the spinal cord injured subject. The second mechanism, the central nervous system lesions associated with thirst, is unlikely to apply as the lesions cited are rostral to the spinal cord. The third mechanism, via hormonal factors, mainly renin and angiotensin, might apply, however. These hormones tend to be elevated in the subjects with higher spinal cord lesions.23 Hemorrhagically induced hypotension raises brain angiotensin, which can stimulate thirst experimentally.24 The polydipsia of the upper levels of SCI may result from both hormonal reactions and abnormal compartment volumes.
The possibility exists that patients had been instructed to drink fluids as a method of reducing urinary tract infections. However, it is unlikely that these instructions discriminate between higher and lower levels of SCI, both being subject to urinary tract infections.
The hyponatremia of the high levels of paralysis can be related to four factors. First, renal conservation of sodium may be impaired owing to sympathetic denervation of the kidney or impaired renal blood flow, as discussed. Second, antidiuretic hormone (ADH) is secreted to exceptionally high concentrations in response to orthostatic hypotension.25 The stimulating effect of hypotension overcomes the inhibitory effect of hypotonicity. Thus, water is conserved despite serum hyponatremia.26 Third, failure of the tetraplegic patient to excrete a water load after the suppression of ADH has been reported, suggesting an ADH-independent mechanism of renal conservation of water.27 Fourth, the augmented water intake, evidenced by polyuria, provides ample substrate for the expression of ADH. In summary, the hyponatremia of SCI can be related to the effects of partially blocked sodium conservation, enhanced water conservation, and increased fluid intake.
The described syndrome of high SCI – salt wasting, hypotension, polydipsia, and hyponatremia in the chronically paralyzed – can be recognized in clinical practice, and a physiological connection of the components of this syndrome can be understood. Salt wasting is suggested by a high FcNa (greater than 2.5%)28 determined on a spot urine sample in the presence of a low serum sodium. Hypotension is recognized by its symptoms with orthostasis or by direct BP monitoring. Polydipsia is suggested by noting urine volume when creatinine clearance is tested by a 24 h collection. Salt wasting and hypotension represent direct effects of disabled sympathetic and somatic nervous systems whereas polydipsia and hyponatremia are indirect effects of these lesions. The net effect is incomplete support for a circulatory system that depends upon on a compensatory water intake in the severely paralyzed.
As parameters of a fragile circulation, this syndrome has therapeutic implications. Water ingestion alone can raise BP and prevent orthostatic syncope, and may be an example of patient self-treatment.29, 30 However, although excessive fluid intake contributes to hyponatremia, which, if extreme, threatens cerebral function, treating this condition with fluid restriction may be depriving the tetraplegic patient with a defense against insufficient circulation. Treating the hyponatremia of an ill patient with fluid restriction but without saline and volume support can be fatal.31 Supplementing salt intake alone can improve the excretion of a water load and ameliorate orthostatic hypotension.32, 33 It can be pointed out that the median calculated daily sodium intake by the subjects surveyed was 3000 mg (130 mmol), well under the recommended 6000 mg (260 mmol) maximum for hospital patients.34 In contrast to able-bodied hospital patients, for whom salt restriction is often recommended, the SCI patient paralyzed at a high level has a need for more dietary salt. Attention to both salt and water metabolism in patients with the syndrome described could improve circulation to critical areas such as the brain, the skin, the kidneys, and the lungs.35
Conclusion
Evidence for a syndrome of higher levels of motor complete SCI – renal salt wasting, hypotension, polydipsia, and hyponatremia – has been collected. The pathophysiology is probably related to sympatholytic effects on renal tubular recovery of sodium, to the loss of BP support through both the sympathetic and somatic nervous system lesions, to stimulation of thirst by volume depletion of the intracellular compartment and high levels of renin and angiotensin, and to excessive antidiuretic activity, hormonal and renal. The circulatory reserve of the high-level SCI patient is limited and dependent on salt and water intake.
References
Brown M, Pyzik S, Finkle JR . Causes of polyuria and polydipsia in patients with injuries of the cervical spinal cord. Neurology 1959; 9: 877–882.
Sica DA, Midha M, Zawada E, Stacy W, Hussey R . Hyponatremia in spinal cord injury. J Am Paraplegia Soc 1990; 13: 78–83.
Frankel HL, Michaelis LS, Golding DR, Beral V . The blood pressure in paraplegia – 1. Paraplegia 1972; 10: 193–198.
Glantz SA . Primer of Biostatistics 4th edn. McGraw Hill: New York, NY 1997.
Palmer BF . Hyponatremia in patients with central nervous system disease: SIADH versus CSW. Trends Endocrinol Metab 2003; 14: 182–187.
DiBona GF . Neural control of the kidney: functionally specific renal sympathetic nerve fibers. Am J Physiol Regul Integr Comp Physiol 2000; 279: R1517–R1524.
Quan A, Baum M . The renal nerve is required for regulation of proximal tubule transport by intraluminally produced ANG II. Am J Physiol Renal Physiol 2001; 280: F524–F529.
Kooner JS, Frankel HL, Mirando N, Peart WS, Mathias CJ . Haemodynamic, hormonal and urinary responses to postural change in tetraplegic and paraplegic man. Paraplegia 1988; 26: 233–237.
Sejersted OM, Mathisen O, Kiil F . Oxygen requirement of renal Na-K-ATPase-dependent sodium reabsorption. Am J Physiol 1977; 232: 152–158.
Baydur A, Adkins RH, Milic-Emili J . Lung mechanics in individuals with spinal cord injury: effects of injury level and posture. J Appl Physiol 2001; 90: 405–411.
Brecher GA . Venous return. Grune and Stratton: New York 1956.
Boutellier U, Farhi LE . Influence of breathing frequency and tidal volume on cardiac output. Respir Physiol 1986; 66: 123–133.
Frisbie JH . Breathing and the support of blood pressure after spinal cord injury. Spinal Cord 2005; 43: 406–407.
Miller JD, Pegelow DF, Jacques AJ, Dempsey JA . Skeletal muscle pump versus respiratory muscle pump: modulation of venous return from the locomotor limb in humans. J Physiol 2005; 563: 925–943.
Guttmann L, Munro AF, Robinson R, Walsh JJ . Effect of tilting on the cardiovascular responses and plasma catecholamine levels in spinal man. Paraplegia 1963; 1: 4–18.
Frieden RA, Ahn JH, Pineda HD, Minutoli F, Whelan E . Venous plethysmography values in patients with spinal cord injury. Arch Phys Med Rehabil 1987; 68: 427–429.
Houtman S, Oeseburg B, Hopman MTE . Blood volume and hemoglobin after spinal cord injury. Am J Phys Med Rehabil 2000; 79: 260–265.
Ring J, Seifert J, Lob G, Stephan W, Probst J, Brendel W . Elimination rate of human serum albumin in paraplegic patients. Paraplegia 1974; 12: 139–144.
Kessler KM et al. Cardiovascular findings in quadriplegic and paraplegic patients and in normal subjects. Am J Cardiol 1986; 58: 525–530.
McKinley MJ, Johnson AK . The physiological regulation of thirst and fluid intake. News Physiol Sci 2004; 19: 1–6.
Greenway RM, Houser HB, Lindan O, Weir DR . Long-term changes in gross body composition of paraplegic and quadriplegic patients. Paraplegia 1970; 4: 301–318.
Cardus D, Wesley G, McTaggart WG . Total body water and its distribution in men with spinal cord injury. Arch Phys Med Rehabil 1984; 65: 509–512.
Mathias CJ, Christensen NJ, Corbett JL, Frankel HL, Goodwin TJ, Peart WS . Plasma catecholamines, plasma renin activity and plasma aldosterone in tetraplegic man, horizontal and tilted. Clin Sci Mol Med 1975; 49: 292–299.
Phillips MI, Heininger F, Toffolo S . The role of brain angiotensin in thirst and AVP release induced by hemorrhage. Regul Peptide 1996; 66: 3–11.
Sved AF, McDowell FH, Blessing WW . Release of antidiuretic hormone in quadriplegic subjects in response to head-up tilt. Neurology 1985; 35: 78–80.
Jacob G, Ertl AC, Shannon JR, Furlan R, Robertson RM, Robertson D . Effect of standing on neurohumoral responses and plasma volume in healthy subjects. J Appl Physiol 1998; 84: 914–921.
Leehey DJ, Picache AA, Robertson GL . Hyponatraemia in quadriplegic patients. Clin Sci 1988; 75: 441–444.
Mathew OP, Jones AS, James E, Bland H, Groshong T . Neonatal renal failure: usefulness of diagnostic indices. Pediatrics 1980; 65: 57–60.
Tank J et al. Pressor effect of water drinking in tetraplegic patients may be a spinal reflex. Hypertension 2003; 41: 1234–1239.
Claydon VE, Schroeder C, Norcliffe LJ, Jordan J, Hainsworth R . Water drinking improves orthostatic tolerance in patients with posturally related syncope. Clin Sci 2006; 110: 343–352.
Arieff AI, Llach F, Massry SG . Neurological manifestations and morbidity of hyopnatremia; correlation with brain water and electrolytes. Medicine 1976; 55: 121–129.
Sica DA, Culpepper RM . Severe hyponatremia in spinal cord injury. Am J Med Sci 1989; 298: 331–333.
Pechere-Bertschi A et al. Circadian variations of renal sodium handling in patients with orthostatic hypotension. Kidney Int 1998; 54: 1276–1282.
Singer AJ, Werther K, Nestle M . The nutritional value of university-hospital diets. N Engl J Med 1996; 335: 1466–1467.
Frisbie JH, Steele DJR . Postural hypotension and abnormalities of salt and water metabolism in myelopathy patients. Spinal Cord 1997; 35: 303–307.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Frisbie, J. Salt wasting, hypotension, polydipsia, and hyponatremia and the level of spinal cord injury. Spinal Cord 45, 563–568 (2007). https://doi.org/10.1038/sj.sc.3101984
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101984
Keywords
This article is cited by
-
Incidence of and factors associated with hyponatremia in traumatic cervical spinal cord injury patients
Spinal Cord Series and Cases (2022)
-
A study of predictors for hyponatraemia in patients with cervical spinal cord injury
Spinal Cord (2018)
-
Hyponatremia in spinal cord injury patients: new insight into differentiating between the dilution and depletion forms
Spinal Cord (2015)
-
Risk factor analysis for low blood pressure and hyponatremia in acutely and subacutely spinal cord injured patients
Spinal Cord (2012)
-
Correction of orthostatic hypotension by respiratory effort
Spinal Cord (2010)