Abstract
Study design:
Cross-sectional; survey.
Objectives:
To describe the utilization, accessibility and satisfaction of primary and preventive health-care services to individuals with long-term spinal cord injuries, and compare results among three countries: the United States, Canada and the United Kingdom.
Setting:
The Canadian sample was obtained from the Canadian Paraplegic Association – Ontario and Manitoba Divisions. The British sample was recruited from the Northwest Regional Spinal Injuries Centre in Southport and National Spinal Injuries Centre at Stoke Mandeville Hospital in Aylesbury. The American sample was recruited through Craig Hospital in Englewood, CO, USA.
Method:
A total sample of 373 individuals aging with a spinal cord injury participated in a mailed survey. The Health Care Questionnaire was used to measure utilization, access and satisfaction with primary care and preventive services.
Results:
In total, 93% of individuals reported having a family doctor, 63% had a spinal injuries specialist and 56% had both a family doctor and spinal injuries specialist. Considerable duplication of services occurred for general medical and preventive services, although lifestyle and emotional issues were not addressed for over 75% of the participants. Significant differences were found in utilization among Canada, US and UK, with Canadians most likely to receive health care from family physicians and Americans most likely to receive care from specialists. Access to and satisfaction with health services was not significantly different among countries.
Conclusion:
People with long-standing spinal cord injuries develop complex maps by which they seek out appropriate primary health-care and preventive services. Given the differences among countries, it is clear that the health delivery model plays an important role in how and where individuals receive health services.
Similar content being viewed by others
Introduction
People with spinal cord injuries report anecdotally that they often cannot find a family physician in their community whose office and equipment are accessible, or who is willing to take them on owing to issues of cost, expertise and time requirements. Further, they report disappointment at the level of knowledge and experience with disability in the medical community.1, 2 Current political rhetoric is full of references to access to health services, usually referring to wait times or geographic distribution of services. However, for people with disabilities, access problems are also related to four additional types of barriers: physical inaccessibility, lack of expertise about disability, attitudes toward disability and health system issues.3, 4, 5
High re-hospitalization rates and complications in the early years following spinal cord injury have been the impetus for examining health-care utilization during the first decade postinjury. A recent study found that over the course of the first 6 years, contact with the health-care system diminished with time. Individuals tended to see their family doctors for both general health and disability-related issues, and had significantly less contact with their physiatrists in the latter years than in the initial year.6 Individuals aging with a spinal cord injury report a greater number of secondary health conditions than the general aging population,6 which lead to more frequent and longer hospital re-admissions compared with the general population.7 However, the long-term use of health services following spinal cord injury is not well understood.
Before proceeding further, it is important to offer a number of definitions. First, the term primary care is used to refer to medical services provided at the first point of contact with the health-care system. According to Starfield et al,8 primary care is typically defined according to four cardinal domains:
-
1
first contact: the point of contact with the health-care system and the gateway to other more specialized services;
-
2
longitudinality: a relationship that extends over a long period of time, typically a minimum of 6 months;
-
3
comprehensiveness: attention to all health problems; and
-
4
coordination: awareness and communication regarding all aspects of health care for a given patient.
The term family doctor was used in this study to describe physicians specializing in the provision of comprehensive primary care for individuals of all ages, organ systems and diseases.9 The terms general practitioner (GP), primary care physician and family physician are also commonly used terms to refer to this area of specialty.
Because of the international context of this study, it is also important to clarify the term used to designate physicians specializing in the care of people with spinal cord injuries. A number of terms are used, including physiatrist, rehabilitation doctor and rehabilitation specialist. In this paper, we use the term spinal injuries specialist, in recognition of this subspecialty of rehabilitation medicine in the UK.
Other definitions of interest include access and utilization. In our previous work on access to primary care for people with disabilities, we have used the term access to refer to the absence of four types of barriers: physical barriers, negative attitudes, lack of expertise about disability, and systemic or structural barriers in the health-care system.10 Utilization refers to services sought in the preceding year, according to the measure used.11, 12
Our own research and that of others1, 6, 13, 14, 15, 16, 17, 18 shows that people with disabilities are relatively high users of health services. It also shows, however, that they have significantly more unmet health needs than comparable members of the general population.19 People with disabilities report three times more unmet health needs than the overall population.19 Even after controlling for the effects of health and chronic disease, disability still represents a significant source of both health service use and unmet health need.
Bockenek17 provides evidence of difficulties experienced by people with disabilities in receiving appropriate and accessible health services. Available literature points to a number of inequities in the delivery of health services to people with disabilities, and particularly to difficulties in accessing primary and preventive care.1, 20, 21, 22, 23 Chan et al24 found that the greater the number of functional limitations an individual reported, the less likely they were to receive preventive services, such as a mammogram or Pap smear. Nosek and Howland25 also found that difficulties with access to primary and preventive care increased with severity of disability.
Bowers et al26 suggest that there are at least three types of expertise needed in order to provide effective primary care to people with disabilities:
-
knowledge of the medical–technical aspects of the presenting health complaint;
-
biographical knowledge about the individual and his or her health history; and
-
systems knowledge regarding policies, programs, benefits and criteria.
To this, we would add knowledge of the medical/technical aspects of the pre-existing disability. Veltman et al27 surveyed people with five significant types of adult disability, including spinal cord injury, regarding the role they expected their family doctor to take. People expected not only concern for their general health and access to specialists but also expertise on disability, advocacy for the patient relative to programs and needs, and emotional support.
In the absence of adequate primary care, authors have noted a number of other strategies that people with disabilities may use to ensure their health needs are met. Several authors reported that people with disabilities are disproportionately high users of institutional services, such as hospital and emergency clinics.17, 18 The location of these services are usually physically accessible, and they typically offer a variety of resources such as diagnostics, prescription and other ancillary services. There are obvious advantages of accessing services in one location: issues of inaccessibility, transportation/parking and other logistics. The research also shows that people with disabilities often use specialists for primary care; that is, as their first line of contact in the event of a new health problem.1, 17 Thus, physiatrists, orthopedists, neurologists or rheumatologists with whom they already have a relationship become the first contact with the health-care system when a problem arises.
In summary, the literature documents the difficulties experienced by people with disabilities in accessing a reasonable standard of primary care. However, conspicuously absent are studies of how specifically the health-care system is negotiated, and what issues are being addressed by whom and with what frequency.
Much of the data on health-care utilization cited above comes from the United States. In the process of a longitudinal study of long-term health following a spinal cord injury, we had an opportunity to compare Canada, United States and United Kingdom. These three countries represent three distinct health-care delivery models:
-
Canada has a publicly funded system, where everyone is meant to have full access to necessary medical services, and physicians act as private practitioners who coordinate and control access to specialty services,
-
Britain also has a publicly funded system, where general practitioners are organized into primary care trusts, and care is integrated at both the community and hospital levels,
-
The American system is primarily privately funded, and is organized and delivered by privately directed health organizations and third-party payers. However, a considerable portion of long-term patients has funding through Medicare or Medicaid, by virtue of the disability or of their age.
Recent survey research comparing these three health systems shows that both patients and doctors have concerns about access in all three systems.28 Although many factors such as rates of seeing specialists and rates of satisfaction and quality of care were similar, there were some notable differences in access issues among the three countries. Whereas people in all three countries experienced difficulties with access to needed services, in Canada and the UK, these difficulties were attributed to wait times and shortages of people and facilities, whereas in the US, they attributed to costs and coverage of health services.29 Among those considered ‘sicker adults’ or those with multiple or chronic conditions, the risk of access barriers and coordination failures was particularly high.19 Between 33 and 50% of such adults were not satisfied with their access to care, with the highest rates of dissatisfaction being in the US and the lowest being in the UK.
The purpose of this paper is to:
-
1
describe the utilization and accessibility of primary and preventive health-care services to individuals with long-term Spinal Cord Injury, and
-
2
compare primary care and preventive health service utilization and accessibility among three countries: the United States, Canada and the United Kingdom.
Methods
Study design
The present study was part of a larger longitudinal international survey examining the effects of aging on individuals with a Spinal Cord Injury.30 This study utilized a cross-sectional analysis of data collected between 2001 and 2003.
Sample
A total sample of 373 was obtained from Canada, the United Kingdom and the United States. The Canadian sample was derived from the member database of the Canadian Paraplegic Association (CPA) – Ontario and Manitoba divisions. It included 127 participants, with an average age of 55.9 (±10.7) years and an average disability duration of 32.1 (±8.4) years. The British sample was recruited from the Northwest Regional Spinal Injuries Centre (NRSIC) in Southport, and National Spinal Injuries Centre (NSIC) at Stoke Mandeville Hospital in Aylesbury. It consisted of 162 individuals with an average age of 62 (±7.7) years and an average injury duration of 39.2 (±5.5) years. The US sample was recruited through Craig Hospital in Englewood, CO USA, and it included 84 participants with an average age of 56.7 (±8.9) years and an average duration of disability of 35.3 (±6.5) years. Participants were included if they:
-
had incurred a spinal cord injury at least 20 years previously,
-
were between the age of 15 and 55 years at the time of injury, and
-
were admitted to rehabilitation within 1 year of injury.
Participant characteristics are found in Table 1. The table reflects the sampling criteria, showing that this is an older sample with a substantial duration of disability. In common with much spinal cord injury research, the sample was dominated by males. There are significant differences between the three countries on age and duration of disability, with the British sample being the oldest and of the longest duration.
Data collection
Participants from all three countries were contacted by mail to request their participation in the study. For those who agreed, a questionnaire package containing the Health Care Questionnaire (HCQ) was either sent out, along with a stamped return envelope, or was completed by the interviewer during a telephone or in-person interview. The questionnaire package contained:
-
1
Demographic data: including age, injury level and duration of disability.
-
2
HCQ: The HCQ is 46-item measure of access and satisfaction with health services (see Appendix A1). The HCQ is a compilation of two published measures: the Primary Care Questionnaire11 and the patient satisfaction with Health Care Provider Scale (PSHCPS).12 The PSHCPS has been found to demonstrate both internal consistency reliability (Cronbach's alpha 0.93) and construct validity, according to the original authors.12 No reliability or validity data was published with the Primary Care Questionnaire11 and no further psychometric studies could be found. The adapted HCQ used in this study allowed us to determine what services were received from both family physicians and spinal injuries specialists, and the level of accessibility and satisfaction with those services. The HCQ is comprised of four subscales: access, prevention, counselling and satisfaction. Psychometric analyses conducted as part of this study included inter-item and item-total correlations, principal components analysis and internal consistency reliability. As Table 2 shows, the eight resulting subscales (four for family doctors and four for spinal injuries specialists) had internal consistency reliability (Cronbach's alpha) in the range of 0.55–0.87. Factor analysis supported unidimensionality for all eight subscales, with factor loadings above 0.30 for the majority of items.
Table 2 Psychometric properties of the health-care questionnaire
Ethics
Ethics approval was obtained from the Queen's University Research Ethics Board, as well as the hospital review boards at each site.
Results
Objective 1: Utilization of health services
Table 3 shows physician utilization by the sample as a whole, as well as by country. Referring to the results for the total sample (N=373), in the first column of the table, almost all of our sample reported having a family doctor (93%), whereas only two-thirds had a spinal injuries specialist (63%). More than half of the sample had both a family doctor and a spinal injuries specialist (56%), and about one-third had only a family doctor (36%). A very small percentage had only a spinal injuries specialist (6%), and less than 1% had no doctor at all.
About half of our sample reported that they saw another medical specialist besides the spinal injuries specialist (49%). Of those individuals who reported seeing other specialists (n=182), a total of 275 contacts were made with specialists in all. The average number of specialists seen in the sample was 1.5 in the preceding year.
Navigating the system
Of the 341 participants who had a family doctor, Table 4 shows the top 10 issues for which members of our sample felt they would seek the assistance of their family doctor. Specific mention was made of two particular problems by more than 80% of the sample: pain and fatigue. More than two-thirds of individuals felt their family doctor was the most appropriate professional to consult for new problems, spinal cord injury-related problems (such as fatigue, pain, bowel and bladder problems), preventive health services (annual physical, female breast exam, blood tests and urine specimen) and personal problems.
Table 5 shows the top 10 issues that participants brought to their spinal injuries specialists (n=230). The most common issue for which they saw their specialists was routine rehabilitation follow-up (91%). Approximately half felt that their specialist was the most appropriate person to see for specific spinal cord injury-related diagnostics (eg, urinary tract ultrasound, neurological exam, blood test, urine specimen) or for an annual physical exam. Just under half reported that they would see the spinal injuries doctor for a flare-up of an existing problem, for pain or for a new problem.
Considering the information within Tables 4 and 5 together, two issues can be identified. First, given the high numbers in both tables, there is considerable scope for duplication of services. Second, closer inspection shows that seven of the 10 items listed on each table are common to both: new problem, flare-up of an existing problem, annual physical, pain, blood test, urine specimen and bowel/bladder. The three unique items for family doctors are: fatigue, personal problems and breast exam. The three unique items for spinal injuries specialists are: routine rehabilitation follow-up, urinary ultrasound and neurological exam.
Looking more closely at duplications, Table 6 shows the issues for which participants reported that they would seek help from both their family doctor and spinal injuries specialist. This analysis involved only those 204 participants who had both a family doctor and a spinal injuries specialist, and thus were faced with choosing who was the most appropriate practitioner for a particular problem. Approximately 20–25% of those participants reported that both their family doctor and spinal injuries specialist were involved in the provision of care for bowel and bladder issues (26%), medical flare-ups (25%), urine specimen testing (21%) and pain (20%).
Perhaps more troubling are the issues for which participants reported that they would consult neither physician (Table 6). For more than 75% of participants, issues of sexual health, alcohol use, community functioning and emotional health were not addressed by either the family doctor or spinal injuries specialist. Some of these omissions may be owing to the age of the sample and the possibility that participants considered these issues were not applicable to them. For example, although family planning and work may not be issues for which service was sought by this aging sample, issues like community functioning, relationships and emotional issues may be especially problematic for this population if not addressed in a timely and effective manner.
Objective 2: Differences between countries
There were significant differences between countries on the provision of care (see Table 3). Almost all Canadians and Britons reported having a family doctor (97 and 99% respectively), whereas significantly fewer Americans (76%) had one. Having a spinal injuries specialist was not significantly different across countries, but Canada was the lowest at 58%, with Britons and Americans at 65 and 66%, respectively. Americans were significantly more likely to have only a spinal injuries specialist (23%). There was also a significant difference between countries in the extent of utilization of other specialists, with Britons having the lowest at 38% in the past year (versus 56 and 58% for the US and Canada, respectively).
Table 4 shows reasons for consulting the family doctor, and again there were significant differences in patterns of utilization between countries. The services used by more than 80% of the sample in each country are highlighted in the table. It is notable that the highest utilization of family medicine is clearly in Canada, followed by the UK and then the US. As stated above, of the 341 sample members who had a family doctor, Canadians and Britons were generally more likely to seek care from the family doctor than Americans in virtually every instance. In particular, Canadians and Britons were significantly more likely to approach the family doctor for fatigue, pain or a personal problem, and to have breast exams (females only). Canadians were also significantly more likely than Britons to have blood tests and annual physicals from the family doctor.
However, that does not necessarily mean that Americans received less service. Whereas Britons and Canadians were most likely to consult their family doctor, Americans were more likely to seek health care from their spinal injuries specialist for both spinal cord injury-related issues, general preventive care and general health care. Table 5 shows that both American and Canadian participants were significantly more likely than British to see their spinal injuries specialist for follow-up, flare-up of a prior problem, pain or a new problem. Significantly fewer Canadians saw their rehabilitation specialist for annual physical reviews and blood tests, presumably because they would see the family doctor for this.
The most common reason to see a spinal injuries specialist in all three countries was for routine rehabilitation follow-up (Canada and US – 99%; UK – 84%). For Canadians, the next most common reasons to see a rehabilitation specialist were ultrasound (62%) and bowel/bladder problems (60%). Britons also tended to see the spinal injuries specialist for urinary tract ultrasounds (76%) and annual physicals (72%). Americans were most likely to consult their rehabilitation specialists for pain (69%), annual physical reviews (68%) and bowel/bladder problems (66%).
In Britain and the US, individuals were more likely to receive an annual physical from their spinal injuries specialists than in Canada (72 and 68%, versus 48%). In the United States, annual check-ups were performed with essentially the same frequency by family doctors as by rehabilitation specialists (70% family, 68% rehabilitation), whereas in Canada, family physicians performed the vast majority of annual physical reviews (94 versus 21%).
Problems of duplication of service were most pertinent for flare-ups and pain among Canadians and for bowel and bladder problems among Britons (Table 6). Britons seem to be the least likely to seek any attention from either medical provider for psychosocial or community living issues. Looking at the lower portion of Table 6, more than 80% of the British sample said they would not seek care from either doctor for the problems listed. Canadians were most likely to seek care on these issues.
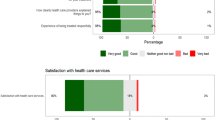
Access and satisfaction
Table 7 shows the results of questions about satisfaction and accessibility from the HCQ. In general, family doctors appear to be more accessible than spinal injuries specialists. Participants tended to feel that family doctors could be reached within 1 day (88% family doctor versus 55% spinal injuries specialist), were able to provide the care when it was needed (93 versus 71%), were able to make house calls (61 versus 10%) and provided specialist referrals (98 versus 80%) with more frequency than the spinal injuries specialist. A greater number of spinal injuries specialists, however, were reported to have offices that were physically accessible – both the space itself (85% rehabilitation specialist versus 83% family physician) as well as the equipment (86 versus 56%) than family doctors.
Overall, Britons reported having the most accessible family doctors (85%) compared to Canadians (74%) or American (78%). However, Americans most frequently rated their rehabilitation specialists (79%) as accessible as compared to Canadians (69%) and Britons (53%).
An overall satisfaction rate of 74% was reported for family doctors and 76% for spinal injuries specialists. No significant differences in satisfaction were found either between spinal injuries specialists and family doctors or among countries.
Discussion
The original purpose of this research was to look at extrinsic factors affecting aging with a spinal cord injury, and particularly the effects on secondary complications.30 The HCQ offered information on service utilization, access and satisfaction with primary care and spinal injuries specialists, as well as simple utilization of specialists. Pain, fatigue, bowel and bladder issues were the secondary problems that most commonly brought members of our sample into contact with medical professionals in the preceding year. The present research shows that 65–90% of people depend on the assistance of their family doctor for these problems, and 45–65% depend on their spinal injuries specialist.
It is important in understanding the findings to recognize the limits on generalizability arising from the sampling process. The sample was derived from specific regions within each of the participating countries (Ontario and Manitoba, Canada; Colorado, USA; and Aylesbury and Southport, England). To the extent that these areas have unique regional characteristics, some of the findings may reflect these. Furthermore, the British and American samples are derived from hospital databases, whereas the Canadian sample is derived from a community organization, and thus some of the differences seen could be attributable to this sampling factor.
Whereas Canada and the UK have universal health care, in the US the provision of health care is dependent on an individual's funding source (private insurance, Medicare, Medicaid) and varies depending on the exact specifications of the insurance policy. For example, insurance plans may only cover specific services, coverage may or may not last the duration of a catastrophic injury or high deductibles may prohibit routine use of the health-care system. The current study did not specifically address funding as a factor in the utilization of heath care.
Difficulties navigating the health-care system were highlighted as one of the four key barriers to health care for individuals with mobility impairments, along with physical access, knowledge, sensitivity and respect, and coverage issues.3 Individuals with long-term spinal cord injury appear to have developed complex maps in order to obtain the care they require with a number of overlapping areas of care as well as missed health-care priorities. According to Bowers et al,31 people with disabilities take on a number of roles in order to maximize effectiveness of medical care: some individuals stated that they had become educators about disability for their doctors; some became managers or coordinators of their own care; and some became researchers and substituted their own research for the perceived lack of provider expertise.
For preventive and general health issues, both new and ongoing, the family doctor was the first choice for the majority of our sample, regardless of country of origin. Specialized testing and follow-up related to spinal cord injuries, however, fall in the realm of the spinal injuries specialist. Service overlap occurs for ongoing spinal cord issues (ie bowel and bladder problems, pain). The issue of an annual physical also falls within the gray zone and highlights the confusion as to which physician provides which service. Issues of psychological health, lifestyle and social functioning were unlikely to be treated by either medical doctor, despite the growing literature that points to the strong relationship between psychosocial factors and health.30
The question therefore remains what factors influence when and where services are provided and who provides them? The availability of near-by rehabilitation facilities may be one factor that affects how the system is navigated. Bockenek17 surveyed 144 individuals who visited a weekly spinal clinic and found that 96% of their American sample considered the rehabilitation physician to be their primary care physician; only 6% had another physician who treated them for general health problems.
Rehabilitation centers and specialized spinal cord injury units32 are likely to provide multiple benefits to individuals. Firstly, they are familiar to some individuals as the places where they obtained their initial rehabilitation, facilitating a long-term relationship and coordinated care. Secondly, they house specialized knowledge and resources. Research conducted in the area of primary care and disability shows that most doctors have only a very small percentage of their caseload that consists of people with disabilities;10 therefore, knowledge of spinal cord injury is likely limited owing to a lack of critical volume. Thirdly, spinal cord injury specialist centers are more likely to be physically accessible and have accessible medical equipment.1
Another strategy to ensure the receipt of appropriate community medical care is through the use of specialists with whom the individual already has a relationship.1 Although the use of specialists may overcome knowledge barriers for some individuals, the pattern of specialty use clearly varies between countries, suggesting a larger system-level influence.
Differences in the health utilization patterns among countries suggest that systemic-level barriers and facilitators are at play. Differences between countries may be a function of a number of factors, both tangible and intangible. Tangible factors might include specific parameters of the health-care system like physician compensation, insurance coverage, geographic dispersion of services or regional coordination mechanisms. Examples of indirect influences might be the culture of the country and by extension, of the health-care system, both primary care and rehabilitation.
In Canada and UK, individuals are most likely to have their health needs addressed by a family physician, whereas spinal injuries specialists are seen for specialized preventive services such as neurological exams, urinary tract investigations, skin care, specialized counselling services, sexual functioning, functional issues. Americans are the least likely to have a family physician, and conversely are more inclined to see their rehabilitation specialists, as compared to Britons and Canadians.
This study demonstrates the power of the health-care delivery system to shape utilization. The professional contact model predominately used in Canada provides individuals with a strong long-term link to their family physicians, who both provide primary care and act as a gatekeeper to speciality services.33 This delivery model, coupled with the shortage of specialists, creates a natural path to the family physicians for most health-care needs.
In the United States, a largely private system is predominately organized around specialty care.34 It is not uncommon for American specialists to maintain a close relationship with patients.35 Therefore, the larger number of individuals without a family doctor, as compared to Canada and the UK, may not necessarily reflect a lack of service, simply differently provided service. The results of this study support previous findings of a higher ratio of service provided by rehabilitation specialists versus family physicians in the US, compared to both Canada and the UK.34, 35
In contrast to both Canada and the United States, the UK's National Health Service uses an integrated community model, where primary care trusts serve as a point of contact to provide health care in a community setting. Only a small portion of health care (approximately 10% of services) is provided privately to those who want and are able to pay for it.36 The impact of a community-based system is reflected by the high percentage of individuals who have a family doctor and the high frequency of house calls. Although Britons reported the least frequent use of services by family doctors or spinal injuries specialists, health services may in fact be provided by other health professionals in a community health context. This study only examined physician care and may have missed services provided within an integrated care context, where not only health but also social care occurs, such as in the UK. With primary care reform on the health care agenda internationally, it may become more common for primary and preventive health services to be offered in an integrated, interdisciplinary context.
Accessibility and satisfaction
Britons reported the highest overall levels of accessibility for family doctors; accessibility scores were influenced by the large majority (92%) of participants who received house calls. Because the data were collected before the new changes in primary care contracting in Great Britain, these numbers may be higher than what would currently be found. Again, this highlights the impact of health delivery models on the receipt of health care.
Overall Americans were the most likely to report physical accessibility of both office space and equipment. This finding speaks to the effectiveness of disability groups and activism, and the impact of national level legislation, such as the American with Disabilities Act (ADA)37 and the UK Disability Discrimination Act38 (DDA), both of which place various duties on service providers to ensure that the goods, facilities and services are accessible to disabled people. However, the duty to make ‘reasonable adjustments’ toward accessibility has been open to interpretation. Furthermore, the DDA does not have the enforceability (and thus the impact) of the ADA on accessibility. In Canada, no disability-specific federal legislation exists to ensure access for people with disabilities. Instead, the federal Human Rights Code and the Charter of Rights and Freedoms ensure equity and protection of the rights of disabled people. Provincial legislation is in place in only one province. The Accessibility for Ontarians with Disabilities Act (2005)39 has recently been enacted to provide enforceable access standards; however, the implementation timeline for primary care delivery has not been established.
Although the HCQ focused on physical barriers, accessibility is often more complex and subtle than purely physical parameters. In addition to the elimination of physical barriers, access requires the attitudes of service providers and office staff be inclusive and respectful of differences. Further, it requires that they have a reasonable level of expertise about the nature and consequences of disability. As discussed earlier, knowledge and attitudes encountered by people with disabilities among health professionals may also affect how they navigate the health-care system.
Individuals with long-term spinal cord injury were generally satisfied with the care provided by both their family physicians and rehabilitation specialists. Despite the differences in the way services are provided and the frequency in which they are received, there was essentially no significant difference in the levels of satisfaction both among countries and between the provision of family doctor care and spinal injuries specialist care.
Given the variability of service utilization among countries, a difference in satisfaction levels was anticipated. The lack of difference may be attributable to a number of issues. One possibility is that the disparity in services received may not represent critical services. For example, despite only 10% of Britons receiving counselling services, individuals may not deem these services as essential; therefore, not receiving them does not decrease satisfaction levels. Alternatively, it may be that a positive rapport with a physician may act as a buffer to dissatisfaction with the quality of service provided. The shortage and maldistribution of physician human resource may also inhibit people from reporting dissatisfaction with primary care. In areas where it is difficult to obtain service, individuals may simply feel grateful for having a family physician, and expectations of service may be low. Finally, the satisfaction questions did not address elements of care that may be impacted by the different service delivery models, for example, satisfaction with payment methods, coordination of services, provision of necessary equipment or knowledge of spinal cord injury issues. Whatever the explanation in this case, this finding is consistent with the literature, which typically reports high levels of health-care satisfaction. Given what is at stake, it may be simply that individuals have difficulty acknowledging if the health care they receive is not satisfactory.
Blendon et al29 examined satisfaction with the health-care system among sicker adults in five countries. Canadians and Britons identified shortages of health professionals and hospital beds, and waiting times as their two biggest problems. In contrast, high costs of health care and inadequate coverage of services were the two greatest concerns of Americans. These results suggest the service delivery model impacts on the satisfaction of the overall provision of service rather than the day-to-day care received. Results from previous studies found a shortage of clinical readmissions in specialized spinal injuries units in the UK.7 If the same is true of the spinal outpatient services, this, together with waiting times, could at least partly explain why Britons tended to use spinal injury specialists less than Canadians and Americans.
Conclusion
People with spinal cord injuries appear to develop complex maps of service provision to help them navigate the health-care system and obtain appropriate primary and preventive health services. Whereas there is overlap in service between the family doctors and spinal injuries specialists, there is also a lack of attention to lifestyle, function and emotional issues. Given the differences among countries, it is clear that the health-care delivery model plays an important role in how and where individuals receive health services.
References
Dejong G . Primary care for persons with disabilities: an overview of the problem. Am J Phys Med Rehab 1997; 76: S2–S8.
Francisco GE, Chae JC, DeLisa JA . Psychiatry as a primary care specialty. Am J Phys Med Rehab 1995; 4: 186–192.
O’Day B, Dautel P, Scheer J . Barriers to healthcare for people with mobility impairments. Manag Care Quart 2002; 10: 41–51.
Graham A, Savic G, Gardner B . Cervical and breast cancer screening in wheelchair dependent females. Spinal Cord 1998; 36: 340–344.
Heath GW, Fentam FH . Physical activity among persons with disabilities – a public health perspective. Exerc Sport Sci Rev 1997; 25: 195–243.
Dryden DM et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004; 42: 513–525.
Savic G, Short DJ, Weitzenkamp D, Charlifue S, Gardner BP . Hospital readmissions in people with chronic spinal cord injury. Spinal Cord 2000; 38: 371–377.
Starfield B, Cassady C, Nanda J, Forrest CB, Berk R . Consumer experiences and provider perceptions of the quality of primary care: implications for managed care. J Fam Pract 1998; 43: 216–226.
American Academy of Family Physicians. Retreived December 15, 2005 from http://www.aafp.org/online/en/home/policy/policies/f/familymedicine.html.
McColl MA et al. Access and quality of primary care for people with complex health needs: a comparison of three payment models. Final report submitted to the Primary Health Care Transition Fund, Ontario Ministry of Health and Long-Term Care, 2005.
Grumbach K, Selby JV, Scmittdiel JA, Quesenberry Jr CP . Quality of primary care practice in a large HMO according to physician specialty. Health Serv Res 1999; 43: 485–499.
Marsh GW . Measuring patient satisfaction outcomes across provider disciplines. J Nurs Manage 1999; 7: 47–62.
McColl MA, Shortt SED, Boyce W, James A . Making disability policy: evaluating the evidence base. In: Potheir D, Develin R (eds). Critical Disability Theory: Essays in Philosophy, Policy and Law. UBC Press: Vancouver 2003.
Hanson KW, Neuman P, Dutwin D, Kasper JD . Uncovering the health challenges facing people with disabilities: the role of health insurance. Disabil Insur 2003; W3: W3553–W3565.
Iezzoni LI, Davis RB, Soukup J, O’Day B . Satisfaction with quality and access to health care among people with disabling conditions. Int J Qual Health Care 2002; 14: 369–381.
Batavia AI, DeJong G . Disability, chronic illness, and risk selection. Arch Phys Med Rehabil 2001; 82: 546–552.
Bockenek WL . Primary care for persons with disabilities: a fragmented model of care for persons with spinal cord injuries. Am J Phys Med Rehabil 1997; 76 (Suppl): S43–S46.
Meyer AR, Branch LG, Cupples A, Lederman RI, Feltin M, Master RJ . Predictors of medical care utilization by independently living adults with spinal cord injuries. Arch Phys Med Rehabil 1989; 70: 471–476.
Jarzynowska A, McColl MA, Shortt SED, James A . Unmet health needs among adults with disabilities in Canada. Can Med Assoc J (Fall) (in press).
McColl MA, Charlifue S, Glass C, Lawson N, Savic G . Aging, gender and spinal cord injury. Arch Phys Med Rehab 2004; 85: 363–367.
Rummery K, Eliis K, Davis A . Negotiating access to community care: perspectives of frontline workers, people with a disability and careers. Health Social Care Comm 1999; 7: 296–300.
Turner-Stokes L, Turner-Stokes T, Schon K, Turner-Stokes H, Dayal S, Brier S . Charter for disabled people using hospitals: a completed access audit cycle. J R Coll of Phys Lond 2000; 34: 185–189.
Anderson P, Kitchin R . Disability, space and sexuality: access to family planning services. Social Sci Med 2000; 51: 1163–1173.
Chan L et al. Do medicare patients with disabilities receive preventive services? A population-based study. Arch Phys Med Rehabil 1999; 80: 642–646.
Nosek MA, Howland CA . Breast and cervical cancer screening among women with physical disabilities. Arch Phys Med Rehabil 1997; 78 (Suppl 5): S39–S44.
Bowers B, Esmond S, Lutz B, Jacobson N . Improving primary care for persons with disabilities: the nature of expertise. Disabil Society 2003; 18: 443–455.
Veltman A, Stewart DE, Tardif G, Branigan M . Perceptions of primary healthcare services among people with physical disabilities. Part 1: access issues. Medscape Gen Med 2001; 3: 18.
Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K . Common concerns amid diverse systems: health care experiences in five countries. Health Affairs 2003; 22: 106–121.
Rimmer JH . Health promotion for people with disabilities: the emerging paradigm shift from disability prevention to prevention of secondary conditions. Phys Ther 1999; 79: 495–502.
McColl MS, Charlifue S, Glass C, Savic G . An international study of aging on spinal cord injury: final report to Ontario Neurotrauma Foundation, 2003.
Bowers B, Esmond S, Lutz B, Jacobson N . Improving primary care for persons with disabilities: the nature of expertise. Disabil Soci 2003; 18: 443–455.
Illis LS . The case for specialist units. Spinal Cord 2004; 42: 443–446.
Lamarch PA, Beaulieu MA, Pineault R, Contandriopoulos Denis JL, Haggerty J . Choices for change: the path for restructuring primary healthcare services in Canada. Canadian Health Services Research Foundation, 2003; 1–38. Retrieved May 27, 2004 from http://www.chsrf.ca/final_research/commissioned_research/policy_synthesis/pdf/choices_for_change_e.pdf.
Koopman RJ, May KM . Specialist management and coordination of ‘out-of-domain care’. Fam Med 2004; 36: 46–50.
Rosenblatt RA, Hart G, Baldwin LM, Chan L, Schneeweiss R . The generalist role of specialty physicians. JAMA 1998; 279: 1364–1370.
Light DW . Universal health care: lessons from the British experience. Am J Pub Health 2003; 93: 25–30.
ADA (1990). One Hundred First Congress of the United States of America. Retrieved May 31, 2005 from http://www.sba.gov/ada/adaact.txt.
Department for Work and Pensions. Disability Discrimination Act (2005). Retrieved July 5, 2005 from http://www.disability.gov.uk/legislation/dda/dda.asp.
Ontario Ministry of Citizenship and Immigration (2005). Accessibility for Ontarian's with Disabilities Act. Retrieved May 31, 2005 from http://www.ontla.on.ca/library/bills/381/118381.htm.
Acknowledgements
This project was supported financially by the Ontario Neurotrauma Foundation. We thank all the participants in the International Study, Aging and Spinal cord injury.
Author information
Authors and Affiliations
Appendix A1. Health Care Questionnaire
Appendix A1. Health Care Questionnaire
(adapted from Grumach, Selby, Schmittdiel and Quesenberry, 1999; Marsh, 1999)
Please see next page for Questionnaire
UTILIZATION

ACCESS

SATISFACTION

Rights and permissions
About this article
Cite this article
Donnelly, C., McColl, M., Charlifue, S. et al. Utilization, access and satisfaction with primary care among people with spinal cord injuries: a comparison of three countries. Spinal Cord 45, 25–36 (2007). https://doi.org/10.1038/sj.sc.3101933
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101933
Keywords
This article is cited by
-
Identifying prescribers of antibiotics in a primary care spinal cord injury cohort
Spinal Cord Series and Cases (2024)
-
Exploring caregivers’ perceptions of community-based service requirements of patients with spinal cord injury: a qualitative study
BMC Primary Care (2023)
-
Examining the impact of COVID-19 on health care utilization among persons with chronic spinal cord injury/dysfunction: a population study
Spinal Cord (2023)
-
Health care and rehabilitation services utilization, benefits and satisfaction: a community survey of individuals with spinal cord injury in Thailand
Spinal Cord (2022)
-
First contact of care for persons with spinal cord injury: a general practitioner or a spinal cord injury specialist?
BMC Family Practice (2021)