Abstract
Study design:
Retrospective study.
Objective:
To examine the functional results and effect on quality of life of continent cutaneous urinary diversion in spinal cord injured patients.
Setting:
Department of Urology, Sahlgrenska University Hospital, Göteborg, Sweden.
Subjects:
A total of 10 patients with spinal cord injury (SCI).
Method:
The patients were operated on with an ileal reservoir (Kock reservoir or T-pouch), Cr-EDTA clearance was determined preoperatively and at follow-up. The patients answered a questionnaire concerning reservoir function, various activities and quality of life. The patient charts were reviewed.
Results:
One patient died of pulmonary embolism 3 years after surgery. Two patients were reoperated on for reservoir perforation. All patients were satisfied/very satisfied with their reservoirs. Half of them reported improved ability to perform various activities. Eight out of nine patients reported improved quality of life.
Conclusion:
For a selected group of patients with SCI, continent cutaneous urinary diversion provides successful outcome with improved quality of life.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) may cause a neurogenic bladder disorder resulting in either a hyper-reflexive or an atonic bladder depending on the level of the damage. Today, clean intermittent catheterization (CIC) is the standard bladder-emptying regimen for both types of neurogenic bladder, provided the patients can perform CIC themselves. However, the CIC regimen does not work for all patients, for example, due to reduced hand function or treatment-refractory urinary leakage between the catheterizations. Furthermore, in order to be able to live an active life, SCI women must be able to perform CIC sitting in a wheelchair. This requires some active grip function and trunk stability. In these patients an indwelling urethral catheter or a suprapubic catheter might be an alternative, especially for older patients.
For some of the patients where the CIC regimen does not work, some kind of urinary diversion might be appropriate. A diversion with a Bricker conduit has sometimes been used but requires an external urine-collecting device which younger patients are reluctant to have. Furthermore, conduit diversion in patients with neurological disorders has a bad reputation due to a high incidence of renal unit deterioration, at least in older materials.1
Continent cutaneous urinary diversion either with an intestinal reservoir or with a catheterizable vesicostomy combined with an augmentation ileocystoplasty, might be considered for younger patients that cannot perform urethral CIC and/or have treatment-refractory incontinence. The present article summarizes our results from a consecutive series of patients with SCI, who have been operated on with an ileal reservoir for continent cutaneous urinary diversion.
Materials and methods
From March 1997 to April 2004 ten patients with SCI underwent continent urinary diversion, either with a Kock reservoir (six patients) with two intussuscepted nipple valves (K+K), a cutaneous double-T-pouch (one patient) (T+T) or a combination of these two operations with an intussuscepted nipple valve for the continence nipple and a serous-lined extramural ileal valve for reflux protection (three patients) (T+K).2, 3, 4 All patients were examined with Cr-EDTA clearance and cystometry before diversion.
The data for the 10 patients are summarized in Table 1. Five of the patients were females and five males. The age at operation was 26–64 years (average 41.6 years). Six patients had a cervical injury and four a thoracical SCI. One tetraplegic patient due to cervical lesion also had a lumbal lesion. All patients were confined to a wheelchair. All but one had an upper motor neuron lesion. Trauma was the most common reason for spinal cord damage. The time between operation and analysis was 0.5–7.5 years (average 3.2 years). The reason for urinary diversion was that the patients were dissatisfied with their previous bladder regimen due to difficulty performing CIC and/or incontinence.
The patients were followed regularly at our outpatient ward at least once a year. Cr-EDTA clearance was determined annually or biannually. At the time of follow-up, the patients were asked to answer a questionnaire with specially constructed questions concerning reservoir function, impact of diversion on quality of life and various forms of activity. The patients who were at risk of developing autonomic dysreflexia (AD), that is, had a level of lesion above T5 (n=6), were asked about the incidence of AD before and after operation.5
Results
At 3 years after diversion one patient died due to a pulmonary embolism. According to the patient’s records the reservoir was functioning well at the time of her death. The nine surviving patients answered the questionnaire. Results concerning reoperations performed, reservoir function and GFR are given in Table 2. Two patients had been reoperated on due to reservoir perforation. One of the patients was reoperated on three times. The perforations occurred during the night. The patient currently has an indwelling catheter during the night and performs self-catheterization during the day. Seven of the patients can catheterize their reservoir themselves. Seven patients never have or seldom have leakage, while one patient sometimes has slight leakage requiring a change of compress over the stoma. One patient with a cutaneous double-T-pouch leaks continuously and requires a bag over the stoma. One patient often experiences catheterization problems and one sometimes. All patients have their natural urinary bladder still in place. Five patients experience problems with their native bladder and require catheterization and rinsing now and then.
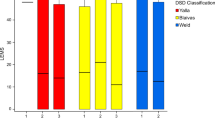
Six of the patients claim that they are very satisfied and three that they are satisfied with their reservoirs. All claim that their reservoirs function very well (five patients) or well (four patients). Even the patient with reservoir leakage is satisfied since her situation has improved a great deal compared with preoperatively, when she suffered from urethral leakage to pads. She does not want to undergo reoperation. The opinions of the patients concerning the way diversion had influenced different aspects of their life are presented in Figures 1, 2, 3, 4 and 5. Half of the patients report a positive effect of the operation on their working capacity and ability to perform daily activities and leisure activities (Figures 1, 2 and 3). Eight of the nine patients report that the diversion has improved their quality of life and consequently state that the operation should have been performed earlier (Figures 4 and 5).
Five of the six patients at risk of developing AD reported episodes of AD before the operation. These episodes had decreased in magnitude and frequency after operation. Two patients reported that detritus in the remaining bladder could elicit the reaction.
Discussion
The present study summarizes the long-term results after continent cutaneous urinary diversion in 10 patients with SCI due to various disorders. Eight of the surviving nine patients have reservoirs that are functioning well. All patients greatly appreciate their diversion although one patient has a leakage that requires a bag over the stoma and one patient requires reservoir drainage during the night. The kidney function was normal at follow-up in all patients.
The present, 10 patients represent only a small fraction of the patients with SCI treated at our hospital. Although most patients had a cervical lesion, hand function sufficient to permit self-catheterization of the reservoir by the patient was considered mandatory for diversion. However, since it is easier to catheterize a stoma on the abdomen, this implies that a SCI subject who cannot use CIC may be able to perform catheterization of a reservoir independently. A common comment was: ‘Why was this operation not performed earlier’.
The most striking result of the present analysis was the reported positive effect of the operation on the patients’ quality of life. Similarly, Zommick et al6 found that 80% of 21 patients with cervical SCI reported improved quality of life after various forms of continent urinary diversion.
Perforation of the reservoir occurred in two patients. This is a serous complication with an incidence of a few per cent after all types of intestinal reservoir for urine storage.7 It often occurred during the night since this is the longest interval between emptying of the reservoir. Theoretically, the risk of perforation during the night is higher for patients in a wheelchair as some of these patients have problems with water retention in the legs during the day. When sleeping in the supine position this accumulated water is redistributed to the blood and excreted in the kidneys, leading to even higher night time urine volumes. The sensations from the reservoir calling for emptying are weaker than the normal afferent signals from the native bladder. This is probably even more evident in patients with SCI. It is thus of utmost importance to inform these patients of the risk of perforation and to recommend reduced fluid intake before going to bed. The volume of the morning urine should be observed and if it is high extra emptying during the night or an indwelling reservoir catheter should be recommended.
What alternatives could be offered to those patients? An incontinent diversion, such as a Bricker conduit, was not considered appropriate due to the low age of the patients. Nine of the 10 patients had an overactive bladder and the main reason for the diversion was incontinence that was not effectively treated with anticholinergic drugs. A further reason for diversion in several patients was difficulty performing CIC due to reduced hand function and that the patient was in a wheelchair. An alternative to performing continent cutaneous urinary diversion in these patients would be an ileocystoplasty combined with a catheterizable suprapubic vesicostomy. This is the most logical alternative to diversion with a Kock reservoir for the patients included in the present study.
Table 3 summarizes the arguments favouring either continent cutaneous diversion or augmentation ileocystoplasty combined with an abdominal stoma. The latter procedure is a smaller operation and there is no need for a new anastomosis between the ureters and the bladder since the trigone is preserved. The remaining urethra could be associated with a risk of leakage but could also reduce the risk of perforation that occurred in two of the present patients. The prevalence of a natural safety valve against high pressure, however, does not completely eliminate the risk of perforation since this complication also occurs in patients with orthotopic bladders after cystectomy for bladder carcinoma.7
Patients with a level of lesion above T5 run the risk of developing AD – a syndrome characterized by a generalized vasoconstriction below lesion level, inducing a huge increase in blood pressure, sweating above the lesion level and a pounding headache.8, 9 The reaction is elicited by stimuli arising below the lesion level and irritations in the urinary bladder are very potent stimuli for this generalized reaction.5 Patients troubled by this complication are also prone to it after ileocystoplasty since the bladder is still within the urological system after the first procedure but not after continent urinary diversion. Our study showed that the episodes of AD had decreased in magnitude and frequency, even though the remaining bladder could be a problem. The AD reaction might be dangerous and serious complications, such as epileptic seizures, cerebrovascular events and pulmonary oedema, have been reported.
Several patients with SCIs have partial lesions that only comprise the efferent nerve to the bladder, which means that some bladder sensitivity remains. Scopies of the augmented bladder necessitated by, for example, bladder stones are prone to be more painful in patients with an ileocystoplasty than in patients with a continent ileal reservoir, valid for patients with a neurogenic bladder disorder.
After diversion with a Kock reservoir, the patients catheterize the outlet with a rather thick catheter – usually Charrière 24 – while patients with Mitrofanoff outlets use thinner catheters. The thick catheters are easier to handle for patients with impaired hand function due to high spinal lesions. In recent years there has been a debate regarding whether clam cystoplasty is associated with an increased risk of carcinoma due to the long line of anastomoses between the bladder wall and the intestine.10 Up to now, 22 cases of carcinoma have been reported in patients with ileocystoplasty. It remains to be elucidated whether this incidence is valid for patients with neurogenic bladder disorders.
All these pros and cons need to be considered for the individual patient. For some patients with, for example, pronounced autonomic dysreflexia, the continent cutaneous reservoir appears to be most suitable while for others ileocystoplasty might be a better alternative. The conclusion to be drawn from our consecutive patient study is that continent cutaneous urostomy works well for these patients and improves their quality of life. Reasonably, these procedures should be performed more frequently than is the case today.
References
Koziol I, Hackler RH . Cutaneous ureteroileostomy in the spinal cord injured patient: a 15-year experience. J Urol 1975; 114: 709–711.
Kock NG, Nilson AE, Nilsson LO, Norlén LJ, Philipson BM . Urinary diversion via a continent ileal reservoir: clinical results in 12 patients. J Urol 1982; 128: 469–475.
Abol-Enein H, Ghoneim MA . Serous lined extramural ileal valve: a new continent urinary outlet. J Urol 1999; 161: 786–791.
Stein JP, Skinner DG . T-mechanism applied to urinary diversion: The orthotopic T-pouch ileal neobladder and cutaneous double-T-pouch ileal reservoir. Tech Urol 2001; 7: 209–222.
Karlsson AK . Autonomic dysreflexia. Spinal Cord 1999; 37: 383–391.
Zommick JN, Simoneau AR, Skinner DG, Ginsberg DA . Continent lower urinary tract reconstruction in the cervical spinal cord injured population. J Urol 2003; 169: 2184–2187.
Månsson W et al. Perforation of continent urinary reservoirs: Scandinavian experience. Scand J Urol Nephrol 1997; 31: 529–532.
Karlsson AK, Friberg P, Lonnroth P, Sullivan L, Elam M . Regional sympathetic function in high spinal cord injury during mental stress and autonomic dysreflexia. Brain 1998; 121: 1711–1719.
Gao SA, Ambring A, Lambert G, Karlsson AK . Autonomic control of the heart and renal vascular bed during autonomic dysreflexia in high spinal cord injury. Clin Auton Res 2002; 12: 457–464.
Ali-El-Dein B, El-Tabey N, Abdel-Latif M, Abdel-Rahim M, El-Bahnasawy MS . Late uro-ileal cancer after incorporation of ileum into the urinary tract. J Urol 2002; 167: 84–88.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pazooki, D., Edlund, C., Karlsson, AK. et al. Continent cutaneous urinary diversion in patients with spinal cord injury. Spinal Cord 44, 19–23 (2006). https://doi.org/10.1038/sj.sc.3101811
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101811
Keywords
This article is cited by
-
Long-Term Outcomes of Augmentation Enterocystoplasty with a Catheterizable Channel in the Adult Neurogenic Population
Current Bladder Dysfunction Reports (2013)
-
Urological rehabilitation of spinal cord injury patients
ArgoSpine News & Journal (2007)