Abstract
Study Design: Study of reusable catheter.
Objective: To investigate whether a silicone cathether reused over years for clean intermittent catheterization (CIC) was safe for spinal cord injured (SCI) men.
Setting: Maharaj Hospital, Chiang Mai, Thailand.
Method: A cross-sectional study was obtained from SCI men who had used CIC with a reusable silicone catheter for more than a year. Demographic data, urological management and urinary tract complications focusing on the radiologic status of the urethra were reviewed and analyzed. In addition, two reused and one new catheters were studied under electron microscope for catheter morphology (surface and lumen) and stiffness.
Results: There were 28 SCI men included in this study. The average duration of CIC use was 4.8 years and the average time of usage for each catheter was 3 years (range 1–7 years). In all, 26 men previously used indwelling catheterization (ID) during the acute phase. In all, 23 men performed self-catheterization. Regarding urinary complications, three reported urethral bleeding, five had episodes of pus per urethra, five had epididymitis, four had passing stones, 18 had occasional foul smelly urine, 10 developed fever and cloudy urine during the past year. Of 17 patients who had ultrasonography done, four had pathologic findings in kidney and one had bladder calculi. Demographic data, urinary management and complications did not have significant relation to the abnormality of the urethrogram or urinary tract infection. However, where the frequency of CIC was higher, the abnormality of the urethra was lower (P<0.05). All had serum Cr level ⩽1.3 mg/dl. Electron microscopic findings of reused catheters for 2 years revealed encrustation but no obstruction in the lumens and 20% increase in stiffness.
Conclusion: The clinical outcome, especially with regard to urethral abnormalities with this reusable silicone catheter is as good as with a disposable one. However, to reuse urinary catheters, one should consider the increasing risk of infection. For SCI patients in developing countries, CIC with a reusable silicone catheter may be a suitable and safe choice if one cleans and applies it properly to reduce infection. In order to answer the question how long a person in a developing country should use the same silicone catheter, further research should be conducted.
Similar content being viewed by others
Introduction
Nowadays clean intermittent catheterization (CIC) is widely accepted as the first line in management of patients with neurogenic bladder dysfunction and unbalanced voiding. So far, various urethral catheters have been introduced to the markets.1 Disposable catheters either with self-lubrication or in connection with jelly injected into the urethra, are used to minimize urethral trauma and infection. They increase ease of use during catheterization.2, 3, 4, 5 Owing to the high cost for long-term use the disposable ones are limited to people in developed countries.6
In Thailand, a reusable silicone catheter for self-catheterization from Japan has been introduced for a decade. Many SCI patients with neurogenic bladder and unbalanced voiding had reused the same catheter for years due to economic reason. They found it safe and easy to handle. We therefore studied whether this reused silicone catheter was really safe enough for SCI men, whether it caused any significant urinary tract infection and if so, which factors were related to such.
Materials and methods
SCI men who had applied CIC or clean intermittent self-catheterization (CISC) at least twice a day for more than a year were included in this study. All gave verbal consent before the study was done. Demographic data, urinary management, physical examination, urethrography, ultrasonography, serum Cr and CCr were reviewed and analyzed by using Epi-info. In addition, electron microscopic study was undertaken to examine two reused and one new catheters.
Results
Demographic data and urological management
There were 28 males; four tetraplegics, 23 paraplegics and one with neurogenic bladder only; 20 with ASIA/IMSOP classification A or B and 8 with C or D. Table 1 shows demographic, urological management and statistical data of all 28 patients. The average duration of post onset was 73 months or 6 years. In all, 26 men had ID during the acute phase with the average duration of ID use of 6.5 weeks. In all, 24 men had used CIC for more than 2 years, with the average duration of CIC use of 4.8 years, the average time of usage for each catheter of 35 months or 3 years and the average CIC frequency of four times per day (see Table 1). A total of 23 men performed CISC. A total of 18 men had reflex voiding in between catheterizations and 13 of them used condom catheter (CC).
Outcome and complications
All had serum Cr level ⩽1.3 mg/dl (range 0.5–1.3) and all 28 patients had a CCr (ml/min) ⩾95. Three out of 28 (11%) reported an episode of urethral bleeding when catheterizing. Four (14%) did not apply lubrication (jelly); however, none reported difficulties with catheterization. Five (18%) reported an episode of urethritis (pus per urethra), five (18%) had symptoms suggesting epididymitis; four (14%) had passing stones; 18 (64%) had occasional foul smelly urine; and 10 (36%) developed fever with cloudy urine, suggesting urinary tract infection (UTI) during the past years. Regarding the latter, six out of 10, had two–three episodes per year. Six out of 28 (21%) did not report any signs or symptoms of infection or urethral problems during the past year, and five of them did CIC themselves. Three (11%) had an old scar at the shaft of the penis due to CC. According to Table 2, none of demographic data and urinary management were significantly related to clinical UTI.
Regarding urethrographic findings, there were 20 men (70%) with normal urethral outline and eight (30%) with minor abnormalities, that is, three (11%) with irregularity, four (15%) with narrowing that did not need treatment, and only one (4%) with stricture at the penile urethra. Among those with normal urethrograms, two had reused the catheter for 7 years.
Table 2 also shows the demographic and urological data in relation to urethrograms. No factors were related to abnormal except daily frequency of CIC. The higher the daily frequency of CIC was, the less abnormal the urethra was found (P<0.05). Those with abnormal urethrogram had longer durations of CIC use and of post onset than those with normal urethrogram but the differences were not significant (P>0.05). In addition, abnormal urethrograms were not found in those who performed CIC/CISC for more than four times per day.
Among 28 patients, 17 had ultrasonography of the upper and the lower urinary tract. Overall, 12 (71%) had normal size and echogenicity of the kidneys. Those with abnormalities were as follows: two mild hydronephrosis, one mild pelvocalyceal dilatation with small renal stones, one focal thinning of parenchyma and one multiple bladder calculi.
Electron microscopic findings
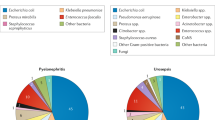
Figure 1 shows electron microscopic findings of a new and two reused catheters. There was some degree of encrustation in the lumen with rather smooth outer surface of the two reused catheters when compared to the new one. In addition, the reused catheters had about 20% increase in stiffness.
Discussion
According to the previous review of urethral catheters used for intermittent catheterization, there is no one best material or technique. Materials and techniques chosen depend mainly on patients' preference and economic reason. Owing to high cost of hydrophilic catheters or disposable catheters used in combination with jelly, the usage of such catheters are limited to people in developed countries only. In regard to socioeconomics, the reusable silicone catheter has advantage over the hydrophilic ones. Its cost is about 16–25 USD per catheter, much less when compared to the yearly cost of the disposable catheters.6
This study shows that CIC/CISC with a reusable silicone catheter did not cause significant damage to the urethra or the upper tract. The prevalence of urethral stricture in this study was about 4% which is close to 3.7% of Guenther et al7 where disposable catheters in combination with jelly were used for long-term CIC. According to Guenther's study,7 a previous period of ID appeared to relate to the later changes of the urethra. In our study, 26 out of 28 SCI men had ID during the acute phase and only one of them had urethral stricture. This does not support the findings of Guenther et al7 but does support the study of Jacobs and Kaufman (1978)8 that ID during the acute phase is not a cause of urethral stricture but claimed to be due to a long-term use of ID. Moreover, in those with abnormal urethrograms, the mean duration of CIC/CISC usage was about 6 years and of postonset was about 10 years. This supports the study of Wyndaele and Maes (1990) who did a 12 year follow-up of SCI patients using CISC. They found that urethral stricture occurred in those using CISC for more than 5 years.2 In addition, the higher the daily frequency of catheterization, the less the urethral changes. This might be due to the fact that those regularly performing CIC developed more skill in catheterization and therefore had less chance of urethral trauma. Moreover, with more catheterizations the chance of urethral dilatation increases. According to our study, CIC/CISC four times or more per day seems to be proper and safe for SCI men in long term.
Regarding urinary outcome and infection, creatinine level of the patients in this study were within normal ranges despite a high incidence of foul smelly urine (64%) and fever with cloudy urine (36%) reflecting significant evidences of clinical UTI. On this behalf, we have to consider that serum creatinine level becomes pathologic only when the kidney function is reduced to about 30% or less. However, all 28 patients had a normal creatinine clearance ⩾95 ml/min. Table 3 shows that the infection rates in this study were higher than those in the prospective study of Wyndaele et al5 and the randomized crossover study of Giannantoni9 using disposable catheters. Perhaps, the higher infection rates were due to a longer retrospective period of this study. When compared to two other long-term retrospective studies of Waller et al4 and Bakke and Vollset10 using disposable hydrophilic catheters, the infection rates seemed not much different. It is difficult to estimate the costs of antibiotics taken by in this study. However, the enormous cost difference between using disposable catheters and this reusable silicone catheter, as shown in Table 3, one might assume that to use such silicone catheters over months and years is cost effective. Moreover, regarding the findings of kidney morphology and kidney function, it can be regarded as safe.
Concerning a proper time that each silicone catheter should be discarded, in Japan it is commonly reused for only 2 weeks6 while in this study the average time of each cathether usage was 3 years. Table 2 shows that there were no differences in the mean age, the mean duration of postonset, the mean duration of CIC use and the mean time of each catheter usage between those with and without febrile UTI. For long-term management, besides proper daily frequency and technique of CIC/CISC, patients' compliance such as ability to properly perform CISC, mental capability and self-discipline,11 it may be safer that one uses the silicone catheter for a shorter period of time; however, no exact time recommendation can be given so far.
Regarding disinfection technique, this reusable silicone catheter can be easily disinfected by soaking it in an antiseptic solution. According to the product monograph, it should be soaked in 0.02–0.05% benzethonium chlorite with sterile glycerine in solution. Chlorhexidine or iodine contained disinfectant is not recommended as they may damage the catheter tip. At present our patients use savlon solution (chlorhexidine 1.5% and cetrimide 15%) with a concentration of 1:100 and change it twice a week; and there have been no reports of the catheter tip damage. According to the electron microscopic findings, SCI persons should be encouraged to forcefully rinse the catheter lumen with a high-speed tap water to minimize encrustation. To boil it every now and then as recommended in the monograph may help but may cause more stiffness.
In conclusion, for SCI persons who need long-term CIC/CISC in developing countries, to reuse a silicone self-catheter seems acceptable due to low cost and ease of use. To reduce catheter-induced infection, a shorter time of usage seems to be desirable and techniques of CIC, cleansing and disinfection should be properly done. In addition, for a stronger conclusion whether reusing such a silicone catheter is safe and that the low costs of these silicone catheters outweigh the possibility of higher rates of UTI compared to disposable catheters, a randomized controlled trial study should be conducted. Up to now, the alternative to the long-term use of this silicone catheter for CIC in a developing country would be an indwelling catheter with its well-known disastrous outcome.
References
Madersbacher H, Wyndaele JJ, Igawa Y, Chancellor M, Chartier-Kastler E, Kovindha A . Conservative management in neuropathic urinary incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A (eds). Incontinence, 2nd edn. Plymouth: Health Publication Ltd 2002, pp 697–754.
Wyndaele JJ, Maes D . Clean intermittent self-catheterisation – a 12-year follow-up. J Urol 1990; 143: 906–908.
Vaidyanathan S, Soni BM, Dundas S, Krishnan KR . Urethral cytology in spinal cord injured patients performing intermittent catheterisation. Paraplegia 1994; 22: 493–500.
Waller L, Jonsson O, Norlen L, Sullivan L . Clean intermittent self-catheterization in spinal cord injury patients: long-term follow-up of a hydrophilic low friction technique. J Urol 1995; 153: 345–348.
Wyndaele JJ, De Ridder D, Everaert K, Heilporn A, Congard-Chassol B . Evaluation of the use of Urocath Gel catheters for intermittent self-catheterization by male patients using conventional catheters for a long time. Spinal Cord 2000; 38: 97–99.
Madersbacher H et al. Conservative management in the neuropathic patient. In: Abrams P, Khoury S, Wein A (eds). Proceeding of the First International Consultation on Incontinence. Plymouth: Health Publication Ltd 1999, pp 775–812.
Guenther M, Loechner-Ernst D, Kramer G, Stoehrer M . Intermittent cathetherisation in neurogenics: no harm to the urethra. In: The Final Program & Abstract Book of the 39th Annual Scientific Meeting of the International Medical Society of Paraplegia 2000, pp 11 (abstract).
Jacobs SC, Kaufman JM . Complications of permanent bladder catheter drainage in spinal cord injury patients. J Urol 1978; 119: 740–741.
Giannantoni A, Di Stasi SM, Scivoletto G, Virgill G, Dolci S, Porena M . Intermittent catheterization with a prelubricated catheter in spinal cord injured patients: a prospective randomized crossover study. J Urol 2001; 166: 130–133.
Bakke A, Vollset S . Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent caheterization. J Urol 1993; 149: 527–531.
Diokno AC, Sonda PL, Hollander JB, Lapides J . Fate of patients started on clean intermittent self-catheterization therpay 10 years ago. J Urol 1983; 129: 1120–1122.
Acknowledgements
Thanks to Medical Service Company (Germany) for the electron microscopic examination and supporting this research study.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kovindha, A., Mai, W. & Madersbacher, H. Reused silicone catheter for clean intermittent catheterization (CIC): is it safe for spinal cord-injured (SCI) men?. Spinal Cord 42, 638–642 (2004). https://doi.org/10.1038/sj.sc.3101646
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101646
Keywords
This article is cited by
-
Cross-sectional internet survey exploring symptomatic urinary tract infection by type of urinary catheter in persons with spinal cord lesion in Japan
Spinal Cord Series and Cases (2023)
-
The temporal burden of preparing catheters for re-use in adults with spinal cord injury: a cross-sectional study
Spinal Cord Series and Cases (2023)
-
The microbiological and physical properties of catheters for intermittent catheterization: a systematic review on the impact of reuse and cleaning
Spinal Cord (2022)
-
Pulse article: survey of neurogenic bladder management in spinal cord injury patients around the world
Spinal Cord Series and Cases (2021)
-
Disability and sustainability: reusable versus single-use catheters for persons with neurogenic bladder due to spinal cord injury
Spinal Cord Series and Cases (2020)