Abstract
Study design: Case report.
Objectives: To report insidious development of autonomic dysreflexia and hydronephrosis due to dyssynergic voiding following discontinuation of intrathecal baclofen therapy.
Setting: Regional Spinal Injuries Centre, Southport, UK.
Methods: A male patient with paraplegia at T-5 (ASIA-A) had implantation of Medtronic Synchromed 8615 s programmable pump to control intractable spasms. After 4 years, the baclofen pump needed replacement because of battery exhaustion. At this time, he was taking oxybutynin 2.5 mg twice a day. He wore a penile sheath and performed intermittent catheterisation three times a day. Intravenous urography showed no dilatation of pelvicalyceal systems or ureters. During the course of the next 4 months, the dose of baclofen had to be increased gradually to 820 μg/day in order to control the spasms. Investigations revealed disconnection of the tube from the pump. The patient decided to undergo explantation of the pump and discontinue intrathecal baclofen therapy altogether. Following removal of the pump, he was prescribed baclofen 20 mg four times a day and diazepam 5 mg twice a day. He continued penile sheath drainage with oxybutynin 2.5 mg twice a day. Although spasms were controlled with oral baclofen and diazepam, he started getting transient, mild headache during reflex voiding. After nearly 2 years, he developed unbearable and pounding headache while passing urine.
Results: The dose of oxybutynin was increased to modified release formulation, 20 mg, once daily. He was prescribed modified release alfuzosin 10 mg once a day. Indwelling urethral catheter drainage was instituted. Intravenous urography showed dilation of left renal pelvis and calyces, and left ureter. After a fortnight, the dose of modified release oxybutynin was increased further to 25 mg once a day. After a month, he started performing self-catheterisation every 3 h and symptoms of autonomic dysreflexia subsided completely. A follow-up intravenous urography performed 6 months later, showed normal appearances of the left kidney.
Conclusion: Spinal cord injury patients, in whom intrathecal baclofen therapy is terminated, need close monitoring of their urological status. Medications, which are prescribed for neuropathic bladder, and the method of bladder drainage, may need suitable changes, as discontinuation of intrathecal baclofen therapy can result in reappearance of detrusor-sphincter dyssynergia in previously susceptible patients.
Similar content being viewed by others
Introduction
Although, intrathecal baclofen therapy is instituted primarily to control spasticity in the patients with spinal cord injury (SCI), chronic infusion of baclofen intrathecally exerts its influence upon vesicourethral function as well. Intrathecal baclofen abolished detrusor-sphincter dyssynergia in 40% of patients with severe spasticity due to spinal cord pathology.1 Therefore, it is reasonable to presume that discontinuation of intrathecal baclofen therapy may result in reappearance of detrusor-sphincter dyssynergia in previously susceptible patients.
Severe rebound spasticity, confusion, seizures and rarely life-threatening rhabdomyolysis, hyperthermia, or autonomic disturbances may occur when intrathecal baclofen therapy is terminated abruptly.2 In May 2002, the FDA and Medtronic added a boxed warning and strengthened the warning sections of the prescribing information of Lioresal Intrathecal. The warnings inform healthcare professionals about rare cases of intrathecal baclofen withdrawal that can lead to life-threatening after effects and/or death in the patients, who abruptly discontinue therapy. Dozens of patients have suffered high fevers, mental impairment and muscle rigidity leading to rhabdomyolosis and organ failure as a result of abrupt discontinuity of intrathecal baclofen. The FDA has received reports of six deaths associated with the sudden discontinuation of Lioresal Intrathecal.3, 4 Patients in whom intrathecal baclofen is discontinued, treatment with GABA-ergic agonist drugs such as oral or enteral baclofen and oral, enteral or intravenous benzodiazepines will prevent potentially fatal sequelae. Meythaler et al5 postulate that intrathecal baclofen withdrawal may be a form of serotonergic syndrome that occurs from loss of gamma-aminobutyric acid B receptor-mediated presynaptic inhibition of serotonin. These authors recommend cyproheptadine as a useful adjunct to baclofen and benzodiazepines in the management of acute intrathecal baclofen withdrawal syndrome.
Whereas the symptoms of abrupt withdrawal of intrathecal baclofen are dramatic, the effects of termination of intrathecal baclofen therapy upon vesicourethral function are insidious. Therefore, it is not commonly appreciated that vesicourethral function needs close monitoring in those spinal cord injury patients, in whom intrathecal baclofen therapy has been discontinued. We report a male patient, who developed urological complications quite insidiously, following termination of intrathecal baclofen therapy.
Case report
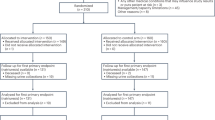
A 17-year-old male sustained complete paraplegia at T-5 level (ASIA impairment scale A) in a road traffic accident in 1988. He had indwelling urethral catheter drainage. In 1995, the indwelling catheter was removed. He was prescribed oxybutynin 5 mg three times a day and he performed self-catheterisation. In 1996, vesical calculus was detected during a routine review and electrohydraulic lithotripsy was performed. Bladder biopsy showed extensive nonkeratinising squamous metaplasia. There was basal hyperplasia of the epithelium, but no dysplasia or evidence of malignancy. Concretions were seen in the superficial stroma (Figure 1).
Histology of the bladder biopsy (H-2734/96) shows extensive nonkeratinising squamous metaplasia and mild nonspecific cystitis. Concretions are seen in the superficial stroma, undergoing trans-epithelial elimination. There is basal hyperplasia of the epithelium, but no evidence of dysplasia or malignancy
He had intractable spasms not amenable to oral baclofen therapy. Therefore, Medtronic Synchromed 8615s programmable pump was implanted in 1996 (Medtronic Ltd, Sherbourne House, Croxley Business Centre, Watford, UK). In 1997, there was recurrence of bladder stone, and electrohydraulic lithotripsy was carried out. Blood urea was 4.8 mmol/l; creatinine: 81 μmol/l. In 2000, the baclofen pump needed replacement because of battery exhaustion. Synchromed EL 8626L-18 pump was implanted.
At this time, he was taking oxybutynin 2.5 mg twice a day. He wore a penile sheath and performed intermittent catheterisation three times a day. Intravenous urography showed excretion of contrast by both kidneys. There was no dilatation of pelvicalyceal systems or ureters (Figure 2). Blood urea was 3.5 mmol/l; creatinine: 80 μmol/l. The dose of intrathecal baclofen was 300 μg per day, administered as a simple continuous infusion.
During the course of the next 4 months, the dose of baclofen had to be increased gradually to 820 μg per day in order to control the spasms. Investigations revealed disconnection of the tube from the pump. The patient decided to undergo explantation of the pump and discontinue intrathecal baclofen therapy altogether. Following removal of the pump in October 2000, he was prescribed baclofen 20 mg four times a day and diazepam 5 mg twice a day. He continued penile sheath drainage with oxybutynin 2.5 mg twice a day. Blood urea was 4.9 mmol/l; creatinine: 89 μmol/l.
Although the spasms were controlled with oral baclofen and diazepam, he started getting transient, mild headache during reflex voiding. The headache would subside completely after he had passed urine. After nearly 2 years, he developed unbearable and pounding headache while passing urine. His wife became concerned about his condition and sought medical advice from the spinal unit. Blood pressure readings were as follows:
The dose of oxybutynin was increased from 2.5 mg twice a day to modified release formulation of oxybutynin, 20 mg, once a day. He was prescribed modified release alfuzosin 10 mg once a day. Indwelling urethral catheter drainage was instituted. Intravenous urography showed dilation of left renal pelvis and calyces, and left ureter (Figure 3). Blood urea was 3.6 mmol/l; creatinine: 80 μmol/l. After a fortnight, the dose of modified release oxybutynin was increased further to 25 mg once a day. After a month, he started performing self-catheterisation every 3 h. No longer does he develop any symptom of autonomic dysreflexia. He continues to take modified release formulations of oxybutynin (25 mg) and alfuzosin (10 mg) a day. A follow-up intravenous urography, which was performed about 6 months later, showed normal appearances of the left kidney. There was marked loss of cortical thickness at the right upper pole with underlying calyceal scarring.
A 60 min film of intravenous urography (28 August 2003): The indwelling urethral Foley catheter has been unclamped allowing free drainage of urine from the bladder. So very little contrast is seen within the urinary bladder. But there is marked dilation of left renal pelvis, calyces and left ureter. Baclofen pump has been explanted
Discussion
After intrathecal baclofen was discontinued, this patient developed gradually dyssynergic voiding, which triggered off autonomic dysreflexia. Dyssynergic voiding resulted in dilation of left ureter, renal pelvis and calyces. Intravenous urography performed when the patient had symptoms of autonomic dysreflexia, showed that the patient had a small-capacity bladder with diverticula (Figure 4). This ruled out the possibility that the patient had been retaining large amounts of urine in the bladder and consequently developed dilatation of left pelvicalyceal system and ureter. When the method of bladder management was changed from reflex voiding to regular intermittent catheterisation with oral oxybutynin therapy (modified release formulation 25 mg once a day), dysreflexic symptoms disappeared. A follow-up intravenous urography performed about 6 months later, showed normal appearances of the left kidney, thus excluding other causes for dilatation of left pelvicalyceal system and ureter.
A 40 min film of intravenous urography (28 August 2003): The catheter had been clamped to allow filling of urinary bladder. Balloon of Foley catheter is seen within the urinary bladder. The bladder is of small capacity and vesical diverticula are present. There is dilation of left renal pelvis and calyces. Baclofen pump has been removed
This case illustrates the need to monitor bladder function after discontinuation of intrathecal baclofen therapy. Subsequent to termination of intrathecal baclofen therapy, these patients require a review of the medications, which are prescribed for neuropathic bladder, and the method of bladder drainage should be modified accordingly.
Although transurethral or transperineal injection of botulinum A toxin into the external sphincter may be effective for treatment of detrusor-sphincter dyssynergia,6 severe generalised muscle weakness has been reported after botulinum toxin injection in the detrusor.7 We believe that intermittent catheterisation with oral or intravesical8 pharmacotherapy to control detrusor hyperreflexia and detrusor-sphincter dyssynergia9 is the first choice of bladder drainage for these patients. When our patient started taking modified release formulations of oxybutynin and alfuzosin, symptoms of autonomic dysreflexia subsided. Together with intermittent catheterisation, pharmacotherapy consisting of an alpha-blocker (alfuzosin) and antimuscarinic (oxybutynin) led to restoration of normal appearances of left pelvicalyceal system in our patient. Athanasopoulos et al10 also found a combination treatment with an alpha-blocker (tamsulosin) plus an anticholinergic (tolterodine) improved quality of life in the patients with bladder outlet obstruction and concomitant detrusor instability.
Our patient developed recurrent bladder stones. Although this patient performed intermittent catheterisation most of the time, he used an indwelling catheter during some weekends or when he was going out. Indwelling catheters are prone to encrustations and these encrustations can lead to formation of bladder stones.11 Ord et al12 studied whether method of bladder management was associated with risk of bladder stone formation in spinal cord-injured patients by analysing the records of 457 patients admitted to Stoke Mandeville Hospital Spinal Injuries Centre between 1985 and 1990. The absolute annual risk of stone formation in the patients with a catheter was 4% compared with 0.2% for those on intermittent self-catheterisation. However, having formed a stone once, the risk of forming a subsequent stone quadrupled to 16% per year. In our patient, bladder biopsy, taken at the time of performing electrohydraulic lithotripsy in 1996, showed the presence of concretions in the superficial stroma (Figure 1). It is possible that the concretions acted as nidus for recurrence of vesical calculi. Another aetiological factor for vesical calculi in spinal cord injury patients, who manage their bladder by intermittent catheterisation, is stone formation around genital hair. Hair may be introduced inadvertently during urethral catheterisation. The hair acts as a nidus for encrustation and stone formation.13, 14, 15
In conclusion, spinal cord clinicians should remember that the urological status is not definitely stable in these patients, as discontinuation of intrathecal baclofen therapy can result in reappearance of detrusor-sphincter dyssynergia in previously susceptible individuals.
References
Steers WD, Meythaler JM, Haworth C, Herrell D, Park TS . Effects of acute bolus and chronic continuous intrathecal baclofen on genitourinary dysfunction due to spinal cord pathology. J Urol 1992; 148: 1849–1855.
Colachis SC, Rea GL . Monitoring of creatinine kinase during weaning of intrathecal baclofen and with symptoms of early withdrawal. Am J Phys Med Rehabil 2003; 82: 489–492.
Lioresal Intrathecal (Baclofen Injection): Overview. http://www.injuryboard.com/view.cfm/Topic=874.
The FDA Safety Information and Adverse Event Reporting Program – 2002 Safety Alert Lioresal (Baclofen Injection). http://www.fda.gov/medwatch/SAFETY/2002/baclofen.htm.
Meythaler JM, Roper JF, Brunner RC . Cyproheptadine for intrathecal baclofen withdrawal. Arch Phys Med Rehabil 2003; 84: 638–642.
Reynard JM, Vass J, Sullivan ME, Mamas M . Sphincterotomy and the treatment of detrusor-sphincter dyssynergia: current status, future prospects. Spinal Cord 2003; 41: 1–11.
Wyndaele JJ, Van Dromme SA . Muscular weakness as side effect of botulinum toxin injection for neurogenic detrusor overactivity. Spinal Cord 2002; 40: 599–600.
Reitz A, Schurch B . Intravesical therapy options for neurogenic detrusor overactivity. Spinal Cord 2004; 42: 267–272.
Bennett JK et al. Terazosin for vesicosphincter dyssynergia in spinal cord-injured male patients. Mol Urol 2000; 4: 415–420.
Athanasopoulos A, Gyftopoulos K, Giannitsas K, Fisfis J, Perimenis P, Barbalias G . Combination treatment with an alpha-blocker plus an anticholinergic for bladder outlet obstruction: a prospective, randomised, controlled study. J Urol 2003; 169: 2253–2256.
Park YI, Linsenmeyer TA . A method to minimize indwelling catheter calcification and bladder stones in individuals with spinal cord injury. J Spinal Cord Med 2001; 24: 105–108.
Ord J, Lunn D, Reynard J . Bladder management and risk of bladder stone formation in spinal cord injured patients. J Urol 2003; 170: 1734–1737.
Vaidyanathan S, Singh G, Sett P, Soni BM . Bladder stones of unusual shape in a male with paraplegia due to spinal cord injury who has been performing self-catheterisation. Spinal Cord 1999; 37: 375–376.
Solomon MH, Koff SA, Diokno AC . Bladder calculi complicating intermittent catheterization. J Urol 1980; 124: 140–141.
Amendola MA, Sonda LP, Diokno AC, Vidyasagar M . Bladder calculi complicating intermittent clean catheterization. AJR Am J Roentgenol 1983; 141: 751–753.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vaidyanathan, S., Soni, B., Oo, T. et al. Delayed complications of discontinuation of intrathecal baclofen therapy: resurgence of dyssynergic voiding, which triggered off autonomic dysreflexia and hydronephrosis. Spinal Cord 42, 598–602 (2004). https://doi.org/10.1038/sj.sc.3101631
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101631
Keywords
This article is cited by
-
Treatment of detrusor sphincter dyssynergia with baclofen and doxazosin
International Urology and Nephrology (2007)