Abstract
Study design:
An in vivo study in Wistar albino rats with injured spinal cord.
Setting
Department of Neurosurgery, Biochemistry and Pathology, Gazi University, Ankara, Turkey.
Objectives:
The aim of this study was to investigate and compare the effects of FK506 an immunosupressive agent with methylprednisolone (MP) on lipid peroxidation (LP) in injured spinal cord tissue.
Method:
A total of 28 adult healthy Wistar albino rats were subjected to traumatic spinal cord injuries (SCI) by using an aneurysmal clip compression technique, and they were divided into four groups. The G1 group (n=8) received FK506 (1 mg/kg); the G2 group (n=8) received FK506 (1 mg/kg) and MP (30 mg/kg); the G3 group (n=6) received only MP (30 mg/kg); and the G4 group (n=6) received no medication. The injured spinal cord tissue was studied by means of lipid peroxides, malondialdehyde (MDA), with thiobarbituric acid reaction and additionally the FK506 (G1); the MP (G3) groups were studied for histopathologic alterations 72 h after SCI with eight separate animals.
Results:
Although LP values of G1, G2, G3 showed no statistical difference between intergroup analyses (P=0.547), a histopathological examination revealed that in the group that received MP, the oedema pattern was more significant than the group that received FK506. Another interesting finding was the presence of polymorphonuclear leucocytes in the MP group, whereas no infiltration was found in the FK506 group.
Conclusion:
Analysis of the results indicated that FK506 is a valuable pharmacological agent that could be used to decrease the LP and polymorphonuclear leucocyte infiltration and inflamatory reactions in the injured spinal cord tissue.
Similar content being viewed by others
Introduction
Immunosuppressive drugs are essential in prolonging allograft survival. FK506 is a macrolide lactane antibiotic that was introduced in 1989 by Starzl as an immunosuppressive agent.1 FK506 binds intracellular receptor FKB-12, immunophilin that is rotamase, and this complex interferes with intracellular calcium-dependent signal transduction pathways, processes that are central to T-cell activation.2,3,4 The FK506/FKB12 complex inhibits calcium- and calmodulin-dependent protein phosphatase, calcineurin, which that prevents the dephosphorylation of nuclear factor of activated T cell (NF-AT), leading to inactivation of IL-2 gene transcription and immunosuppression.5,6 In vitro, it has been shown that FK506 also inhibits lymphocyte migration, including T cells, in response to IL-2 or IL-8 chemotactic signaling.7
This study investigated the ability of immunosuppressant FK506 to reduce the free radical count in spinal cords after the experimental traumatic spinal cord injury (SCI) in rats.
Materials and methods
A total at 28 adult male Wistar albino rats weighing between 250 and 310 g were used in this experiment. The animal experimentation was conducted in conformity with the ‘Guide for the care and use of laboratory animals’ (National Institutes of Health publication No: 86–23). Anaesthesia was induced with (10 mg/kg) xylazine and (50 mg/kg) ketamine hydrochloride. C6-T2 laminectomy was performed. Dura mater was exposed and the extradural spinal cord at T1 was compressed for 1 min with an aneurysm clip (closing force 70 g), which caused complete paraplegia that remained unchanged during the course of the study. After the injury, the paraspinal musculature and subcutaneous tissues were closed with absorbable suture material. The paraplegic animals were then divided into four groups. In the first group (G1) (n=8), the SCI animals received a daily subcutaneous injection of FK506 treatment of 1 mg/kg in 3 days. In group 2 (G2) (n=8), FK506 was administered 1 mg/kg once per day for 3 days started after the intraperitoneal methylprednisolone administration following the SCI. In group 3 (G3) (n=6), each animal received two doses of methylprednisolone 30 mg/kg. Rats in the control group (G4) (n=6) received no medication after the SCI. The first dosage of FK506 and methylprednisolone was administered within 30 min of surgery; the final and the second dosage of MP was administered 24 h later via intraperitoneally. The animals were housed in a temperature-controlled room (26–28°C) for 3 days, one per cage. Bladders were manually expressed three times per day. All animals were killed by decapitation 72 h after spinal cord injury. Injured segment (1 cm) of spinal cord was dissected and stored at −20°C for assays at malondialdehyde (MDA). In order to evaluate the histopathological changes in the animals that received FK506 and MP, we studied another eight rats (n=4 each group) that were subjected to the same procedure in G1 and G3.
Sources of supplies and equipment
FK506 (Prograf, 5 mg/ml) was obtained from Fujisawa Ireland Co. Kerry (Ireland). Methylprednisolone sodium succinate (Prednol-L 20 mg) was obtained from Mustafa Nevzat Co. (Istanbul, Turkey). The aneurysm clip was purchased from Aesculap AG (FE 751 K with a closing force at 70 g, Tuttlingen, Germany).
Measurement of tissue MDA levels
Tissue homogenates were prepared in a ratio of 1 g of wet tissue to 9 ml of 1.15%. KCl by using a Teflon homogeniser.
Procedure: In all, 0.2 ml of 10% (w/v) tissue homogenate was added to 0.2 ml of 8.1% SDS, 1.5 ml of 20% acetic acid solution adjusted to pH 3.5 with NaOH, and 1.5 ml of 0.8% aqueous solution of TBA. The mixture was made up to 4.0 ml with distilled water, and then heated at 95°C for 60 min. After cooling with tap water, 1.0 ml of distilled water and 5.0 ml of the mixture of n-butanol and pyridine (15:1 v/v) were added and shaken vigorously. After centrifugation at 4000 rpm for 10 min, the organic layer was taken and its absorbency at 532 nm was measured. 1,1,1,3-Tetraethoxy propane was used as the standard. The results were expressed as nmol MDA/g wet tissue.8
Histopathology
For histopathologic examination, sections obtained from formalin-fixed, paraffin-embedded tissue samples were used. The samples were stained using haematoxylin and eosin to evaluate tissue changes after SCI.
Statistical analysis
Data were expressed as the mean±standard error of the mean (Table 1). Statistical differences between the four groups and triple comparison for G1–G2–G3 were compared using the Kruskal–Wallis variance analysis. A probability value of less than 0.05 was considered statistically significant. In the comparison of groups, two-by-two Mann–Whitney u-test was used (in case the P-value was <0.05).
Results
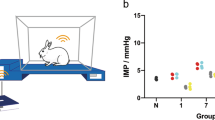
Figure 1 shows the effect of SCI with and without the drug administration on MDA levels in spinal cord homogenate, measured 72 h after the trauma. Although comparison between the four groups showed statistical difference (P=0.01), the intergroup comparison between G1–G2–G3 revealed no difference (P=0.547). For G1–G2, G1–G3, G2–G3, the MDA values were not different statistically (P=0.528, 0.30 and 0.560, respectively). For G1–G4, G2–G4 and G3–G4, the MDA values were significantly different (P=0.01, 0.07 and 0.06, respectively). FK506, FK506 with MP and MP administration (G1, G2, G3) attenuated the decrease in the MDA level noted in the trauma-only group (G4).
Histopathologic examinations of G1 and G3 were carried out. In G3, there were signs of tissue degeneration and necrosis that was evident in the posterior and central regions of the spinal cord, with severe oedema where the necrotic regions also included polymorphonuclear leucocytes (Figure 2). In G1, histopathological changes in the spinal cord were similar to those observed in G3, but the oedema pattern was relatively less and no signs of inflammatory cells in the necrotic regions were determined (Figure 3).
Discussion
The central nervous system possesses high levels of polyunsaturated lipids and metabolic rate, and, on the other hand, low antioxidant enzyme activity when compared to other tissues. This makes the free radical formation hazardous.9,10,11 In SCI, both primary and secondary injuries are involved in the physiopathology. Activation of endogenous substances prompted the secondary injury. There have been a number of studies performed in an attempt to identify the pathophysiological mechanisms occurring after traumatic SCI.12,13,14,15 Lipid peroxidation is one of the main pathological mechanisms involved in secondary damage after a SCI. The primary autodestructive event is started by the hydrolysis of fatty acids from membrane phospholipids, leading to cellular damage.16 Reduction of lipid peroxidation with methylprednisolone treatment in SCI seemed to be the main factor in the improvement of the outcome.17,18,19 Another key factor in the secondary injury mechanism was Ca+2 ion. Following the trauma or ischaemia, Ca+2 influx plays an important role in the pathogenesis of neural injury.20,21 In contused spinal cords, Happel et al22 showed that time promotes encouraged increases in calcium content in the total tissue. Banik et al23 reported that perfusion onto the spinal cord with high concentrate Ca+2-included solutions causes similar biochemical and histopathological changes, mimicking trauma.
There are different mechanisms discussed in the neuroprotective effect of FK 506. In T lymphocytes, FK506 binds immunophilin FKB12 that inhibits the calcineurin. This action involves the immunosuppresive effect of the drug.24,25 Calcineurin is reported to regulate calcium channel activity that is proposed for calcium in neurodegeneration.26,27 Ca+2 influx activates a Ca+2-sensitive protein phosphatase, calcineurin, which dephosphorylates the channel, thereby inactivating it.28 Another well-known effect of FK506 is reducing the superoxide radical formation in neutrophils dose dependently.29 The inhibition of dephosphorylation of nitric oxide synthase reduces the formation of nitric oxide (NO) and NO-dependent free radical formation that leads to cellular damage.30,31 Calcineurin also regulates nitric oxide synthase (NOS) activity in a Ca+2-dependent manner.32 Phosphorylated NOS is inactive and its dephosphorylation by calcineurin elicits the formation of nitric oxide, which can then react with superoxide radicals to form highly toxic peroxynitrite radicals.30,32 Toung et al33 reported that FK506 failed to reduce NO production in vivo during brain ischaemia, which indicates a neuroprotective mechanism of the drug, rather than reducing NO. However, Dowson et al34 suggested that FK506 shows its cerebroprotective actions by inhibiting NO production, indirectly preventing the calcineurin-mediated dephosphorylation of NOS.30 In the presented study, no statistical difference was observed in measured MDA levels between the glucocorticoid and glucocorticoid with FK506-combined and FK506-received groups. These results show that administration of FK506 is able to diminish the production of LP in injured spinal cords. This result might be postulated as FK506 could decrease the free radical formation following the traumatic SCI by preventing the calcineurin-mediated dephosphorylation of NOS. However, the calcineurin level in the spinal cord is low according to the data by the measurement of the enzyme-immunoassay method, whereas the putamen, caudate nucleus and hippocampus have high levels.34 In this study, measured LP levels between G1–G2–G3 indicated no statistical difference. It may be implicated that FK506 is effective as glucocorticoids in the inhibition of SCI, inducing LP to diminish neural tissue damage.
Bavetta et al35 examined the effects of FK506 and GPI 1046 on the responses to partial transection of ascending spinal dorsal column axons in rats. In their study, they also compared the effect of MP and concluded that the combination of FK506 and MP is more significantly effective than MP alone in protecting axons but not more effective than FK506 alone. FK506 is considered to improve neural damage by inhibition of neuronal calcineurin activity, and the inhibitory effects for calcineurin on inflammatory cells may contribute to improvement.36 Following the SCI, inflammatory reaction with polymorphonuclear leucocytes and other inflammatory cells causes cytokine-induced macrophage migration that increases vascular permeability, favouring oedema.37 In the presented study, a histopathological absence of polymorphonuclear leucocytes and relatively less oedema formation in G1 indicated the effectiveness of FK506 on the inflammatory cells, eosinophils, and neutrophils.38,39,40 As a conclusion, in SCI, FK506 could be used to inhibit the inflammatory reaction, decreasing the formation of free radicals and lipid peroxidation, which is valuable in neuroprotection and in maintaining the cord function.
References
Starzl TE, Todo S, Fung J, Demetris AJ, Venkataramman R, Jain A . FK506 for liver, kidney and pancreas transplantation. Lancet 1989; 2: 1000–10004.
Schreiber SL . Chemistry and biology of the immunophilins and their immunosuppressive ligands. Since 1991; 251: 283–287.
Siekierka JJ, Strauch MJ, Hung SH, Sigal NH . FK-506, a potent novel immunosuppressive agent, binds to a cytosolic protein which is distinct from the cyclosporin A-binding protein, cyclophilin. J Immunol 1989; 143: 1580–1583.
De Franco AL . Immunosuppressants at work. Nature 1991; 352: 754–755.
Sigal NH, Dumont FJ . Cyclosporin A, FK-506, and rapamycin: pharmacologic probes of lymphocyte signal transduction. Ann Rev Immunol 1992; 10: 519–560.
Flanagon WM, Corthesy B, Bram RJ, Crabtree GR . Nuclear association of a T-cell transcription factor blocked by FK-506 and cyclosporin A. Nature 1991; 352: 803–807.
Adams DH, Liu Q . FK506 inhibits human lymphocyte migration and production of lymphocyte chemotactic factors in liver allograft recipients. Hepatology 1996; 23: 1476–1483.
Ohkawa H, Ohishi N, Yagi K . Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 1979; 95: 351–358.
Aspberg A, Tottmar O . Oxidative stres decreases antioxidant enzyme activities in reaggregation cultures of brain cells. Free Radical Biol Med 1994; 17: 511–516.
Halliwell B, Gutteridge JMC . Oxygen radicals and the nervous system. Trends Neurosci 1985; 8: 22–26.
Bulkley GB . The role of oxygen free radicals in human disease processes. Surgery 1983; 94: 407–411.
Blight A . Spinal cord injury models; neurophysiology. J Neurotrauma 1992; 9: 147–150.
Hamada Y et al. Roles of nitric oxide in compression injury of rat spinal cord. Free Radic Biol Med 1996; 20: 1–9.
Kaptanoğlu E, Caner HH, Sürücü HS, Akbiyik F . Effect of mexiletine on lipid peroxidation and early ultrastructural findings in experimental spinal cord injury. J Neurosurg 1999; 91(2 Suppl): 200–204.
Tator CH, Fehlings MG . Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991; 75: 15–26.
Kaptanoğlu E, Tuncel M, Palaoğlu S, Konan A, Demirpençe E, Kilinç K . Comparison of the effects of melatonin and methylprednisolone in experimental spinal cord injury. J Neurosurg 2000; 93(1 Suppl): 77–84.
Anderson DK et al. Lipid hydrolysis and peroxidation in injured spinal cord; partial protection with methylprednisolone or vitamin E and selenium. Cent Nerv Syst Trauma 1985; 2: 257–267.
Braughler JM, Hall ED . Correlation of methylprednisolone levels in cat spinal cord with its effect on (Na++K+)-ATPase, lipid proxidation, and alpha motor neuron function. J Neurosurg 1982; 56: 838–844.
Braughler JM, Hall ED . Current application of ‘high dose’ steroid therapy for CNS injury. A pharmacological respective. J Neurosurg 1985; 62: 806–810.
Hall ED, Wolf DL . A pharmacological analysis of the pathophysiologic mechanisms of posttraumatic spinal cord ischemia. J Neurosurg 1986; 64: 951–961.
Young W, Koreh I . Potassium and calcium changes in injured spinal cords. Brain Res 1986; 365: 42–53.
Happel RD, Smith KP, Banik NL, Powers JM, Hogan EL, Balentine JD . Ca+2 accumulation in experimental spinal cord trauma. Brain Res 1981; 211: 476–479.
Banik NL, Hogan EL, Whetstine LJ, Balentine JD . Changes in myelin and axonal proteins in CaCl2-induced myelopathy in rat spinal cord. Cent Nerv Syst Trauma 1984; 1: 131–137.
Clipstone NA, Crabtree GR . Identification of calcineurin as a key signalling enzyme in T-lymphocyte activation. Nature 1992; 357: 695–697.
Liu J et al. Inhibition of T cell signaling by immunophilin–ligand complexes correlates with loss of calcineurin phosphotase activity. Biochemistry 1992; 31: 3896–3901.
Amstrong DL . channel regulation by calcineurin, a Ca+2-activated phosphotase in mammalian brain. Trends Neurosci 1989; 12: 117–122.
Choi DW . Calcium-mediated neurotoxicity; relationship to specific channel types and role in ischemic damage. Trends Neurosci 1988; 11: 465–469.
Kandel ER, Schwartz JH, Jessell TM . Principles of neural science. In: Koster J (ed). Voltage-Gated Ion Channels and the Generation of the Action Potential of the Action Potential, 3rd edn. Elsevier: New York, 1991, pp 104–118.
Nishinaka YS, Sugiyama S, Yokota M, Saito H, Ozawa T . Protective effect of FK506 on ischemia/reperfusion induced myocardial damage in canine heart. J Cardiovasc Pharmacol 1993; 21: 448–454.
Dawson TM, Steiner JP, Dawson VL, Dinerman JL, Uhl GR, Snyder SH . Immunosuppressant FK506 enhances phosphorylation of nitric oxide synthase and protects against glutamate neurotoxicity. Proc Natl Acad Sci USA 1993; 90: 9808–9812.
Lipton SA et al. A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature 1993; 364: 626–632.
Morioka M, Hamada JI, Ushio Y, Miyamoto E . Potential role of calcineurin for brain ischemia and traumatic injury. Prog Neurobiol 1999; 58: 1–30.
Toung TJ, Bhardwaj A, Dawson VL, Dawson TM, Traystman RJ, Hum PD . Neuroprotective FK506 does not alter in vivo nitric oxide production during ischemia and early reperfusion in rats. Stroke 1999; 30: 1279–1285.
Goto S, Matsukado Y, Mihara Y, Inoue N, Miyamoto E . The distribution of calcineurin in rat brain by light and electron microscopic immuno-histochemistry and enzyme-immunoassay. Brain Res 1986; 397: 161–172.
Bavetta S, Hamlyn PJ, Burnstock G, Lieberman AR, Anderson PN . The effects of FK506 on dorsal column axons following spinal cord injury in adult rats: neuroprotection and local regeneration. Exp Neurol 1999; 158: 382–393.
Morioka M, Hamada J, Ushio Y, Miyamoto E . Potential role of calcineurin for brain ischemia and traumatic injury. Prog Neurobiol 1999; 58: 1–30.
Vaquero J, Zurita M, de Oya S, Coca S . Vascular endothelial growth/permeability factor in spinal cord injury. J Neurosurg 1999; 90(Suppl 4): 220–223.
Hom JT, Estridge T . FK506 and rapamycin modulate the functional activities of human peripheral blood eosinophils. Clin Immunol Immunopathol 1993; 68: 293–300.
Burnett D et al. Inhibition by FK506 of formyl peptide-induced neutrophil activation and associated protein synthesis. Biochem Pharmacol 1994; 48: 1081–1088.
Taoka Y et al. Activated protein C reduces the severity of compression-induced spinal cord injury in rats by inhibiting activation of leukocytes. J Neurosci 1998; 18: 1393–1398.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kaymaz, M., Emmez, H., Bukan, N. et al. Effectiveness of FK506 on lipid peroxidation in the spinal cord following experimental traumatic injury. Spinal Cord 43, 22–26 (2005). https://doi.org/10.1038/sj.sc.3101621
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101621