Abstract
Study design: Comparison of different kinematic and loading conditions on muscle activation in clinically complete spinal cord-injured subjects stepping unilaterally with manual assistance.
Objective: To determine if rhythmic lower limb loading or movement could produce rhythmic muscle activation in the nonstepping limb of subjects with clinically complete spinal cord injury (SCI).
Setting: Human Locomotion Research Center, Department of Neurology, University of California, Los Angeles, USA.
Methods: We recorded electromyography, joint kinematics, and vertical ground reaction forces as four subjects with clinically complete SCI stepped with manual assistance and partial bodyweight support. For all trials, one limb continuously stepped while the other limb underwent different conditions, including rhythmic lower limb loading in an extended position without limb movement, rhythmic lower limb movement similar to stepping without limb loading, and no lower limb loading or movement with the leg in an extended or flexed position.
Results: Three subjects displayed rhythmic muscle activity in the nonstepping limb for trials with rhythmic limb loading, but no limb movement. One subject displayed rhythmic muscle activity in the nonstepping limb for trials without ipsilateral limb loading or movement. The rhythmic muscle activity in the nonstepping limb was similar to the rhythmic muscle activity during bilateral stepping.
Conclusions: The human spinal cord can use sensory information about ipsilateral limb loading to increase muscle activation even when there is no limb movement. The results also indicate that movement and loading in one limb can produce rhythmic muscle activity in the other limb even when it is stationary and unloaded. These findings emphasize the importance of optimizing load-related and contralateral sensory input during gait rehabilitation after SCI.
Similar content being viewed by others
Introduction
When humans with clinically complete spinal cord injuries (SCI) step bilaterally with partial bodyweight support and manual assistance, they exhibit locomotor-like muscle activity patterns in their lower limbs.1,2 Presumably, proprioceptive feedback related to the kinematics and kinetics of stepping activates and coordinates locomotor networks in the spinal cord to produce the rhythmic muscle activation patterns.3 Previous studies have found that the amplitude of muscle activity in clinically complete SCI subjects is directly related to the magnitude of lower limb load during bilateral stepping.4,5 Steps with greater limb loading during stance have increased electromyography (EMG) amplitudes compared to steps with less limb loading, but similar kinematics. Although limb loading during stepping appears to be an important proprioceptive signal affecting muscle activation patterns in humans with clinically complete SCI, the relative importance of limb loading versus limb kinematics is not known. Evidence from a range of animal species indicates that the central nervous system uses multiple sensory signals, including limb loading and limb kinematics, to generate and modify locomotor muscle activity patterns.6 It seems reasonable to suppose that neuronal networks in the human spinal cord also use multiple sensory signals to generate and modify rhythmic muscle activity patterns,7 but it has been difficult to implicate specific signals because of the multitude of sensory information involved in normal human locomotion.
We studied humans with clinically complete SCI during unilateral stepping to examine the effects of different sensory signals on muscle activation. Unilateral stepping was an ideal paradigm for this study because it allowed us to manipulate loading and movement independently in one limb, while the other limb continued to step with normal kinematics and loading. Past studies on spinalized cats and healthy humans have demonstrated that unilateral stepping induces the activation of locomotor central pattern generators8,9 and reflex modulation similar to normal locomotion,10,11 respectively. By studying spinal cord-injured humans during unilateral stepping and manipulating the loading pattern and position of the leg, we were able to compare the independent effects of rhythmic lower limb loading versus rhythmic lower limb movement on the nonstepping limb. Our goal was to determine if either condition was sufficient to produce rhythmic muscle activity in the nonstepping limb. For all conditions, the contralateral limb continued stepping with manual assistance so that it experienced both rhythmic loading and movement.
Materials and methods
Subjects
Four individuals with SCI volunteered for this study (Table 1). All subjects completed sensory-evoked potentials examinations to test for conductivity between the lower limbs and the brain. The results indicated no detectable potential in the cortex from either limb for all four subjects. In addition, the clinical staff tested subjects’ sensory and motor function according to the American Spinal Injury Association (ASIA) impairment scale12 to certify that subjects had clinically complete SCI (ie ASIA-A classification). No current test for completeness of SCI in humans is absolutely definitive. As a result, we define our subjects as clinically complete when the subjects are classified as ASIA-A with clinical exam and sensory-evoked potentials are absent at the cortex bilaterally. The University of California Los Angeles Human Subjects Protection Committee approved all the experiments and each subject signed an informed consent form. The experimental procedures conformed to the policies and principles contained in the Declaration of Helsinki. Subject numbering in Table 1 conforms to identification numbers of SCI subjects in the UCLA Human Locomotion Research Center database so that identification is consistent across publications.
Subjects underwent bilateral locomotor training with manual assistance and partial bodyweight support13 prior to data collection (Table 1). The number of training sessions for Subjects A15, A16, and A6 were designed to enable subjects to complete the data collection session without distress, not to produce substantial changes from long-term training. Subject A14 underwent a considerably longer period of locomotor training compared to other subjects because Subject A14 was involved in a long-term training study in addition to this study and may have had adaptive changes as a result of the relatively high number of consecutive sessions. The data collection session for each subject typically lasted 4–5 h and included approximately 15–30 min of actual stepping. The same trainers provided manual assistance for all subjects throughout data collection.
Procedure
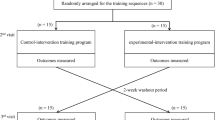
Subjects performed six different stepping conditions in a quasirandomized order (Figure 1). The order was quasirandomized because all unilateral stepping bouts were completed in between initial and final bilateral stepping bouts. This was necessary due to the technical limitations of shifting the treadmill laterally for the unilateral stepping bouts. For all conditions, subjects stepped on a treadmill with partial bodyweight support and manual assistance. Subjects completed a minimum of two stepping bouts for each of the six conditions with unilateral stepping bouts randomized in order. We collected data bilaterally from eight consecutive steps for each stepping bout. In between stepping bouts, the treadmill was turned off and the subjects stood in place with partial weight bearing or rested in a chair. Additional breaks were provided for the subjects when we shifted the treadmill during the experiment.
Schematic of the six stepping conditions. Subjects wore harnesses connected to an overhead support that provided partial bodyweight support and limited the downward movement of the subject's torso. Trainers provided manual assistance to both limbs as necessary for all conditions. The first stepping condition was the prebilateral condition (a) where subjects stepped bilaterally. The unistanding condition (b) had one limb stepping, while the other limb was standing on a stationary platform. The uniextended condition (c) had one limb stepping, while the other limb was bearing no weight but was supported in a normal standing position by a string. The harness prevented the subject from falling when both limbs were not in contact with the ground by supporting the subject's entire body weight. The uniflexed condition (d) had one limb stepping, while the other limb was supported in a flexed position by a string. The uniairstepping condition (e) had one limb stepping, while the other limb was airstepping (ie bearing no weight, but moving through motions similar to stepping). The last stepping condition was the postbilateral stepping condition (f). Each subject repeated each condition a minimum of two times with a randomized order for unilateral stepping conditions
Three trainers manually facilitated subjects’ lower limbs through the step cycle, providing assistance as needed.13 A harness attached to a stiff suspension cable supported the subjects. The cable provided a vertical constraint on the movement of the torso and reduced the vertical ground reaction force by supporting a portion of the subject's body weight. We monitored the support force of the cable with a strain gauge load cell attached to the cable. During the bilateral stepping condition (Figure 1a), two trainers held each stepping limb distal to the patella to facilitate knee flexion during the swing phase, and knee and hip extension during the stance phase. Trainers used their other hand to hold each stepping limb proximal to the ankle during the swing phase to assist with foot lift off and placement. A third trainer provided stabilization at the hips to prevent excessive hip movement and simulate normal stepping kinematics more closely. During the unistanding condition (Figure 1b), one limb was stepping and the other limb was in a normal standing position on a wooden block. The treadmill had been moved laterally to provide room for the block, allowing the nonstepping limb to bear weight as in standing. The trainer at the stepping limb moved it through the normal stepping motions as during bilateral stepping. The trainer at the nonstepping limb had one hand on the lateral and medial aspects of the heel (being careful not to touch the Achilles tendon) and the other hand on the thigh. The goal of the trainer was to minimize all movement of the limb and attempt to keep the knee and ankle from flexing or extending. The trainer stabilizing the hips attempted to provide rhythmic lateral tilting of the torso and pelvis so that the load on the standing limb would decrease when that limb would typically be in swing. For some subjects, the tilting was enough to lift the sole of the standing foot 1–2 cm off the block. For other subjects, the sole remained on the block because the tilting was not enough to bring the foot off the block. During the uniextended condition (Figure 1c), one limb was stepping and the other limb was in a normal standing position, but not bearing weight. This was similar to the unistanding condition, except that the wooden block had been removed. A string was connected from the bottom of the harness to the shoe of the extended limb to maintain the ankle angle in normal standing position. The stepping limb was placed on the outer part of the treadmill belt. During the uniflexed condition (Figure 1d), procedures were identical to the uniextended condition, except that the string held the nonstepping limb with a knee angle of approximately 90°. The trainer had one hand on the front of the thigh and one hand on the anterior side of the ankle, attempting to minimize ankle displacement. During the uniairstepping condition (Figure 1e), the trainer on the nonstepping limb moved the limb through a normal stepping motion without making foot–ground contact. The treadmill was still shifted laterally, preventing any foot–ground contact.
Each subject stepped at a constant treadmill speed (range 0.9–1.25 m/s) and level of harness support (range 42–75% body weight). We aimed at providing the least bodyweight support and fastest treadmill speed at which each subject was comfortable stepping for long bouts. Three subjects completed testing on both limbs, while Subject A14 only completed testing on one limb at the subject's request. We also did not obtain data on Subject A14 for the uniairstepping condition.
Data acquisition
We measured EMG, joint kinematics, and vertical ground reaction forces bilaterally for all stepping conditions. We recorded EMG using bipolar silver–silver chloride surface electrodes connected to hard-wired signal conditioning amplifiers (Konigsberg Instruments, Pasadena, CA, USA) that had a bandwidth of 10–1000 Hz. We placed EMG electrodes on the soleus (distal to the gastrocnemius muscle belly and lateral to the Achilles tendon), medial gastrocnemius (below the popliteal crease on medial aspect of calf), and tibialis anterior (below the tibial tuberosity and lateral to the tibial crest). Visual inspection of EMG signals during manually initiated rapid plantarflexion and dorsiflexion movements verified that crosstalk was negligible.14 We placed analog footswitches on the bottom of each shoe at the heel, first metatarsal, fifth metatarsal, and toe to detect foot–ground contact. A personal computer sampled EMG and foot switch signals at 1000 Hz via an analog-to-digital converter and a customized software program (LabVIEW, National Instruments Corporation, Austin, TX, USA). We recorded limb kinematics at 30 Hz with electromagnetic sensors (6D-Research System, Skill Technologies Inc., Phoenix, AZ, USA) placed on the foot, shank, thigh, and pelvis. We defined the ankle angle as the angle formed by the tibia, ankle joint center of rotation, and metatarsophalangeal joint. The ankle angle during standing position was approximately 120° for all subjects. We recorded vertical ground reaction forces (VGRF) at 50 Hz with in-sole pressure transducers (Pedar, Novel Electronics Inc., St Paul, MN, USA) placed inside the shoes. Nondisabled subjects of comparable weight and shoe size to SCI subjects walked over a force platform (Kistler, Amherst, NY, USA) wearing the testing shoes to verify the calibration of in-sole pressure sensors before each data collection. We synchronized data acquisition systems by recording analog timing signals from the in-sole pressure transducer system and the electromagnetic sensor system on the personal computer collecting EMG signals. We videotaped all data collection sessions and synchronized the video recording with data acquisition by means of a Society for Motion Picture and Television Engineers (SMPTE) time code. The time-stamped videotape allowed us to verify the synchronization accuracy of data from the footswitches, in-sole pressure transducers, electromagnetic sensors, and EMG for each stepping condition.
Data analysis
We processed data using customized software programs (LabVIEW, National Instruments). The final analysis included 848 steps, an average of 20.6 steps per condition (n=6 for Subjects A6, A15, and A16; n=5 for Subject A14) per limb (n=7; two limbs for Subjects A6, A15, and A16; one limb for Subject A14). We filtered EMG signals using a fourth-order Butterworth band-pass filter (40–500 Hz) before full-wave rectification. We quantified EMG amplitude by taking the mean amplitude of the rectified EMG burst from each stride cycle. A single individual marked burst onset and burst offset for all EMG data using a customized software program to view data. When no burst was visible, the mean amplitude was taken for the entire stride. Manual burst marking has been shown to be reliable and often times superior to burst marking by computer algorithms.15 Post hoc analyses revealed high correlations between EMG burst mean amplitudes and EMG stride cycle mean amplitudes (P<0.001, R>0.98) for all step cycles with clear EMG bursts. This strongly suggests that the manual determination of burst timing did not skew results. From the in-sole pressure transducer data, we calculated the mean vertical ground reaction force (VGRF) during the stance phase of each step for the stepping limb. We also used the in-sole pressure transducer data to calculate the time between successive heel contacts of the stepping limb (ie stride duration). We filtered joint kinematic data with a fourth-order Butterworth low-pass filter with a cutoff frequency of 6 Hz. After identifying the beginning and end of each stride, we calculated the ankle displacement of the stepping limb by subtracting the minimum joint angle from the maximum joint angle. Lastly, we averaged EMG, kinematic, and kinetic data for eight consecutive steps in the middle of each stepping bout (randomly chosen) for statistical analysis.
Statistics
We performed a repeated measures ANOVA and Tukey's honestly significant difference (HSD) post hoc tests on stride duration, mean vertical ground reaction force, and ankle displacement data to test for statistical differences between conditions across the seven limbs (significance set at P<0.05). In cases where the nonstepping limb displayed rhythmic EMG bursts, we used ANOVAs on EMG amplitudes from different stepping conditions for that subject to determine if the conditions were statistically different (significance set at P<0.05). We used JMP IN software (SAS Institute, Inc.) for all statistical analyses.
Results
Kinematic and kinetic parameters
Trainers were able to produce consistent lower limb joint movements and vertical ground reaction forces for the different conditions. The mean stride duration was approximately 1.2 s for all conditions (repeated measures ANOVA, P=0.0561). The mean bodyweight load of the stepping limb and ankle displacement during stance was similar for all conditions (means: 39% body weight and 41°), except unistanding (repeated measures ANOVA, P=0.0488 and 0.0492, respectively). Limb loading and ankle displacement for the stepping limb were slightly lower during the unistanding condition (31% body weight and 35°) because the nonstepping limb was bearing a portion of the body weight during the stepping limb's stance phase (Tukey's HSD, P<0.05).
EMG activity during bilateral stepping
Subjects exhibited different EMG patterns in the soleus, medial gastrocnemius, and tibialis anterior during bilateral stepping (Figure 2). Two subjects demonstrated rhythmic EMG activity in both limbs during bilateral stepping (Subjects A14 and A15). Subject A14 had rhythmic soleus and medial gastrocnemius EMG activity in both legs, and tibialis anterior EMG activity in the left leg. Soleus and medial gastrocnemius activity occurred during stance and tibialis anterior activity occurred during late stance and early swing. Subject A15 had rhythmic EMG activity in all three muscles during stance in both legs. Subject A16 had rhythmic EMG activity only in the left soleus and tibialis anterior during bilateral stepping. Subject A6 did not display consistent rhythmic EMG activity in any muscles during bilateral stepping.
Example prebilateral stepping data. EMG data are from soleus (SOL), medial gastrocnemius (MG), and tibialis anterior (TA) muscles for the left and right limbs. Kinematic data are joint angles for the hip, knee, and ankle. Kinetic data are vertical ground reaction forces (VGRF). (a) Subject A14 had rhythmic EMG bursts synchronized to the step cycle for five of the six muscles. (b) Subject A15 had rhythmic EMG bursts synchronized to the step cycle for all six muscles
EMG activity in the nonstepping limb during unilateral stepping
Unistanding
Three subjects exhibited rhythmic EMG bursts in their nonstepping limb during the unistanding condition (Subjects A14, A15, and A16). Subject A14 displayed rhythmic soleus EMG bursts in the nonstepping limb during the unistanding condition, but did not display medial gastrocnemius or tibialis anterior EMG bursts (Figure 3a). Ankle displacement was less than 3° for Subject A14 during unistanding. Subject A15 displayed rhythmic EMG activity in all three muscles in the nonstepping limb during unistanding (Figure 3b). Although trainers attempted to minimize joint movement in the nonstepping limb of Subject A15, the right ankle range of motion during each stride was approximately 10–14°. Subject A16 had rhythmic EMG bursts in the medial gastrocnemius muscle during the unistanding condition (Figure 3c). Unlike Subjects A14 and A15, the majority of the medial gastrocnemius EMG bursts occurred when the limb was not being loaded in Subject A16. The right ankle displacement during unistanding for Subject A16 was 6–12° per stride.
Unistanding data for three subjects with rhythmic EMG in the nonstepping limb. (a) Subject A14 had soleus EMG activity in the nonstepping limb (right limb) synchronized to ipsilateral limb loading. The right ankle and right knee range of motion were less than 3° per stride. Right hip movement was 10° per stride due to the pelvis tilting as the left limb stepped. (b) Subject A15 had soleus, medial gastrocnemius, and tibialis anterior EMG bursts in the nonstepping limb (right limb) synchronized with ipsilateral limb loading. The right knee range of motion was less than 5°. (c) Subject A16 had rhythmic medial gastrocnemius EMG bursts in the nonstepping limb (right limb) synchronized with loading of the stepping limb (left limb)
Uniextended and Uniflexed
Only Subject A16 exhibited rhythmic EMG bursts in the nonstepping limb during the uniextended or uniflexed conditions with no limb loading (Figure 4). Both the medial gastrocnemius and the tibialis anterior had alternating bursts. The tibialis anterior EMG amplitude in the nonstepping limb was higher during the uniextended condition than during the other unilateral conditions (Tukey's HSD, P<0.05). The ankle displacement for Subject A16 was 7–10° for the uniextended condition and 2–4° for the uniflexed condition.
Uniextended data for subject with rhythmic EMG in the nonstepping limb. The medial gastrocnemius in the nonstepping limb (right limb) had rhythmic EMG bursts synchronized with contralateral limb loading. The right tibialis anterior also had rhythmic EMG bursts in antiphase with the left tibialis anterior EMG bursts. The right ankle range of motion had a frequency that was twice the stride frequency and twice the EMG burst frequency
Uniairstepping
No subjects demonstrated clear rhythmic EMG bursts in their nonstepping limb during the uniairstepping condition. Subject A15 had some faint EMG bursts, but the amplitude of muscle activity was very low and it was difficult to identify a clear rhythmic pattern. The range of ankle joint motion in the nonstepping limb of Subject A15 was similar for the uniairstepping (8–12°) and unistanding conditions (10–14°). All three muscles in Subject A15 had significantly higher EMG amplitudes for the unistanding condition compared to the uniairstepping condition (Tukey's HSD, P<0.05). Subject A16 had ankle displacements of 12–19° during airstepping, which were greater than ankle displacements during unistanding (6–12°) and uniextended conditions (7–10°).
Discussion
Our results demonstrate that in humans with clinically complete SCI: (1) ipsilateral limb loading without limb movement can result in rhythmic EMG activity when the contralateral limb is stepping, and (2) rhythmic EMG bursts can occur in a stationary unloaded limb if the contralateral limb is stepping.
EMG bursts related to limb loading
EMG activity was well synchronized with limb loading in both limbs for Subjects A14 and A15 (Figure 3). Both subjects demonstrated a small amount of ankle joint movement during the unistanding condition, but similar or greater ankle joint movement during other unilateral conditions was not sufficient to cause rhythmic EMG bursting. Indeed, the uniairstepping condition had the greatest amount of limb movement, but produced the lowest amount of rhythmic muscle activation. This suggests that the increases in EMG amplitude during limb loading were not caused by stretch reflex activation. Previous studies have found that the EMG amplitude increases in proportion to lower limb loading in nondisabled and spinal cord-injured humans,4,16,17,18 but those studies have examined normal bilateral stepping where the limb undergoes considerable flexion and extension with each step.
The most likely neural mechanisms for increased EMG amplitude during limb loading without limb movement are sensory feedback from cutaneous receptors on the soles of the feet and sensory input from Golgi tendon organs in lower limb extensor and plantarflexor muscles. Afferents from both sources could act through reflex pathways directly onto motor neurons or onto locomotor neural networks in the spinal cord9,19,20,21,22,23,24,25,26,27 (for review, see Duysens et al6). There is no way to tell from the current data as to which afferents or which pathways were responsible. Future studies on humans with SCI including direct electrical stimulation of afferents could provide a greater insight.21,28,29,30
Our finding that EMG amplitude increased with limb loading, but not with limb movement, is in direct contrast to another recent study on humans with clinically complete SCI.31 Dietz et al31 used a robotic orthosis (ie Lokomat) to move the lower limbs of spinal cord injury subjects through a stepping motion on a treadmill. They also studied a unilateral stepping condition with rhythmic limb loading on the stationary nonstepping limb (ie similar to our unistanding condition). Dietz et al31 found no rhythmic EMG bursts in the nonstepping limbs for their subjects with clinically complete SCIs. Two significant differences between the studies were the speed of stepping and the amount of limb loading. Dietz et al's subjects stepped at a fairly slow speed (0.5 m/s), while our subjects stepped at speeds closer to normal walking speeds for healthy subjects (0.9–1.25 m/s). Similarly, Dietz et al's subjects supported ∼30% of body weight on their nonstepping limb, while our subjects supported up to ∼60% of body weight on their nonstepping limb. Faster stepping speeds and greater limb loads enhance sensory feedback to the spinal cord and increase muscle activation amplitudes in humans with clinically complete SCI.4,32,33 As a result, it seems likely that the slower speeds and decreased limb loading used by Dietz et al may not have provided strong enough sensory stimuli to activate lower limb motor neurons. Another factor that could have played a role in differences between the studies is the amount of previous locomotor training. The duration and intensity of locomotor training has a major effect on the strength of spinal circuits.2,34,35,36,37,38,39,40 Our two subjects, who showed load-dependent increases in EMG amplitude (Subjects A14 and A15), had the greatest amount of locomotor training prior to testing in our study. It is not clear how much training Dietz et al's31 subjects underwent. Additional training studies that examine subjects before and after long duration locomotor training would help to determine if the amount of training is a major factor in load-dependent muscle activation.
EMG bursts induced by contralateral limb stepping
Rhythmic EMG bursts in Subject A16's nonstepping limb appeared to be caused by the contralateral limb stepping and not directly by ipsilateral limb loading. During the unistanding condition, peak medial gastrocnemius EMG in the nonstepping limb occurred when the limb was not being loaded. More importantly, rhythmic EMG bursts occurred in the medial gastrocnemius and tibialis anterior of Subject A16's nonstepping limb during the uniextended and uniflexed conditions. Although the limb joints in the nonstepping limb underwent a small amount of rhythmic movement in these conditions, there was a greater joint displacement without rhythmic EMG bursts during the uniairstepping condition. This suggests that ipsilateral muscle stretch was also not the direct cause of the rhythmic EMG bursts.
The most likely neural mechanism for the rhythmic EMG bursts in Subject A16's nonstepping limb is contralateral excitation of spinal locomotor circuits. Afferent feedback from the stepping limb could have stimulated locomotor circuits in the spinal cord, rhythmically activating muscles in the nonstepping limb via excitatory pathways. It has long been realized that cats and other nonhuman vertebrates possess spinal locomotor circuits with pathways coordinating left and right limb muscles.41,42,43,44,45 When decerebrate cats step unilaterally with one hindlimb stationary and the other hindlimb on a treadmill belt, they display rhythmic EMG bursts in the nonstepping limb8,9 similar to our results. Thus, the left–right spinal locomotor pathways are robust enough in cats that sensory information from the contralateral stepping limb can generate muscle activation in the nonstepping limb. Studies that have examined nondisabled humans stepping unilaterally found that rhythmic loading on the nonstepping limb can result in flexor EMG bursts and reflex modulation comparable to normal walking,10,31 although extensor EMG amplitudes are greatly reduced compared to normal walking.31 In addition, muscle activation patterns from healthy human subjects during cycling indicate that neuronal interlimb coupling affects motor patterns during cycling.46,47 Our finding of contralaterally induced muscle activation in a human with clinically complete SCI is the first evidence that left–right spinal locomotor pathways are capable of producing contralateral rhythmic muscle activation in humans.
It is important to note that the recent study by Dietz et al31 found no evidence of rhythmic EMG in the nonstepping limb of subjects with clinically complete SCI. Thus, our second main finding also contrasts from their study. The differences in the stepping speed and lower limb loading between the two studies could be the explanation for the contrasting results, as discussed previously above. Duysens and Pearson9 observed that when decerebrate cats stepped unilaterally with their hindlimbs, ‘vigorous walking’ produced more robust EMG bursts in the nonstepping limb and it was more difficult to inhibit the EMG bursts with manipulations of afferent feedback compared to less vigorous walking.9 This suggests that the closer stepping kinematics and kinetics in spinal subjects are to normal walking, the stronger the influence of contralateral locomotor neural pathways on muscle activation.
Implications for neurorehabilitation after SCI
Task-specific sensorimotor stimulation is the key to the effectiveness of locomotor training. Numerous studies have shown that locomotor training is a viable therapy for re-training SCI humans to walk.48,49,50,51,52 In designing a training regimen for each patient, therapists can modify a number of parameters to influence muscle activation patterns. Past studies have shown that the EMG amplitude and timing in SCI subjects respond to changes in limb loading,4,5 treadmill speed,32 and treadmill grade.53 These parameters can influence muscle activity patterns through multiple sensory pathways such as cutaneous receptors, muscle spindles, and Golgi tendon organs. Results from the present study add further evidence for ipsilateral limb loading, while also indicating that contralateral limb mechanics can be an important sensory cue in humans with SCIs. Ideally, therapists should aim for providing sensory information that is as close as possible to normal locomotion to maximize neuromuscular recruitment in patients. It may be helpful for therapists to use lower limb electromyography as a tool for identifying sensory inputs that are most helpful for a given patient. Where some spinal cord-injured individuals might respond to increased ipsilateral limb loading, other individuals might demonstrate a stronger muscle activation response to faster treadmill stepping. Therapists who are aware of the sensory signals affecting locomotor muscle activation patterns and provide sensory information that is as close as possible to normal walking will have the best chance of optimizing locomotor training for their patients.
References
Dobkin BH et al. Modulation of locomotor-like EMG activity in subjects with complete and incomplete spinal cord injury. J Neurol Rehabil 1995; 9: 183–190.
Dietz V et al. Locomotor capacity of spinal cord in paraplegic patients. Ann Neurol 1995; 37: 574–582.
Maegele M et al. Recruitment of spinal motor pools during voluntary movements versus stepping after human spinal cord injury. J Neurotrauma 2002; 19: 1217–1229.
Harkema SJ et al. Human lumbosacral spinal cord interprets loading during stepping. J Neurophysiol 1997; 77: 797–811.
Kojima N, Nakazawa K, Yano H . Effects of limb loading on the lower-limb electromyographic activity during orthotic locomotion in a paraplegic patient. Neurosci Lett 1999; 274: 211–213.
Duysens J, Clarac F, Cruse H . Load-regulating mecha-nisms in gait and posture: comparative aspects. Physiol Rev 2000; 80: 83–133.
Duysens J . Human gait as a step in evolution. Brain 2002; 125: 2589–2590.
Duysens J . Reflex control of locomotion as revealed by stimulation of cutaneous afferents in spontaneously walking premammillary cats. J Neurophysiol 1977; 40: 737–751.
Duysens J, Pearson KG . Inhibition of flexor burst generation by loading ankle extensor muscles in walking cats. Brain Res 1980; 187: 321–332.
Faist M et al. Modulation of the biceps femoris tendon jerk reflex during human locomotion. Exp Brain Res 1999; 125: 265–270.
Van de Crommert HW et al. Biceps femoris tendon jerk reflexes are enhanced at the end of the swing phase in humans. Brain Res 1996; 734: 341–344.
Maynard FM et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Behrman AL, Harkema SJ . Locomotor training after human spinal cord injury: a series of case studies. Phys Ther 2000; 80: 688–700.
Winter DA, Fuglevand AJ, Archer SE . Crosstalk in surface electromyography: theoretical and practical estimates. J Electromyogr Kinesiol 1994; 4: 15–26.
Hodges PW, Bui BH . A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electroencephalogr Clin Neurophysiol 1996; 101: 511–519.
Stephens MJ, Yang JF . Loading during the stance phase of walking in humans increases the extensor EMG amplitude but does not change the duration of the step cycle. Exp Brain Res 1999; 124: 363–370.
Ferris DP et al. Soleus H-reflex gain in humans walking and running under simulated reduced gravity. J Physiol (Lond) 2001; 530: 167–180.
Finch L, Barbeau H, Arsenault B . Influence of body weight support on normal human gait: development of a gait retraining strategy. Phys Ther 1991; 71: 842–855.
Duysens J, Pearson KG . The role of cutaneous afferents from the distal hindlimb in the regulation of the step cycle of thalamic cats. Exp Brain Res 1976; 24: 245–255.
Duysens J, Stein RB . Reflexes induced by nerve stimulation in walking cats with implanted cuff electrodes. Exp Brain Res 1978; 32: 213–224.
Yang JF, Stein RB . Phase-dependent reflex reversal in human leg muscles during walking. J Neurophysiol 1990; 63: 1109–1117.
Pearson KG, Collins DF . Reversal of the influence of group lb afferents from plantaris on activity in medial gastrocnemius muscle during locomotor activity. J Neurophysiol 1993; 70: 1009–1017.
Gossard JP et al. Transmission in a locomotor-related group lb pathway from hindlimb extensor muscles in the cat. Exp Brain Res 1994; 98: 213–228.
Guertin P et al. Ankle extensor group I afferents excite extensors throughout the hindlimb during fictive locomotion in the cat. J Physiol (Lond) 1995; 487: 197–209.
McCrea DA et al. Disynaptic group I excitation of synergist ankle extensor motoneurones during fictive loco-motion in the cat. J Physiol (Lond) 1995; 487: 527–539.
Angel MJ et al. Group I extensor afferents evoke disynaptic EPSPs in cat hindlimb extensor motorneurones during fictive locomotion. J Physiol (Lond) 1996; 494: 851–861.
Duysens J et al. Medial gastrocnemius is more activated than lateral gastrocnemius in sural nerve induced reflexes during human gait. Brain Res 1996; 727: 230–232.
Pierrot-Deseilligny E et al. Pattern of group I fibre projections from ankle flexor and extensor muscles in man. Exp Brain Res 1981; 42: 337–350.
Burne JA, Lippold OC . Reflex inhibition following electrical stimulation over muscle tendons in man. Brain 1996; 119: 1107–1114.
Stephens MJ, Yang JF . Short latency, non-reciprocal group I inhibition is reduced during the stance phase of walking in humans. Brain Res 1996; 743: 24–31.
Dietz V, Muller R, Colombo G . Locomotor activity in spinal man: significance of afferent input from joint and load receptors. Brain 2002; 125: 2626–2634.
Harkema SJ . Neural plasticity after human spinal cord injury: application of locomotor training to the rehabilitation of walking. Neuroscientist 2001; 7: 455–468.
Patel UK et al. The response of neural locomotor circuits to changes in gait velocity. Soc Neurosci Abstr 1998; 24: 2104.
Cote MP, Menard A, Gossard JP . Spinal cats on the treadmill: changes in load pathways. J Neurosci 2003; 23: 2789–2796.
Pearson KG, Misiaszek JE . Use-dependent gain change in the reflex contribution to extensor activity in walking cats. Brain Res 2000; 883: 131–134.
Pearson KG . Could enhanced reflex function contribute to improving locomotion after spinal cord repair? J Physiol (Lond) 2001; 533: 75–81.
de Leon RD et al. Locomotor capacity attributable to step training versus spontaneous recovery after spinalization in adult cats. J Neurophysiol 1998; 79: 1329–1340.
de Leon RD et al. Hindlimb locomotor and postural training modulates glycinergic inhibition in the spinal cord of the adult spinal cat. J Neurophysiol 1999; 82: 359–369.
de Leon RD et al. Retention of hindlimb stepping ability in adult spinal cats after the cessation of step training. J Neurophysiol 1999; 81: 85–94.
Hodgson JA et al. Can the mammalian lumbar spinal cord learn a motor task? Med Sci Sports Exerc 1994; 26: 1491–1497.
Brown TG . On the nature of the fundamental activity of the nervous centres; together with an analysis of the conditioning of rhythmic activity in progression, and a theory of the evolution of function in the nervous system. J Physiol (Lond) 1914; 48: 18–46.
Grillner S, Zangger P . On the central generation of locomotion in the low spinal cat. Exp Brain Res 1979; 34: 241–261.
Forssberg H et al. The locomotion of the low spinal cat. II. Interlimb coordination. Acta Physiol Scand 1980; 108: 283–295.
Jankowska E et al. The effect of DOPA on the spinal cord. 5. Reciprocal organization of pathways transmitting excitatory action to alpha motoneurones of flexors and extensors. Acta Physiol Scand 1967; 70: 369–388.
Stein PS et al. Bilateral control of hindlimb scratching in the spinal turtle: contralateral spinal circuitry contributes to the normal ipsilateral motor pattern of fictive rostral scratching. J Neurosci 1995; 15: 4343–4355.
Ting LH et al. Contralateral movement and extensor force generation alter flexion phase muscle coordination in pedaling. J Neurophysiol 2000; 83: 3351–3365.
Ting LH et al. Sensorimotor state of the contralateral leg affects ipsilateral muscle coordination of pedaling. J Neurophysiol 1998; 80: 1341–1351.
Wernig A, Nanassy A, Muller S . Maintenance of locomotor abilities following Laufband (treadmill) therapy in para- and tetraplegic persons: follow-up studies. Spinal Cord 1998; 36: 744–749.
Wernig A et al. Laufband therapy based on ‘rules of spinal locomotion’ is effective in spinal cord injured persons. Eur J Neurosci 1995; 7: 823–829.
Barbeau H et al. Does neurorehabilitation play a role in the recovery of walking in neurological populations? Ann NY Acad Sci 1998; 860: 377–392.
Field-Fote EC . Spinal cord control of movement: implications for locomotor rehabilitation following spinal cord injury. Phys Ther 2000; 80: 477–484.
Dietz V et al. Locomotor pattern in paraplegic patients: training effects and recovery of spinal cord function. Spinal Cord 1998; 36: 380–390.
Leroux A, Fung J, Barbeau H . Adaptation of the walking pattern to uphill walking in normal and spinal-cord injured subjects. Exp Brain Res 1999; 126: 359–368.
Acknowledgements
We thank Roscelle Joaquin, Rita Lukacs, and Sue Ono, PT, for step training the subjects; Ani Balmanoukian, Roscelle Joaquin, Rita Lukacs, Linh Ngo, Sue Ono, PT, and Mark Roberton for help with data collection and reduction; Keir Pearson, Reggie Edgerton, Claire Farley, and Art Kuo for critical comments on earlier versions of the manuscript, and the subjects for their dedication and patience. National Institutes of Health Grants NS16333, NS36584, NS07479, NS07449, and RR00865 supported this research.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ferris, D., Gordon, K., Beres-Jones, J. et al. Muscle activation during unilateral stepping occurs in the nonstepping limb of humans with clinically complete spinal cord injury. Spinal Cord 42, 14–23 (2004). https://doi.org/10.1038/sj.sc.3101542
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101542
Keywords
This article is cited by
-
Feasibility of transcutaneous spinal direct current stimulation combined with locomotor training after spinal cord injury
Spinal Cord (2022)
-
Properties of the surface electromyogram following traumatic spinal cord injury: a scoping review
Journal of NeuroEngineering and Rehabilitation (2021)
-
Unilateral step training can drive faster learning of novel gait patterns
Scientific Reports (2020)
-
Influence of body weight unloading on human gait characteristics: a systematic review
Journal of NeuroEngineering and Rehabilitation (2018)
-
Walking reduces sensorimotor network connectivity compared to standing
Journal of NeuroEngineering and Rehabilitation (2014)