Abstract
Study design: A standardized animal model of contusive spinal cord injury (SCI) with incomplete paraplegia was used to test the hypothesis that moderate systemic hypothermia reduces neural cell death. Terminal deoxynucleotidyl transferase [TdT]-mediated deoxyuridine triphosphate [dUTP] nick-end labeling (TUNEL) staining was used as a marker of apoptosis or cell damage.
Objective: To determine whether or not moderate hypothermia could have a neuroprotective effect in neural cell death following spinal cord injury in rats.
Setting: Kagawa Medical University, Japan.
Methods: Male Sprague–Dawley (SD) rats (n=39) weighing on average 300 g (280–320 g) were used to prepare SCI models. After receiving contusive injury at T11/12, rats were killed at 24 h, 72 h, or 7 days after injury. The spinal cord was removed en bloc and of examined at five segments: 5 and 10 mm rostral to the center of injury, center of injury, and 5 and 10 mm caudal to the center of injury. Rats that received hypothermia (32°C/4 h) were killed at the same time points as those that received normothermia (37°C/3 h). The specimens were stained with hematoxylin and eosin, and subjected to in situ nick-end labeling (TUNEL), a specific method for visualizing cell death in the spinal cord.
Results: At 24 h postinjury, TUNEL positive cells (TPC) decreased significantly 10 mm rostral to center of injury in hypothermic animals compared to the normothermia group. At 72 h post-SCI, TPC also decreased significantly at 5 mm rostral, and 5 and 10 mm caudal to the lesion center compared to normothermic animals. At 7 days postinjury, a significant decrease of TPC was observed at the 5 mm rostral and 5 mm caudal sites compared to normothermic animals.
Conclusion: These results indicate that systemic hypothermia has a neuroprotective effect following SCI by attenuating post-traumatic TPC.
Similar content being viewed by others
Introduction
Several studies have confirmed two types of spinal cord injury (SCI): primary injury in which tissue damage is caused by a contusion and secondary injury in which neuronal and supporting cell death occurs over time. 1,2 Factors that could exacerbate post-traumatic secondary injury include release of excitatory toxic amino acids such as glutamate,3 ischemia,4,5,6 and lipid peroxidation in cell membrane caused by free radicals.7 However, it is not precisely known how these factors are involved in the mechanism of SCI.
Apoptosis-induced neuronal and glial cell death has been reported to occur in the spinal cord following traumatic injury.8,9 Depending on the severity of injury, post-SCI apoptosis affects a much greater extent of area than primary injury.10 In addition, similar to the phenomenon in brain, apoptotic cell death could occur and progress even a few days after the onset of ischemia.11,12 Among the therapeutic strategies, clinical and experimental effectiveness of mild-to-moderate systemic hypothermia for the treatment of central nervous system (CNS) injury due to brain injury or ischemia has been reported.13,14,15,16,17 However, a great deal remains unknown as to how hypothermia protects neuronal and supporting cells following injury. Our recent studies have also shown that hypothermia protects against neuronal cell death in experimental brain injury and ischemia models.18,19 The present study investigated the effects of moderate hypothermia on animals with traumatic SCI and attempted to evaluate whether moderate hypothermia could have a neuroprotective effect by preventing neuronal and supporting cell death.
Materials and methods
Operation and hypothermic procedures
Male Sprague–Dawley (SD) rats (n=39) with an average body weight of 300 g (280–320 g) were used to prepare SCI models. After a rat was anesthetized by administering pentobarbital sodium intraperitoneally (i.p.) (30 mg/kg), it was fixed on a surgical table and surgery was performed. A midline skin incision was made in the dorsal side, and the spinal column was exposed from T8 to L2 spinal column. The laminae of T11 and T12 were carefully removed using microrongeurs, starting from the caudal edge of the T12 lamina. After laminectomy, the dura was confirmed to be intact. The clamp was adjusted and fixed to ensure that the spinal column was horizontal with respect to the floor. Then, a 2-mm diameter metal rod weighing 25 g was placed gently centrally onto the dura of the spinal cord on the dorsal side. The compression was applied continuously for 10 min to produce a contusive injury. A preliminary experiment was conducted to examine the course of spontaneous recovery of the animal model used in this study. Injury produced by 25 g for 10 min caused complete paraplegia for 2–3 days after injury, followed by gradual recovery from around 1 week after injury. Spontaneous recovery occurred stepwise until an incomplete paraplegia model was obtained 5–6 weeks after injury.20
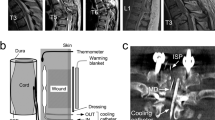
At 10 min after the end of compression, hypothermia was begun using an automatic hypothermia system to lower body temperature to a target level over a 20-min period. Body temperature was maintained at 32°C for 4 h. The animals receiving this treatment constituted the hypothermic group. Another group of rats underwent laminectomy and spinal cord compression and their body temperature was maintained at 37°C for 3 h (normothermic group). In a third group, rats underwent laminectomy without spinal cord compression and body temperature was maintained at 37°C for 1 h (sham-operated group). The experimental conditions of the three groups are summarized in Table 1.
Hypothermia was induced as reported in our previous study.21 Briefly, the hypothermic temperature control system included a program controller (FP 21; Shimaden, Tokyo, Japan), a telemetry system, two pumps (AC-2110; Atto, Tokyo, Japan), and a polyrecorder (Unicorder U-228; Nippon Denshi Kagaku Co., Kyoto, Japan). The animals were anesthetized with sodium pentobarbital (30 mg/kg, i.p.), and supplemental doses were given intermittently as necessary. The tympanic temperature was monitored with a thermotelemeter (XM-FH; Mini-Mitter, Sunriver, OR, USA) and a telemetry receiver (RLA 1020; Data Sciences International, St Paul, MN, USA). At first, the hypothermic pattern was input into the program controller. According to the program, cold or hot water was pumped to a water blanket made of silicone tubing (Laboran Silicone Tube 3 × 5 mm2; Iuchi, Osaka, Japan), which maintained the body temperature of the animal. The data were transmitted from the thermotelemeter to the telemetry receiver, and the tympanic temperature measured by the telemetry system was fed back to the program controller. The pump for cold water was activated when the tympanic temperature was above the set temperature, and that for hot water was activated when the tympanic temperature was below the set temperature. Post-traumatic hypothermia was defined as cooling at 32°C for 4 h and rewarming to 37°C for 40 min. Hypothermia was controlled by monitoring tympanic temperature and simultaneous recording of the rectal temperature. In the normothermia and sham-operated groups, body temperature was controlled at a rectal temperature of 37°C during spinal cord surgery using a feedback-controlled heating pad (Temperature controller; CMA, Stockholm, Sweden).
Hematoxylin and eosin (HE) and in situ nick-end labeling
The spinal cord was removed at 24 h, 72 h and 1 week after injury, transcardiac perfusion fixed by 4% neutral-buffered formalin solution, and then embedded in paraffin. Serial 5 μm-thick sections were prepared from each spinal cord specimen at five locations: 5 and 10 mm rostral to the center of injury, the center of injury, and 5 and 10 mm caudal to the center of injury. The sections were histologically analyzed by HE, and terminal deoxynucleotidyl transferase [TdT]-mediated deoxyuridine triphosphate [dUTP] nick-end labeling (TUNEL) staining. The TUNEL reaction detects DNA fragmentation, and was performed in accordance with a previous report.22 The neuronal and supporting cell death in injured spinal cord tissue was assessed by the TUNEL method as follows: the 3′-OH-terminal fragmented nuclear DNA was bound to biotin-labeled [dUTP] using TdT, and apoptosis was identified by enzyme labeling using avidin. We used an apoptosis detection kit ApopTag S7101 (INTERGEN Co., Purchase, NY, USA). Paraffin sections were deparaffinized and hydrated through a series of xylene, graded ethanols, and double-distilled water. The sections were treated with 20 μg/ml proteinase K in 0.1 M Tris buffer (pH 8.0) at room temperature for 15 min to strip them of nuclear proteins and then washed four times in double-distilled water for 2 min each time. After endogenous peroxidase blocking with 2% H2O2 for 5 min at room temperature, the sections were treated with equilibration buffer for few minutes, and incubated with a reaction buffer containing TdT enzyme for 60 min at 37°C. The reaction was terminated by washing the sections with stop/wash buffer for 30 min at 37°C. The sections were then washed twice with phosphate-buffered saline for 5 min before incubating in antidigoxigenin peroxidase solution for 30 min at room temperature. They were visualized with diaminobenzidine substrate working solution and then counterstained with hematoxylin.
The number of TUNEL positive cells (TPC) were counted for each section. To eliminate the artefacts due to hemorrhage and necrosis, TPC in the white matter and gray matter on the ventral side of the central canal were examined in sections from regions 5 or 10 mm rostral or caudal to the center of injury. Also, the ventral area below half of the maximum vertical diameter of the spinal cord was examined in sections from the center of injury.
All experimental procedures were performed in compliance with the guiding principles for Care and Use of Animals described in the American Journal of Physiology and the guidelines established by the Experimental Animal Facility of the Faculty of Medicine, Kagawa Medical University.
Statistical analysis
All data are expressed as mean±SEM and analyzed using the computer program Stat View (Abacus Concepts, Inc., Berkeley, CA, USA). The numbers of TPC were compared between the normothermia and hypothermia groups at the same time point using one-way analysis of variance and Fisher's protected least-significant difference test. Differences were considered to be statistically significant at the level of P<0.05.
Results
Body temperature recording
Pretraumatic and immediately post-traumatic mean rectal temperatures were maintained at almost 37°C with no significant differences among the three groups. At 30 min postinjury, rectal and tympanic temperatures were decreased to 32.0±1.1 and 32.9±0.7°C, respectively, in the hypothermic group. Tympanic temperature was maintained at 31–32°C for a further 4 h, after which the animals were rewarmed to 37°C for 40 min.
TPC distribution and effects of hypothermia by cell count
The distribution of TPC at three time points after injury and at five spinal cord regions in the normothermic, hypothermic, and sham-operated rats are shown in Figure 1. TPC were hardly detected in the sham-operated group at all three time points and five locations. Furthermore, in this group there were no significant differences in the incidence of positive cells between the central and peripheral (rostral and caudal) areas, and between the three time points after operation. For both normothermia and hypothermia groups, the numbers of TPC increased at the center of injury 24 h after injury, but there were only few TPC 5 and 10 mm rostral and caudal to the center of injury at this time (Figure 1a). At 24 h after injury and 10 mm rostral to the center, the number of TPC in the hypothermia group was significantly lower compared to the normothermia group (P<0.05) (Figure 1a).
At 72 h after injury, for both normothermia and hypothermia groups, the number of TPC did not change at the center of injury, but a tendency of increase was observed 5 and 10 mm rostral and caudal to the center of injury. Significant decreases of TPC by hypothermia were observed 5 mm rostral, and 5 and 10 mm caudal to the center of injury (P<0.05) (Figure 1b). At 1 week after injury, the number of TPC had decreased at the center of injury, but increased 5 and 10 mm rostral and caudal to the center. This tendency of increase was particularly marked 5 mm rostral and caudal to the center. The pattern of changes in TPC tended to be similar in the normothermic and hypothermic groups. At 1 week after injury, significant decreases by hypothermia were observed 5 mm rostral and caudal to the center of injury (P<0.05) (Figure 1c).
Figure 2 shows a typical example of TUNEL staining in hypothermic and normothermic rats at 1 week after SCI. In both groups, TUNEL positive apoptotic cells were found in the white matter mainly in the region 5 mm rostral to the center. TPC showing typical apoptotic bodies were present mostly in the peripheral area. The number of positive cells was significantly lower in the hypothermic group as is also shown in Figure 2A1 and A2.
TUNEL staining photomicrographs showing cross-sections of the 5 mm rostral side to the center of injury, 1 week after injury in hypothermic (a) and normothermic (b) rats. (A1) Original magnification × 40. (A2) Enlarged area from the square in Figure A1; original magnification × 400. (B1) Original magnification × 40. (B2) Enlarged area from the square in Figure B1; original magnification × 400. Bar=500 μm (A1, B1) and 100 μm (A2, B2)
Discussion
Previous studies have demonstrated various mechanisms underlying the effectiveness of hypothermia in mitigating SCI, such as decrease of vasogenic edema to reduce extravasation of fibrinogen and fibronectin,23 inhibition of polymorphonuclear leukocyte infiltration and accumulation,24 and suppression of signaling impairment in the white matter25,26 or neuronal impairment in the gray matter.27
The results of the present study showed that at 24 and 72 h after injury, the numbers of TPC in injured spinal cord were high at the center of injury, but low in regions 5 and 10 mm rostral and caudal to the center. However, at 1 week after injury, the numbers of TPC had decreased at the center of injury, but increased 5 and 10 mm rostral and caudal to the center. These findings reflect the biphasic nature of the pathophysiology of SCI; namely, primary injury and secondary injury, and suggest that the changes in numbers of TPC during SCI may be related to apoptosis.
A limitation of TUNEL staining is that not all TPC are equivalent to apoptotic cells and TUNEL staining may reveal only some of the apoptotic characteristics. TUNEL and ISNEL: in situ end labeling28 are the major methods used for in situ detection of DNA fragmentation in oligonucleosome units.29 Since TdT is used in TUNEL staining, the presence of 3′-OH terminal in DNA is additively labeled with time, and may give a positive staining reaction. Furthermore, DNA fragmentation also occurs in necrosis.30 For this reason, we paid attention to perform TUNEL staining always under constant conditions of reaction time, reagent concentrations and room temperature.
HE-stained sections appeared to be normal 10 mm rostral and caudal to the center of injury (data not shown), but TPC were seen at these areas, thus suggesting that cell death is more widespread than expected. As to the effects of hypothermia on SCI from the viewpoint of the neuronal and supporting cell death, the numbers of TPC in the peripheral regions of injury 24 h, 72 h, and 1 week after injury were significantly lower in the hypothermia group compared to the normothermia group, demonstrating that hypothermia suppressed the onset of delayed cell death following SCI. However, we also detected a small but significant decrease in TPC only in the region 10 mm rostral to the lesion center 24 h post-SCI. Li et al10 also observed a tendency of early increase of apoptotic cells in areas remote from the injury site 4 h to 1 day after injury. Baldwin et al31 compared the oxidative stress and blood–spinal cord barrier breach between equidistant areas on the rostral and caudal sides, and found that injury was less severe on the rostral side. In our SCI model, the region 10 mm rostral to the lesion might be least affected by the trauma at 24 h post-SCI.
Apoptosis may occur from several hours to several days after injury in some locations,32 thus the suppression of cell death is clinically relevant. Following SCI, apoptosis appears in the vicinity of the area affected by mechanical contusion, and since the chronological course of cell death is controlled, delayed cell death in spinal white matter somewhat specifically affects oligodendrocytes.33,34 Oligodendroglial apoptosis is known to be associated with upregulation of caspase-3 for signaling in apoptosis35 as well as FAS and p75 expression,36 and has been shown to be related to progression of white matter degeneration.37 In other words, the decrease of apoptotic cell death by hypothermia may reduce myelin damage, and contribute to the recovery of neurologic function. Previous studies reported that administration of MK-801 and/or a competitive inhibitor (L-Ng-nitro-arginine methylester) of nitric oxide synthase (NOS) resulted in a reduction of TPC following SCI.38,39 Furthermore, the NOS inhibitor was effective for the recovery of neurologic function following SCI, suggesting that NO induced by NOS could be cytotoxic in the subacute phase of SCI.40 However, the effect of hypothermia on SCI has not been investigated so far.
Several mechanisms could explain how hypothermia might have a neuroprotective effect following SCI. In the case of cerebral ischemia, hypothermia inhibits the increase in the extracellular concentration of glutamate,41 and this increase is strongly temperature dependent.42 Elevated excitatory amino-acid release also causes neurological dysfunction in SCI models, and when cultured spinal cord cells are exposed to glutamate for 5 min, loss of neuronal cells is observed 24 h later.43 An injection of kynurenate into the subarachnoid space following SCI improves motor function.44 The administration of NBQX (a non-NMDA receptor antagonist) within 4 h of injury improves neurological prognosis.45 Therefore, inhibition of post-traumatic glutamate release may be one of the possible mechanisms of the neuroprotective effect of hypothermia. Although systemic hypothermia has been reported to have a neuroprotective effect through inhibiting TPC, the pyramidal tract in rodents runs in ventral region of the dorsal column.46 Therefore, this effect on motor functional recovery requires further investigation.
Conclusion
The present study shows that moderate systemic hypothermia may have beneficial effects on the outcome of SCI by inhibiting TPC in the peripheral areas of spinal cord. In the future, the effectiveness of hypothermia should be investigated by determining the therapeutic time window of effective systemic hypothermia, the neural protective effects of prolonged hypothermia, and the effects of functional recovery.
References
Anderson DK, Hall ED . Pathophysiology of spinal cord trauma. Ann Emerg Med 1993; 22: 987–992.
Tator CH . Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 1995; 5: 407–413.
Faden AI, Simon RP . A potential role for excitotoxins in the pathophysiology of spinal cord injury. Ann Neurol 1988; 23: 623–626.
Griffiths IR, Burns N, Crawford AR . Early vascular changes in the spinal gray matter following impact injury. Acta Neuropathol (Berl) 1978; 19: 33–39.
Rivlin AS, Tator CH . Regional spinal cord blood flow in rats after severe cord trauma. J Neurosurg 1978; 49: 844–853.
Wallace MC, Tator CH, Frazee P . Relationship between posttraumatic ischemia and hemorrhage in the injured rat spinal cord as shown by colloidal carbon angiography. Neurosurgery 1986; 18: 433–439.
Hall ED, Braughler JM . Role of lipid peroxidation in post-traumatic spinal cord degeneration: a review. Central Nervous Syst Trauma 1986; 3: 281–294.
Katoh K et al. Induction and its spread of apoptosis in rat spinal cord after mechanical trauma. Neurosci Lett 1996; 20: 9–12.
Li GL et al. Apoptosis and expression of Bcl-2 after compression trauma to rat spinal cord. J Neuropathol Exp Neurol 1996; 55: 280–289.
Li GL, Farooque M, Holtz A, Olsson Y . Apoptosis of oligodendrocyte occurs for long distances away from the primary injury after compression trauma to rat spinal cord. Acta Neuropathol (Berl) 1999; 98: 473–480.
Kirino T . Delayed neuronal death in the gerbil hippocampus following ischemia. Brain Res 1982; 6: 57–69.
Nitatori T et al. Delayed neuronal death in the CA1 pyramidal cell layer of the gerbil hippocampus following transient ischemia is apoptosis. J Neurosci 1995; 15: 1001–1011.
Clifton GL et al. Marked protection by moderate hypothermia after experimental traumatic brain injury. J Cereb Blood Flow Metab 1991; 11: 114–121.
Colbourne F, Corbett D . Delayed and prolonged post-ischemic hypothermia is neuroprotective in the gerbil. Brain Res 1994; 22: 265–272.
Dietrich WD et al. Post-traumatic brain hypothermia reduces histopathological damage following concussive brain injury in the rat. Acta Neuropathol (Berl) 1994; 87: 250–258.
Marion DW et al. The use of moderate therapeutic hypothermia for patients with severe head injuries: a preliminary report. J Neurosurg 1993; 79: 354–362.
Shiozaki T et al. Effect of mild hypothermia on uncontrollable intracranial hypertension after severe head injury. J Neurosurg 1993; 79: 363–368.
Miyamoto O et al. Depression of long term potentiation in gerbil hippocampus following postischemic hypothermia. Brain Res 2000; 4: 168–172.
Xu RX et al. Specific inhibition of apoptosis after cold-induced brain injury by moderate postinjury hypothermia. Neurosurgery 1998; 43: 107–114.
Shibuya S et al. Embryonic intermediate filament, nestin, expression following traumatic spinal cord injury in adult rats. Neurosci 2002; 114: 905–916.
Nakamura T et al. Influence of rewarming conditions after hypothermia in gerbils with transient forebrain ischemia. J Neurosurg 1999; 91: 114–120.
Gavrieli Y, Sherman Y, Ben-Sasson SA . Identification of programmed cell death in situ via specific labeling of nuclear DNA fragmentation. J Cell Biol 1992; 119: 493–501.
Yu WR et al. Systemic hypothermia following compression injury of rat spinal cord: reduction of plasma protein extravasation demonstrated by immunohistochemistry. Acta Neuropathol (Berl) 1999; 98: 15–21.
Chatzipanteli K et al. Posttraumatic hypothermia reduces polymorphonuclear leukocyte accumulation following spinal cord injury in rats. J Neurotrauma 2000; 17: 321–332.
Jou IM . Effects of core body temperature on changes in spinal somatosensory-evoked potential in acute spinal cord compression injury: an experimental study in the rat. Spine 2000; 25: 1878–1885.
Westergren H et al. Systemic hypothermia following spinal cord compression injury in the rat: axonal changes studied by beta-APP, ubiquitin, and PGP 9.5 immunohistochemistry. Spinal Cord 1999; 37: 696–704.
Yu WR et al. Systemic hypothermia following spinal cord compression injury in the rat: an immunohisto-chemical study on MAP 2 with special reference to dendrite changes. Acta Neuropathol (Berl) 2000; 100: 546–552.
Wijsman JH et al. A new method to detect apoptosis in paraffin sections: in situ end-labeling of fragmented DNA. J Histochem Cytochem 1993; 41: 7–12.
Ben-Sasson SA, Sherman Y, Gavrieli Y . Identification of dying cells – in situ staining. Methods Cell Biol 1995; 46: 29–39.
Hayashi R et al. Quantitative differentiation of both free 3′-OH and 5′-OH DNA ends between heat-induced apoptosis and necrosis. J Histochem Cytochem 1998; 46: 1051–1059.
Baldwin SA et al. The presence of 4-hydroxynonenal/protein complex as an indicator of oxidative stress after experimental spinal cord contusion in a rat model. J Neurosurg 1998; 88: 874–883.
Crowe MJ et al. Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat Med 1997; 3: 73–76.
Abe Y et al. Apoptotic cells associated with Wallerian degeneration after experimental spinal cord injury: a possible mechanism of oligodendroglial death. J Neurotrauma 1999; 16: 945–952.
Shuman SL, Bresnahan JC, Beattie MS . Apoptosis of microglia and oligodendrocytes after spinal cord contusion in rats. J Neurosci Res 1997; 1: 798–808.
Citron BA et al. Rapid upregulation of caspase-3 in rat spinal cord after injury: mRNA, protein, and cellular localization correlates with apoptotic cell death. Exp Neurol 2000; 166: 213–226.
Casha S, Yu WR, Fehlings MG . Oligodendroglial apoptosis occurs along degenerating axons and is associated with FAS and p75 expression following spinal cord injury in the rat. Neurosciences 2001; 103: 203–218.
Warden P et al. Delayed glial cell death following Wallerian degeneration in white matter tracts after spinal cord dorsal column cordotomy in adult rats. Exp Neurol 2001; 168: 213–224.
Satake K et al. Nitric oxide via macrophage iNOS induces apoptosis following traumatic spinal cord injury. Brain Res Mol Brain Res 2000; 85: 114–122.
Wada S et al. Apoptosis following spinal cord injury in rats and preventative effect of N-methyl-D-asparate receptor antagonist. J Neurosurg 1999; 91: 98–104.
Hamada Y et al. Roles of nitric oxide in compression injury of rat spinal cord. Free Radio Biol Med 1996; 20: 1–9.
Mitani A, Kataoka K . Critical levels of extracellular glutamate mediating gerbil hippocampal delayed neuronal death during hypothermia: brain microdialysis study. Neurosci 1991; 42: 661–670.
Busto R et al. Effect of mild hypothermia on ischemia-induced release of neurotransmitters and fatty acids in rat brain. Stroke 1989; 20: 904–910.
Choi DW . Ionic dependence of glutamate neurotoxicity. J Neurosci 1987; 7: 369–379.
Wrathall JR, Bouzoukis J, Choiniere D . Effect of kynurenate on functional deficits resulting from traumatic spinal cord injury. Eur J Pharmacol 1992; 6: 273–281.
Wrathall JR, Choiniere D, Teng YD . Dose-dependent reduction of tissue loss and functional impairment after spinal cord trauma with the AMPA/kainate antagonist NBQX. J Neurosci 1994; 14: 6598–6607.
Liang FY, Moret V, Wiesendanger M, Rouiller EM . Corticomotoneuronal connections in the rat: evidence from double-labeling of motoneurons and corticospinal axon arborizations. J Comp Neurol 1991; 311: 356–366.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Shibuya, S., Miyamoto, O., Janjua, N. et al. Post-traumatic moderate systemic hypothermia reduces TUNEL positive cells following spinal cord injury in rat. Spinal Cord 42, 29–34 (2004). https://doi.org/10.1038/sj.sc.3101516
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101516
Keywords
This article is cited by
-
Effects of local hypothermia–rewarming on physiology, metabolism and inflammation of acutely injured human spinal cord
Scientific Reports (2020)
-
Targeted Perfusion Therapy in Spinal Cord Trauma
Neurotherapeutics (2020)
-
Post-traumatic moderate systemic hyperthermia worsens behavioural outcome after spinal cord injury in the rat
Spinal Cord (2006)