Abstract
Study design: Prospective 2 years survey from 1 February 1997 to 31 January 1999.
Objectives: To assess the incidence of complications during the acute stage of spinal cord lesions and the possible correlations between them and the type of care and rehabilitation provided.
Setting: Spinal cord injured patients consecutively admitted to 37 Italian Rehabilitation Centres (RCs).
Methods: The study population was drawn from the GISEM (Italian Group for the Epidemiological Study of Spinal Cord Injuries) study (1997–1999), which involved the participation of 37 RCs and Spinal Units (SUs), situated all over Italy, mainly in the northern and central part of the country. Only patients admitted within 60 days from the traumatic injury were considered. This yielded a population of 588 patients (18% females and 82% males). Six of the most common complications were considered: trophic skin changes, heterotopic ossifications, urinary complications, respiratory complications, deep-vein thrombosis and pulmonary embolism.
Results: Results revealed a high incidence of trophic skin changes (23.3%), while over half of the patients presented at least one of the complications under examination. Trophic skin changes occurred exclusively among the patients whose admission to the SUs had been delayed or who had received initial treatment in nonspecialised Centres.
Conclusions: Optimal rehabilitation care, with regard to the prevention of complications during the acute phase, entails early admission to a specialised multidisciplinary facility, namely an SU.
Similar content being viewed by others
Introduction
Despite noteworthy advances in the prevention and treatment of spinal cord injuries (SCI), a variety of distressing complications can occur both during the acute phase and long after injury.1,2,3
Such pathological situations can create substantial medical problems (with unfavourable prognostic consequences in terms of both mortality and neurological and functional recovery) as well as psychosocial (loss of social life, depression and isolation) and financial hardship.4 Over the last 50 years, the prevention of complications during the acute phase of SCI has represented a cornerstone for the health-care personnel involved in the care of patients of this kind.
Aims of the study
The aims of the study were to examine the incidence of the most common complications among patients with post-traumatic spinal cord lesions and to explore possible correlations with the time lapse from injury to admission to a specialised centre, and possible differences in the incidence of complications among the three types of centres that participated in the study.
Materials and methods
In the period 1 February 1997 to 1 February 1999, GISEM (Italian Group for the Epidemiological Study of Spinal Cord Injuries) conducted an epidemiological study on spinal cord injured patients for the purpose of creating a national database. A total of 37 centres participated, including all of the Italian Spinal Units (SUs) and the most important General Rehabilitation Centres (RCs) having beds dedicated to the care of paratetraplegia.
Each centre received a questionnaire to complete in order to establish the exact type of health-care facility they could be classified as. Seven centres were classified as SUs (the entire course of treatment is completed within the same structure, from immediately after injury to the final discharge home); 25 were classified as General RCs (able to provide rehabilitation treatment during the postacute phase but unable to treat patients during the early acute phase), while the remaining five centres were defined as Rehabilitation Service (RS) (structure capable of providing treatment in other wards but without beds designated to SCI at their disposal). No information was collected regarding the availability of specific facilities such as special beds or mattresses, or intensive respiratory therapy, that are surely available in SU. The data collected regarded all SCI patients with either traumatic or nontraumatic aetiologies admitted to these structures during the study period. The data were recorded on a computerised clinical form consisting of 80 items concerning personal data, detailed information on the injury, medical and/or surgical treatment received during the acute phase, treatment in other centres, clinical status and complications on admission, neurological classification according to the ASIA/ISCOS criteria,5 clinical complications during treatment, and medical, social and psychological status at the final discharge.
Every 3 months, data from each centre were sent to the coordinating Centre for analysis. Every 6 months, the scientific committee held a meeting to review the data and to make any necessary changes to the aims of the study.
In this way, 2210 forms were collected, relative to 1930 patients. Of these, in this study we included only patients with traumatic SCI who were admitted for the first time to one of the aforementioned centres within 60 days of injury.
In turn, they were subdivided into five groups according to the time lapse from injury to admission:
-
1)
within 48 h;
-
2)
48 h–1 week;
-
3)
1–2 weeks;
-
4)
15–30 days;
-
5)
30–60 days after injury.
Listed below are the six types of medical complications present on admission or occurring during hospitalisation that were taken into consideration and recorded:
-
Trophic skin changes:6,7 The presence of at least one sore (irrespective of the type according to the Ennis and Sarmento classification). The mildest form of trophic skin changes should have appeared as a lesion presenting an area of redness that did not whiten when touched or pressed.
-
Heterotopic ossifications:8,9 Confirmed by X-ray and/or bone scintigraphy.
-
Urinary complications:10,11,12 All urinary tract disorders, except, of course, the presence of neurogenic bladder disorders. Various diagnostic techniques were used including urography, retrograde cystography, renal CT, renal scintigraphy, blood tests, etc.
-
Respiratory complications:13,14,15 Atelectasis, pneumonia, chest effusions diagnosed by chest X-ray and/or pulmonary CT.
-
Pulmonary embolism:16 Confirmed by pulmonary perfusion scintigraphy.
-
Deep-vein thrombosis:17 Deep-vein occlusion of the lower limbs confirmed by echo-colour Doppler or venography.
Data analyses were performed using Pearson's χ test. The significance level was set at P<0.05. Some of these data are presented in Tables 1, 2, 3 and 4 and in Figure 5.
Results
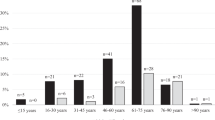
A total of 588 subjects were included in the study: 112 females (19%) and 476 males (81%) (Figure 1). The mean age of the subjects at the time of injury was 38.9 years.
There were 322 (56.5%) paraplegics and 238 (40.5%) (Figure 2) tetraplegics; 291 (49%) were neurologically complete (ASIA Impairment Scale: A) and 297 were incomplete (B: 11.4%; C: 23.3%; D: 13.4%; E: 1.9%) (Figure 3). Causes of injuries, as shown in Figure 4, were:
-
Car accidents (35.2%).
-
Motorbike accidents (15%).
-
Cycling or pedestrian accidents (3.6%).
-
Sports (8.2%).
-
Assaults (1.7%).
-
Suicide attempts (4.1%).
-
Other causes (32%).
-
Unknown causes (0.2%).
A high incidence of at least one complication on admission was documented. This occurred in 25.3% of the patients admitted to SUs, in 39.9% of those admitted to General RCs and in 25% of those treated by the RS (see Table 1).
The most common complication detected on admission was trophic skin changes, which were present in 15.5% of the patients admitted to SU, 29.6% of those admitted to General RCs with dedicated beds (RC) and 20.5% of those treated by RS. Its presence was strongly influenced by the type of lesion (more frequent in complete lesions (33.9%) than in incomplete ones (13%), see Table 2).
Heterotopic ossifications were observed on admission in 6.9% of the patients admitted to the SUs, and in 1.3% of those admitted to RCs. Their incidence was strongly influenced by the type of lesion (more frequent in complete lesions than in incomplete ones, as seen in Table 2).
Urinary complications were reported in 2.1% of the admissions to the SU, 8.7% of the admissions to the RCs, and 2.3% of the admissions to RSs. They were not significantly influenced by the type of lesion (complete versus incomplete) (see Tables, 2).
Respiratory complications on admission were notably more common in those patients admitted to the SU and RCs (9.4 and 12.5%, respectively) than in those treated by RSs (2.3%). Their incidence was strongly influenced by the type of lesion, so that they were more frequent in complete lesions (17.2%) than in incomplete ones (7.6%), as seen in Table 2.
Deep-vein thrombosis was observed in 1.3% of the patients admitted to SU and in 5.5% of the patients on admission to the RCs, and were absent in the others. Its incidence was not statistically correlated to the completeness of lesions (4.9% in complete versus 2.7% in incomplete).
Six episodes of pulmonary embolism were reported: five by General RCs and one by an SU.
As shown in Table 1, several complications such as trophic skin changes, heterotopic ossifications and urological disorders were already present on admission. It should be noted that there was a high incidence of respiratory complications in patients who were admitted to the SUs. This is to be interpreted as a direct consequence of the higher severity of the patients referred to these specialised centres.
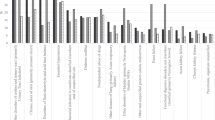
As can be seen in Figure 5, the longer the delay from injury to admission to the structures, the greater the incidence of the complications. The presence of at least one complication rose from 8.9% among patients admitted within 48 h of injury to 15.5% among those admitted 7–14 days postinjury, to 38.6% among those admitted 15–30 days postinjury, up to 49.8% among those admitted 30–60 days postinjury. The increase in the incidence of pressure sores, heterotopic ossifications and urinary complications was particularly marked.
No statistically significant differences were observed for the other complications taken into consideration in our study, with regard to the delay between injury and admission.
As shown in Table 3, the incidence of trophic skin changes occurring during hospitalisation in the SUs (3.4%) was less than half that observed in the General RCs (7.4%), and a quarter of that observed in the RSs without beds (13.6%). There were no significant differences in the occurrence of heterotopic ossification or urological complications. The incidence of respiratory complications during hospitalisation was similar when the SU (9.9%) and the General RCs (7.4%) were compared. This finding may be due to the higher incidence of such complications particularly during the very acute phase (SUs usually accept patients earlier after injury) and among patients with more severe injuries who are not usually referred to nonspecialised centres. A significant increase was found, however, on comparing the RSs without beds (22.7%).
No significant difference in the incidence of deep-vein thrombosis and pulmonary embolism has been reported among the patients staying in the three different structures (Table 3). This finding is probably due to the less systematic investigations performed in the RC and RS compared to the SU.
The incidence of trophic skin changes that occurred during hospitalisation was significantly higher in complete versus. incomplete lesions (9.4 versus 3.4%, see Table 4). The same finding has been detected with regard to heterotopic ossifications (5.9 versus 2.1%, see Table 4), urinary complications (12.6 versus 5.2%, see Table 4) and respiratory complications (14.9 versus 4.5%, see Table 4). No statistically significant difference has been reported in the incidence of deep-vein thrombosis and pulmonary embolism when complete and incomplete lesions occurring during hospitalization were compared.
Discussion and conclusions
The comparison of the GISEM study results and those of the European literature shows that, on the whole, the present SCI patients received an acceptable standard of treatment aimed at tertiary prevention. However, the same cannot be said if one considers the extremely high incidence of trophic skin changes or sores.
As if any further proof were necessary, the analysis of our data further supports the contention that early admission to an SU is the surest way of preventing complications during the acute phase. It can dramatically reduce the incidence of complications, which in addition to creating difficulties for the patients and the structures to which they are admitted, worsen an already difficult situation.
It should be noted that the described situation is relative to a population treated in centres and hospitals mostly in central and northern Italy. Since just one center from southern Italy participated in the study, it is reasonable to assert that secondary and tertiary prevention in the Southern part of Italy and on the islands, where no SU is available, is still very poor. Our hope is that a uniform standard of SCI treatment will soon be provided throughout the country, in the certainty that this will serve to improve the quality of other national facilities, and no longer be forced to cope with the treatment and medical care emergencies of Italy's southern population.
GISEM Scientific Committee
M Franceschini, S Aito, MG Celani, A Citterio, G Finali, D Loria, MC Pagliacci, S Ricci, M Taricco, L Spizzichino, M Zampolini.
Participating Centres and local referees:
-
Clinica di Neuroriabilitazione, Ancona: L Provinciali, M Danni
-
SRRF Ospedale Maggiore, Parma: M Boselli, M Franceschini
-
SRRF Policlinico S Orsola Malpighi, Bologna: M Menarini, M Alianti L Landi
-
SRRF Ospedale Bellaria, Bologna: MP Ferrari, G Domenicucci
-
DRRF Ospedale Maggiore, Bologna: R Piperno, N Battisti.
-
Centro Paraplegici Ospedale di Ostia: DA Fletzer, M Magnini
-
Centro Medico Cassano Murge – IRCCS, Cassano Murge(BA): R Nardulli, S Calabrese, E Lo Savio
-
Unitá Spinale – CTO, Firenze: S Aito
-
Casa di Cura ‘Luce sul Mare’, Igea Marina: A Battistini, L Betti
-
Centro di Riabilitazione ‘Villa Beretta’ – Ospedale Valduce, Costamasnaga: N Cellotto, A Lissoni, M Cazzaniga, F Molteni, L Suardi
-
Ospedale di Riabilitazione di Longone al Segrino, Longone al Segrino: M Almici
-
Sezione Mielolesi, Magenta: Magnaghi, A Zanollo, Zucchi, Tagliabue, F Politi
-
UORRF Ospedale Civile, Legnano: G Alberti
-
Istituto di Terapia Fisica e Riabilitazione, Milano: T Redaelli, E Radaelli, C Gallo, F Santagostini
-
Divisione Paraplegici – CTO, Milano: A Bava, CM Borghi
-
SRRF Ospedale di Bergamo – Sezione Mozzo, Mozzo: I Ghislandi, M Ceravolo, G Molinero
-
Centro di Riabilitazione ‘S Stefano’, P Potenza Picena: M Menichetti, M Vallasciani, M Rabuini, G Leone, S Spurio
-
Servizio Riabilitazione Ortopedica, Padova: D Primon, M Ortolani, Arrigo Baldo, M Gulgelmetto
-
Ospedale Casati, Passirana di Rho: M Taricco, Ranieri, R Adone, S Di Carlo, A Ferrari, MG Maringelli
-
Centro Medico Montescano, Pavia: C Pistarini, C Rampulla, A Contardi
-
Ospedale Villa Rosa — CRF, Pergine Valsugana: R Albertazzi, A Mosetti
-
Unitá Spinale Unipolare – Ospedale Silvestrini, Perugia: MC Pagliacci, G Finali
-
Unitá di Neuroriabilitazione Clinica neurologica Ospedale S Chiara, Pisa: G Stampacchia, B Rossi
-
SRRF Ospedale SM delle Croci, Ravenna: G Gatta, S Tibaldi, G Cortese
-
IRCCS Santa Lucia, Roma: G Scivoletto, V Castellano
-
Unitá Spinale Unipolare CTO, Roma: V Santilli, Trigila, M Vinciguerra
-
Unitá Spinale, Sondalo: E Occhi, F Gualzetti
-
Unitá Spinale, Torino: D Loria, V Filipello, S Negri, L Olino
-
U.O. di Riabilitazione Intensiva Neuromotoria, Trevi: S Baratta, M Zampolini, MG Celani
-
Centro di Riabilitazione, Trieste: P Di Benedetto, R Piccinino
-
Istituto di Medicina Fisica e Riabilitazione, Udine: M Saccavini, L Lovati A Zampa
-
Reparto di RRF Ospedale ‘Sacro Cuore-Don Calabria’, Negrar: Z Cordioli, G Salvi, R Avesani
-
UORRF Unita Spinale Ospedale San Bortolo, Vicenza: M Leucci, M Menarini
-
Centro di Recupero e Rieducazione Funzionale, Villanova d’Arda: S Lotta, D Nicolotti, R Bocchi
-
Clinica Villa delle Magnolie, Castel Morrone: N Avena, M Esposito, P Sabino, C Limardi
-
Istituto scienze neurologiche, Catania: A Reggo
-
Istituto Riabilitazione Neuromotoria, Mezzaselva di Roana: C Strazzabosco, C Guerriero
References
Johnson RL et al. Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1996; 36: 45–50.
Chen D, Apple DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury. Current experience of the model systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Bergman SB, Yarkony GM, Stients SA . Spinal cord injury rehabilitation. Medical complications. Arch Phys Med Rehabil 1997; Mar, 78 (Suppl) S53–S58.
Johnson RL, Whiteneck GG, Brooks CA . Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord 1996; 34: 470–480.
Ditunno JF, Young W, Donovan WH, Creasey G . The international standars booklet for neurological and functional classification of spinal cord injury. Paraplegia 1994; 32: 70–80.
Enis JF, Sarmiento A . The pathophysiology and management of pressure sores. Orthop Rev 1973; 2: 25–34.
Yarkony GM, Heinemann AW . Pressure ulcers. In: Stover SL, DeLisa JA, Whiteneck GG (ed). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersburg, MD 1995, pp. 100–119.
Ucnelhart D, Demiaux-Domenech B, Rtoh M, Chantraine A . Bone metabolism in spinal cord injured individuals and in others who have prolonged immobilization. a review. Paraplegia 1995; 33: 669–673.
Bruin ED et al. Changes of tibia bone properties after spinal cord injury: effects of early intervention. Arch Phys Med Rehabil 1999; 80: 214–220.
Kuhlemeier KV et al. Renal function after acute and chronic spinal cord injury. J Urol 1984; 131: 443–446.
Wheeler Jr JS, Walter JW . Acute urologic management of the patient with spinal cord injury. Initial hospitalization. Urol Clin North Am 1993; 20: 403–411.
Stover SL, Lloyd LK, Waites KB, Jackson AH . Urinary tract infections in spinal cord injury. Arch Phys Med Rehabil 1989; 70: 47–54.
Ragnarsson KT, Hall KM, Wilmot CB, Carter RE . Management of pulmonary, cardiovascular, and metabolic conditions after spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersburg, MD 1995, pp 79–99.
Mnsel JK, Norman JR . Respiratory complications and management of spinal cord injuries. Chest 1990; 97: 1446–1452.
Carter RE . Respiratory aspects of spinal cord injury management. Paraplegia 1987; 25: 262–266.
Jackson AB, Groomes TE . Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 1994; 75: 270–275.
Consortium for Spinal Cord Medicine . Prevention of Thromboembolism in Spinal Cord Injury. Paralyzed Veterans of America: Washington, DC 1997.
Author information
Authors and Affiliations
Consortia
Rights and permissions
About this article
Cite this article
Aito, S., on behalf of the ‘Gruppo Italiano Studio Epidemiologico Mielolesioni’ GISEM group. Complications during the acute phase of traumatic spinal cord lesions. Spinal Cord 41, 629–635 (2003). https://doi.org/10.1038/sj.sc.3101513
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101513
Keywords
This article is cited by
-
Epidemiological characteristics and early complications after spinal cord injury in Former Yugoslav Republic of Macedonia
Spinal Cord (2020)
-
The effects of early or direct admission to a specialised spinal injury unit on outcomes after acute traumatic spinal cord injury
Spinal Cord (2017)
-
Right care, right time, right place: improving outcomes for people with spinal cord injury through early access to intervention and improved access to specialised care: study protocol
BMC Health Services Research (2014)
-
The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate
Spinal Cord (2014)
-
Reliability of the spine adverse events severity system (SAVES) for individuals with traumatic spinal cord injury
Spinal Cord (2014)