Abstract
Study design: A case report of Neisseria sicca/subflava discitis in a healthy elderly female.
Objective: To report a rare case, which is usually seen exclusively in children.
Setting: Stoke on Trent, England.
Method: Case report, a 65-year-old female with a 6 month history of back and bilateral leg pain. X-rays showed collapse of L4/5 disc. No neurological deficit. Magnetic resonance imaging supported the clinical suspicion of discitis. Percutaneous biopsy followed 2 weeks later by open biopsy with bilateral root decompression was performed. Culture of L4/5 disc tissue produced Neisseria sicca/subflava. The patient was treated with a 4-week course of intravenous amoxycillin. Follow-up at 3 months confirmed clinical resolution of original symptoms.
Conclusion: Any organism cultured from biopsy needs to be interpreted within the context of the clinical case. If clinical suspicion is high, further weight must be added to the finding of unusual or environmental organisms and culture of a repeat aspirate or biopsy may clarify the significance.
Similar content being viewed by others
Case report
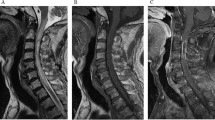
A previously fit and well 65-year-old female with no concurrent illnesses was referred with a history of 6 months of mid-back and bilateral leg pain. Plain radiographs revealed collapse of disc height at L4/L5 with inferior and superior end plate erosion, respectively (see Figure 1). No neurological deficit could be elicited on examination. Blood investigations demonstrated a minimally raised erythrocyte sedimentation rate at 21 mm/h (normal upper range <20 mm/h), a normal C-reactive protein of 4 mmol (normal range <6 mmol) and normal white cell count. Magnetic resonance imaging (MRI) was performed, which supported the clinical suspicion of discitis with exit foramen stenosis of undetermined cause. A percutaneous Tru-Cut biopsy, 20 mm specimen notch, (Allegiance Healthcare Corporation, IL, USA) was performed under general anaesthetic, and image intensifier guidance. Tru-Cut tissue specimens were sent for histological and microbiological evaluation. With further fine-needle aspirate and Tru-Cut instrument swab sent for microbiology. Culture for Mycobacterium remained negative. Culture of a Tru-Cut instrument swab and spine disc fluid showed no growth after 48 h and 5 days of incubation, respectively. However, culture of disc biopsy tissue produced a scanty growth of Neisseria species that was reported as a probable contaminant. With clinical and radiological suspicion of infection but no identification of a common causative organism, 2 weeks later an open biopsy with bilateral root decompression was performed. Cultures for Mycobacteria and culture of disc tissue remained negative. However, culture of L4/L5 disc tissue again produced Neisseria species, identified as Neisseria sicca/subflava by the laboratory of Hospital Infection, PHLS Central Public Health laboratory, London, UK for both specimens. The two isolates had a similar biochemical pattern, did not produce β-lactamase, and the minimum inhibitory concentration (MIC) for penicillin was 0.5 mg/l, amoxycillin 0.5 mg/l and cefotaxime 0.047 mg/l. The patient was treated with a 4-week course of intravenous amoxycillin (500 mg TDS) and discharged with a further 6-week course of oral amoxycillin (250 mg TDS), resulting in a clinical resolution of symptoms. Follow-up at 3 months confirmed continued clinical resolution of the original symptoms and discharge from outpatient clinic. Laboratory response to treatment could not be quantified, as parameters were normal within experimental error and laboratory reproducibility before, during and after treatment.
Discussion
Infective discitis is a relatively common cause of morbidity; the challenge arises in establishing the causative organism. Difficulty in obtaining tissue for culture and unsuccessful culture despite high clinical suspicions confound this challenge.1,2,3,4
Neisseria sicca/subflava is a slow-growing, fastidious Gram negative diplococcus that can be found as a common inhabitant of the oral cavity. It very rarely causes orthopaedic infections, seen almost exclusively in children as septic arthritis or osteomyelitis.5 Discitis caused by this organism has not been previously reported to the best of our knowledge, following an Ovid-based Medline search incorporating keywords Neisseria sicca/subflava, discitis. Previous authors have reported meningitis, peritonitis, endocarditis and bacteraemia,6,7,8,9 the majority occurring in immunocompromised individuals.
Any organism cultured from a discovertebral biopsy needs to be interpreted within the context of the clinical case and other supportive laboratory evidence. If clinical suspicion is high, further weight must be added to the finding of even unusual4 or environmental organisms to avoid false-negative reporting. If the significance of the cultured organism remains doubtful and antibiotics have not yet been given, culture of a repeat aspirate or biopsy may clarify the significance of the finding.
References
Chew FS, Kline MJ . Diagnostic yield of CT-guided percutaneous aspiration procedures in suspect spontaneous infectious discitis. Radiology 2001; 218: 211–214.
Fouquet B et al. Infectious discitis diagnostic contribution of laboratory tests and percutaneous discovertebral biopsy. Rev Rhum Engl Ed 1996; 63: 24–29.
McCain GA et al. Septic discitis. J Rheumatol 1981; 8: 100–109.
Noordeen MH, Godfrey LW . Case report of an unusual cause of back pain. Intervertebral discitis caused by Eikenella corrodens. Clin Orthop 1992; 280: 175–178.
Obeid EM . Neisseria subflava causing septic arthritis of the ankle in a child. J Infect 1993; 27: 100–101.
Baraldes MA et al. Meningitis due to Neisseria subflava: case report and review. Clin Infect Dis 2000; 30: 615–617.
Vermeij CG, Van Dam DW, Oosterkamp HM, Verburgh CA . Neisseria subflava biovar perflava peritonitis in a continuous cyclic peritoneal dialysis patient. Nephrol Dial Transplant 1999; 14: 1608.
Amsel BJ, Moulijn AC . Nonfebrile mitral valve endocarditis due to Neisseria subflava. Chest 1996; 109: 280–282.
Domingo P et al. Neisseria subflava bacteraemia in a neutropenic patient. Arch Intern Med 1996; 156: 1762–1765.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Roberts, P., Gadgil, A., Orendi, J. et al. Infective discitis with Neisseria sicca/subflava in a previously healthy adult. Spinal Cord 41, 590–591 (2003). https://doi.org/10.1038/sj.sc.3101497
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101497
Keywords
This article is cited by
-
Antimicrobial resistance in clinical isolates of Neisseria subflava from the oral cavities of a Japanese population
Journal of Infection and Chemotherapy (2007)