Abstract
Study design: Prospective comparative study.
Objective: To determine whether control of upper limb joint synergy during unrestrained arm raising involving shoulder and elbow flexion is modified by deltoid-to-triceps transfer.
Setting: Rehabilitation unit for spinal cord injury patients, France.
Methods: Five C6 subjects with C5–C6 tetraplegia sustained posterior deltoid-to-triceps transfer and were compared to a control group of 11 subjects. Kinematics of shoulder and elbow joints before, 6 month and 1 year after surgery, during straight-arm raising (SAR) in the plane of the scapula and hand-to-nape-of-neck movements (HNNMs) were explored. Motion was recorded with a six-camera Vicon motion analysis system and the data used to assess the coupling of elbow and shoulder flexion velocities (EFVs and SFVs) and extension velocities.
Results: All subjects were initially assessed at 6.9 months (mean) postsurgery. Three of the upper limbs were assessed a second time (mean 17.9 months). The first assessment showed an increase in shoulder flexion amplitudes in tetraplegic subjects with presurgery shoulder flexion deficits. Peak SFVs and EFVs and extension velocities were slightly modified at the first postsurgery assessment and dramatically improved at the second assessment during both SAR and HNNM. Despite these increased velocities, joint coordination was only partially restored.
Conclusion: A restored elbow active extension improves the speed of elbow flexion. The additional improvement of shoulder motion emphasises the relation between joints in the control of arm movement.
Similar content being viewed by others
Introduction
The surgical restoration of elbow extension in C6 tetraplegic subjects was introduced by Moberg in 1975.1 Several types of tendon transfer can be done. The oldest of these used in tetraplegic subjects, the transfer from the posterior deltoid to the triceps, has been extensively studied.2,3,4,5,6,7 Another method that was initially described for restoring elbow extension in subjects with peripheral paralysis uses the biceps brachii.8 This has been modified to avoid radial paralysis.9,10 Other older techniques initially used to improve elbow extension are no longer used for this purpose, but rather for restoring elbow flexion11,12,13 using the latissimus dorsi14 or for recovering finger opposition in tetraplegic subjects with the brachioradialis.15
While the surgical techniques have been extensively described, most objective evaluations have relied on questionnaires about functions that are not specific to subjects with tetraplegia. Such functional evaluations are also more suitable for a programme of complete surgical restoration of prehension, including the restitution of elbow extension and the opposition of one or more digits16 than for analysing the restoration of elbow extension alone.
Few kinematic studies have been done on the arms of tetraplegic subjects. Most of them have evaluated restricted movements, particularly the kinematics of the elbow,17,18 and shown that the lack of active contraction of the triceps brachii is responsible for the slower elbow flexion velocity and prolonged acceleration and deceleration times. Tetraplegic subjects are also slower at carrying out free pointing movements to targets located in front of them.19 The present study was done to determine whether surgical restoration of shoulder extension of C5–C6 tetraplegic subjects results in faster free arm movements, whether they influence the kinematic parameters of elbow and shoulder articulation, and whether they improve shoulder–elbow coordination.
Materials and methods
Population
This investigation was carried out on five tetraplegic subjects who had suffered traumatic spinal cord injuries, four men and one woman (mean age 27 years SEM 6.0). Both upper limbs of subjects 1 and 3 (S1, S3, Table 1) were operated on. Thus in total seven upper limbs were studied. Posterior deltoid-to-triceps tendon transfers were performed in all the subjects. The interface between the posterior deltoid and the triceps was created according to the Pulvertaft technique with Orthomed R artificial tendon wrapped with aponevrosis in each patient. The elbow was splinted in the extended position for 4 weeks after surgery. Physiotherapy began in the 5th postoperative week with complete removal of the splint at the end of the 6th week. Data on the subjects, time of investigation and their ASIA motor scores assessed at the time of investigation are given in Table 1. The mean time between trauma and surgery was 19.8 months (SEM 4.8). The mean ASIA motor score was 19.2 (SEM 1.3). All subjects could flex their shoulder and elbow against a passive resistance. The preoperative assessment of the upper limb motion was performed 2.1 months (SEM 1.2) before surgery. The first postsurgery assessment was performed when elbow extension was clinically assessed at 3 (on a 1–5 point scale) an average of 6.9 months after surgery (SEM 2.6). A second postsurgery assessment was performed in two subjects (S2 and S3) 17.9 months after surgery (SEM 2.3). The three other subjects were not reassessed because S4 and S5 returned to their homes overseas and S1 died.
We compared our results to those of a reference population of 11 subjects, seven men and four women (mean age 27.4 years SEM 4.6). The ages of the two populations were not significantly different (Student's t-test).
General experimental procedure
All arm motions were assessed using a Vicon 3D motion analysis system. The locations of markers were similar to those used by Schmidt et al.20 Four markers were placed on the arm, three on the forearm and one on the hand. Markers were also placed over the seventh cervical and 10th thoracic vertebrae and the sternum (Figure 1). A static trial was performed first with anatomical markers on the acromion, the elbow (lateral and medial epicondyles) and the wrist (see Figure 1). This trial allowed us to estimate the joint centres and axes relative to the technical frames. The anatomical markers were removed during motion capture, leaving just the technical markers. Angles were calculated from the data obtained during the static trial with the position of each segment (trunk arm, forearm and hand) given by the technical markers. This conformation minimized skin movement during the upper limb movement.20 Shoulder movement was analysed with respect to the trunk, and our marker set did not distinguish between the glenohumeral and the thoraco-scapular joints.21,22
Markers for upper limb movement: arm and forearm bear technical and anatomical markers. The anatomical (lateral and medial epicondyle and wrist) markers are removed after the static trial to minimise skin movement during arm movement. Straight arrows show the axis used to calculate the three basic movements of the shoulder (flexion, abduction and rotation) using Euler's angles
Each control subject sat on a stool; the subjects with tetraplegia sat in a wheelchair. All subjects were asked to perform two movements: (i) a straight-arm lateral and maximal raising and return (SAR) and (ii) a hand-to-nape-of-neck movement (HNNM) and return. The starting and ending positions were the arm along the trunk. Movements were performed at the subject's preferred speed. The first movement revealed the compensatory activity used by each tetraplegic subject to keep the elbow in extension without active extension during maximal shoulder flexion. The second movement was used to evaluate the synergy between the elbow and shoulder.
Angular data calculation
Each angle was expressed as three successive rotations. At the shoulder, the first rotation was flexion with an axis at the intersection of the frontal and coronal planes of the trunk; zero position was when the arm was down along the trunk. The second rotation was abduction with a vertical axis in the sagittal plane of the trunk; zero position was when the arm was in the sagittal plane of the trunk. The third rotation was rotation of the arm about its axis, joining the acromion marker and the centre of the elbow joint; the zero position was when the axis of flexion of the elbow was in the sagittal plane of the trunk. The flexion axis at the elbow was determined with the markers on the lateral and medial epicondyles (see Figure 1 and for a more detailed description see van der Helm and Pronk23).
Statistical analysis
Data are given as means with their standard error (SEM). Since the number of operated upper limbs was small, a nonparametric test (Wilcoxon's ranking signed test) was used to compare the values before and after surgery. The tetraplegic and the control group were compared using Student's t-test or ANOVA.
Results
Straight-arm raising
Figure 2 shows the importance of recovered elbow extension on shoulder kinematics during SAR. This tetraplegic subject (S2) underwent deltoid-to-triceps transfer 2 years after injury, which increased the flexion amplitude two-fold, decreased abduction to the same extent and decreased the peak of external rotation by one-quarter. Table 2 shows the results for the seven operated upper limbs (first assessment). SAR was performed in all the subjects, with a statistically significant decrease in the maximal shoulder abduction (mean 57 SEM 12 before and 14 SEM 6 after surgery), whatever the side operated on. The difference between the shoulder abduction of controls and subjects with tetraplegia before surgery was not statistically significant. Maximal shoulder flexion was severely reduced before surgery in 4/7 subjects (mean 79° SEM 11). Although shoulder flexion increased after deltoid-to-triceps transfer by 42% (mean 113 SEM 11) in these subjects, it remained significantly lower (121 SEM 12) than in the control group (153° SEM 7, P<0.0001). Maximal flexion during SAR did not change significantly if flexion was greater than 120° (3/7) before surgery, that is, it was not greater than 10% of presurgery amplitude. Postsurgery evaluation showed no systematic change in arm rotation.
Shoulder flexion/extension velocities were calculated during the ascending and descending movements and labelled shoulder flexion velocity (SFV).
The mean SFVs were significantly increased in all the subjects (Table 2) during ascent, from 22°/s (SEM 11) to 56°/s (SEM 19), and descent, from 33°/s (SEM 13) to 65°/s (SEM 21). The maximal SFVs during ascent before surgery in tetraplegic subjects (55°/s, SEM 26) were significantly lower than in the control group (234°/s SEM 70, P<0.0001) and remained lower at the first postsurgery evaluation (mean 86°/s SEM 29). The late assessments of three upper limbs showed near normal SFVs of 199°/s (SEM 16). Two of them (S2 right and S3 left) showed increased SFVs of 25 and 22% at the first postsurgery assessment and 85 and 119% at the second. The maximal SFV of the third upper limb (S3 right) increased at the first postsurgery assessment (627%) and to a lesser extent (19%) at the second evaluation (see the table of Figure 3). The time course of the increase of SFV in S3 (left upper limb) is illustrated in Figure 3 before, 10.5 and 21 months after surgery.
SFV during SAR before surgery (a), at the first postoperative assessment (first POA: b, mean 6.9 months) and at the second postoperative assessment (second POA: c, mean 17.9 months) after deltoid-to-triceps transfer in one C5–C6 tetraplegic woman and one control (d). Each curve displays the SFV profile during the ascent and the descending phase of SAR. The table shows the peaks of flexion angular velocity of the shoulder expressed in °/s for S2 and S3 (three upper limbs)
Hand-to-nape-of-neck movement
Table 3 displays the peaks of elbow and shoulder kinematic data before and after surgery and the duration of each phase of the HNNM movement (flexion time or ascent and extension time or descending phase). Elbow flexion/extension velocities were calculated during ascent and during descent and labelled elbow flexion velocities (EFVs). Maximal shoulder flexion, abduction and rotations amplitudes were not significantly different from those of the control group and not significantly modified after surgery. Maximal elbow flexion in tetraplegic subjects before surgery was greater (mean 156° SEM 7) than that of the control group (149° SEM 4) and decreased slightly but significantly (P=0.03) after deltoid-to-triceps transfer (from 156° SEM 7 before to 145° SEM 15). Ascending time of HNNM was decreased (from 3.9 s SEM 1.9 to 2.9 s SEM 0.9), as was descending time (from 3.2 s SEM 1.5 to 2.4 s SEM 1) at the first postsurgery examination; both decreases were statistically significant.
Maximal SFVs were much lower in tetraplegic subjects before surgery (62°/s SEM 22) than those of the control group (201°/s SEM 41). SFV increased in 5/7 upper limbs during the first evaluation after surgery and decreased in two during ascent and descending phase of HNNM (Table 4). The mean increase in maximal SFV during the first assessment was 28% during flexion, 38% during extension. The SFV during flexion of S2 and S3 increased 32% between the pre- and postsurgery assessments and by 128% between the early and late postsurgery assessments. The SFVs were close to normal values (Figure 4) during the late assessment, being 192°/s SEM 21 (normal: 201°/s SEM 41) during ascent and 220°/s SEM 53 (normal: 253°/s SEM 80) during descending phase of HNNM.
Maximal EFVs increased during descending phase after surgery (Table 4 and Figure 5 dashed lines). Before surgery, the mean EFV during descending phase (109°/s SEM 39) was much lower than normal values (mean 241 SEM 29). As for the shoulder, the first postsurgery assessment showed a slight increase in EFV (19%), while the late assessment indicated a near normal EFV (mean 203°/s SEM 19). EFV during ascent increased similarly (Table 4 and Figure 5 straight lines).
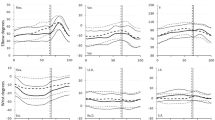
The HNMM of the control group showed a smooth coupling of the elbow and shoulder positions (Figure 6a) during ascent and a more complex coupling of flexion velocities (Figure 6b). The coordination of elbow and shoulder positions was greatly disrupted in tetraplegic subjects, usually with a larger elbow flexion at the beginning of the movement (Figure 6c) and a late shoulder flexion. Although the elbow and shoulder positions remained coupled in subjects with tetraplegia, the coordination of the joint flexion velocities was completely anarchic (Figure 6d). The synergy of elbow and shoulder positions improved slightly at the first assessment after surgery, with a similar absence of coupling between flexion velocities (Figure 7a′ and b′). The coupling of elbow and shoulder positions remained irregular (Figure 7b) and the onset of the movement was sometimes a shoulder flexion that was never observed in the control group (Figure 6a). The late postsurgery assessment showed improved joint coordination during flexion. The coupling of elbow and shoulder positions became more regular and shaped as in the control group (Figure 7c and Figure 6a).
Flexion velocities improved after surgery, but the coordination of flexion velocities varied from subject to subject. Figure 8 shows the strategies of coordination in elbow and shoulder flexion velocities during ascending and descending phases of HNNM for the three upper limbs assessed late as well as for control subjects. S2 dissociated EFVs and SFVs, with an early increase in EFV during the ascending phase and a late decrease in EFV at the end of the movement. The S3 right upper limb had lower joint velocities with a more irregular shape. While the movement of S3 left upper limb seemed to have a normal velocity profile during ascent, the descending phase was more irregular (Figure 7c′).
Discussion
We find that transfer of the posterior deltoid to the triceps in C5–C6 subjects with tetraplegia improves the kinematics of arm movement when executing two free arm movements. When active stabilisation of the elbow is required, as for lateral elevation, the restoration of active muscle contraction allowing elbow extension increases the amplitude of movement and the speed of shoulder flexion in both the ascending and descending phases as soon as the first few months after surgery. While surgery does not change the amplitude of two-joint movements (HNNM) that require flexion of both the shoulder and elbow, it does permit faster shoulder and elbow flexion during the arm raising and lowering phases. The increased flexion speed is much greater during evaluations done over a year after surgery. The joint synergy is also improved during this late evaluation. This varies from one subject to another, and from one limb to another in the same subject.
Most instrumental evaluations of the results of surgery to restore active extension of the elbow in C6 tetraplegic subjects have measured the strength of the transferred muscle, and thus improved elbow extension.2,4,24 Our study of unconstrained arm movements (HNNM) reveals faster elbow extension, indicating the restoration of extension torque, but it also shows a parallel increase in the speeds of elbow flexion and shoulder flexion and extension in movements involving the shoulder (HNNM) and in isolated shoulder movements (SAR). Wierzbicka et al25 showed that contraction of the triceps brachii during pure elbow flexion allows the flexion muscles to produce a larger amplitude flexion plus greater acceleration of the forearm than that obtained without triceps activity. Thus, the triceps controls the time of the movement in rapid movements and is thus a major parameter in controlling the speed of elbow flexion.25 Elbow flexion is slower in C6 tetraplegic subjects who have no triceps brachii contraction, despite the fact that they have no deficit of isometric force in elbow flexion.17 Our results show that the increased speed of elbow extension is directly linked to the restoration of active elbow extension by tendon transfer. But, also with increased elbow flexion speed during unconstrained movements (HNNM), confirming the findings of Wierzbicka et al25 during constrained horizontal single-joint movements.
Brys and Waters26 demonstrated improved joint function depending on the force of an adjacent joint after the restoration of prehension by the transfer of the brachioradialis to the flexor pollici longus in tetraplegic patients. The force of the finger–thumb opposition (pinch) was found to be increased as the elbow extension force increased. There could be several reasons for the great increases in shoulder flexion and extension speeds that we have seen after restoration of elbow extension. It could be because of the loss of biomechanical adaptation of the shoulder to compensate for the deficient elbow extension, to an increase in shoulder flexion force resulting from increased shoulder extension torque, or to increased shoulder flexion linked to increased elbow extension torque.
Tetraplegic subjects identical to those we have studied raised themselves by movements involving flexion and adduction of the shoulder to compensate for their lack of elbow extension.27,28 Part of the overall upper limb movement, which is done by the elbow extensors in the control group, can thus be compensated for in our tetraplegic subjects by a change in shoulder kinetics or kinematics. The restricted speed of shoulder flexion during SAR before surgery may thus be partly because of the compensation that the shoulder must develop to allow passive elbow extension when there is no active contraction of the triceps brachii. The restoration of triceps function also allows the shoulder to fully use its kinetic capacity and to develop normal flexion speeds during both concentric (elevation phase) and eccentric movements (descending phase). The faster shoulder flexion that we have observed following surgery may also be linked to improved shoulder extension torque, although the isometric power of a muscle falls after the transfer of one of its insertions.1,29 The torque of the posterior deltoid might increase after surgery because the insertion is moved 25 cm towards the end of the humerus by the addition of a graft. The same mechanism as in elbow flexion17 may well explain the faster shoulder flexion. Our protocol does not allow us to differentiate between these various mechanisms; thus further studies are needed.
While we have demonstrated an increase in flexion speed after surgery, we have not found any synergy between the shoulder and elbow joints comparable to that seen in the control group, even after some considerable time postsurgery. This problem of speed coordination could be because of the lack of any change in proprioceptor deficit from the medullary damage. The control of free arm movements depends on proprioceptor activity.30 Thus, although the proprioceptive control of areas below the lesion is unchanged in our subjects, the proprioceptive information generated by an elbow movement is inevitably reinforced by the tendon transfer.
It has been shown that the posterior deltoid has anatomical features that make it ideal for restoring elbow extension in C5–C6 tetraplegic subjects,7 but the quality of the results of tendon transfer seem to depend on several factors. The mechanical behaviour of the transfer is not the same as that of a normal triceps: the isometric coupling peak is much weaker and occurs at 130° of flexion instead of at 110° as in the normal triceps.4 Isokinetic evaluation of the elbow extension also shows a great reduction in the maximum torque in tetraplegic subjects after transfer of the posterior deltoid, but also shows that the acceleration and deceleration phases are four to five times slower.24 The chronic decrease in elbow extension torque after muscle transfer may be partly responsible for the lack of uniform control of joint coordination that we find, or the development of a compensatory strategy, as in our patient S2.
The variation in extension torque is also much greater in tetraplegic subjects after tendon transfer than in the control group.4 The placing of the transferred tendon under tension during surgery directly influences the quality of outcome.2,31 The gradual postsurgery elongation of each tendon varies greatly from one individual to another (23.1±5.8 mm),32 which can explain the variability of joint coordination from one upper limb to another of the same tetraplegic.
There have been few instrumental evaluations of the benefit of surgery on the upper limbs of tetraplegic subjects,16,24,33 although many studies have demonstrated the functional benefit of such surgery.2,3,12,24,34,35,36,37 Functional scales are usually used to determine the improvement in elbow function following surgery for tendon transfer.2,5,9,37,38 A recent study by Dunkerley et al37 found no significant difference between the activities of independent daily living and the use of a manual wheelchair in two groups of tetraplegic subjects with injuries at the same level; one group underwent transfer of the posterior deltoid to the triceps while the other did not. These two groups were evaluated for their performance, measured with the functional independance measure (FIM) and their wheelchair performance over 10 m and in controlling the wheelchair. The authors suggest that the FIM may not be sensitive enough to assess this type of therapy, and that it might be necessary to develop more sensitive scales.19 Three-dimensional analysis of movement seems to be a powerful tool that could satisfy certain requirements for testing the quality of functional results of tendon transfer surgery in tetraplegic subjects.
Conclusion
Stabilisation of the elbow by transfer of the posterior deltoid to the triceps provides early increases in the joint amplitude during free movements of the upper limb in C6 tetraplegic subjects. The peaks of shoulder and elbow flexion speed are almost normal, indicating the importance of restoring elbow extension torque for improving the whole kinematic picture of the upper limb in these subjects. It also emphasises the influence of the kinetic behaviour of a joint on the kinematics of an adjacent joint. But, despite this great improvement in upper limb kinematics, the synergy between the shoulder and elbow joints is not completely restored.
References
Moberg E . Surgical treatment for absent single-hand grip and elbow extension in quadriplegia. Principles and preliminary experience. J Bone Joint Surg Am 1975; 57: 196–206.
Lacey SH, Wilber RG, Peckham PH, Freehafer AA . The posterior deltoid to triceps transfer: a clinical and biomechanical assessment. J Hand Surg [Am] 1986; 11: 542–547.
Mennen U, Boonzaier AC . An improved technique of posterior deltoid to triceps transfer in tetraplegia. J Hand Surg [Br] 1991; 16: 197–201.
Rabischong E, Benoit P, Benichou M, Allieu Y . Length–tension relationship of the posterior deltoid to triceps transfer in C6 tetraplegic patients. Paraplegia 1993; 31: 33–39.
Raczka R, Braun R, Waters RL . Posterior deltoid-to-triceps transfer in quadriplegia. Clin Orthop 1984; 11: 163–167.
Allieu Y et al. Réanimation de l'extension du coude chez le tétraplégique par transplation du deltoïde postérieur. Rev Chir Orthop 1985; 71: 195–200.
Friden J, Lieber RL . Quantitative evaluation of the posterior deltoid to triceps tendon transfer based on muscle architectural properties. J Hand Surg [Am] 2001; 26: 147–155.
Friedenberg ZB . Transposition of the biceps brachii for triceps weakness. J Bone Joint Surg 1954; 36: 356–358.
Kuz JE, Van Heest AE, House JH . Biceps-to-triceps transfer in tetraplegic patients: report of the medial routing technique and follow-up of three cases. J Hand Surg [Am] 1999; 24: 161–172.
Revol M, Briand E, Servant JM . Biceps-to-triceps transfer in tetraplegia. The medial route. J Hand Surg [Br] 1999; 24: 235–237.
Betz RR et al. Bipolar latissimus dorsi transposition and functional neuromuscular stimulation to restore elbow flexion in an individual with C4 quadriplegia and C5 denervation. J Am Paraplegia Soc 1992; 15: 202–228.
Johnstone BR et al. Surgical rehabilitation of the upper limb in quadriplegia. Aust N Z J Surg 1987; 57: 917–926.
Stern PJ, Caudle RJ . Tendon transfers for elbow flexion. Hand Clin 1998; 4: 297–307.
Harman PH . Muscle transplantation for triceps palsy. The technique of utilizing the latissimus dorsi. J Bone Joint Surg 1949; 31: 409–412.
Ober FR, Barr JS . Brachioradialis muscle transposition for triceps weakness. Surg Gynecol Obstet 1938; 67: 105.
van der Linde H et al. Kinematic assessment of manual skill following functional hand surgery in tetraplegia. J Hand Surg [Am] 2000; 25: 1140–1146.
Wierzbicka MM, Wiegner AW . Effects of weak antagonist on fast elbow flexion movements in man. Exp Brain Res 1992; 91: 509–519.
Wierzbicka MM, Wiegner AW . Accuracy of motor responses in subjects with and without control of antagonist muscle. J Neurophysiol 1996; 75: 2533–2541.
Laffont I et al. Kinematics of prehension and pointing movements in C6 quadriplegic patients. Spinal Cord 2000; 38: 354–362.
Schmidt R, Disselhorst-Klug C, Silny J, Rau G . A marker-based measurement procedure for unconstrained wrist and elbow motions. J Biomech 1999; 32: 615–621.
Prokopenko RA, Frolov AA, Biryukova EV, Roby-Brami A . Assessment of the accuracy of a human arm model with seven degrees of freedom. J Biomech 2001; 34: 177–185.
Kelkar R et al. Glenohumeral mechanics: a study of articular geometry, contact, and kinematics. J Shoulder Elbow Surg 2001; 10: 73–84.
van der Helm FC, Pronk GM . Three-dimensional recording and description of motions of the shoulder mechanism. J Biomech Eng 1995; 117: 27–40.
Bottero L et al. [Isokinetic dynamometric evaluation of rehabilitation results of elbow extension in tetraplegic patients]. Ann Chir Plast Esthet 2000; 45: 419–424.
Wierzbicka MM, Wiegner AW, Shahani BT . Role of agonist and antagonist muscles in fast arm movements in man. Exp Brain Res 1986; 63: 331–340.
Brys D, Waters RL . Effect of triceps function on the brachioradialis transfer in quadriplegia. J Hand Surg [Am] 1987; 12: 237–239.
Harvey LA, Crosbie J . Weight bearing through flexed upper limbs in quadriplegics with paralyzed triceps brachii muscles. Spinal Cord 1999; 37: 780–785.
Harvey LA, Crosbie J . Biomechanical analysis of a weight-relief maneuver in C5 and C6 quadriplegia. Arch Phys Med Rehabil 2000; 81: 500–505.
Freehafer AA . Tendon transfers in patients with cervical spinal cord injury. J Hand Surg [Am] 1991; 16: 804–809.
Verschueren SM, Swinnen SP, Cordo PJ, Dounskaia NV . Proprioceptive control of multijoint movement: unimanual circle drawing. Exp Brain Res 1999; 127: 171–181.
Freehafer AA, Peckham PH, Keith MW . Determination of muscle–tendon unit properties during tendon transfer. J Hand Surg [Am] 1979; 4: 331–339.
Friden J, Ejeskar A, Dahlgren A, Lieber RL . Protection of the deltoid to triceps tendon transfer repair sites. J Hand Surg [Am] 2000; 25: 144–149.
Kirsch RF, Acosta AM, Perreault EJ, Keith MW . Measurement of isometric elbow and shoulder moments: position-dependent strength of posterior deltoid-to-triceps muscle tendon transfer in tetraplegia. IEEE Trans Rehabil Eng 1996; 4: 403–409.
Freehafer AA, Kelly CM, Peckham PH . Tendon transfer for the restoration of upper limb function after a cervical spinal cord injury. J Hand Surg [Am] 1984; 9: 887–893.
Freehafer AA . Gaining independence in tetraplegia. Cleveland technique. Clin Orthop 1998; 282–289.
Mohammed KD et al. Upper-limb surgery for tetraplegia. J Bone Joint Surg Br 1992; 74: 873–879.
Dunkerley AL, Ashburn A, Stack EL . Deltoid triceps transfer and functional independence of people with tetraplegia. Spinal Cord 2000; 38: 435–441.
Paul SD et al. Single-stage reconstruction of key pinch and extension of the elbow in tetraplegic patients. J Bone Joint Surg Am 1994; 76: 1451–1456.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Remy-Neris, O., Milcamps, J., Chikhi-Keromest, R. et al. Improved kinematics of unrestrained arm raising in C5–C6 tetraplegic subjects after deltoid-to-triceps transfer. Spinal Cord 41, 435–445 (2003). https://doi.org/10.1038/sj.sc.3101481
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101481
Keywords
This article is cited by
-
Upper limb kinematics after cervical spinal cord injury: a review
Journal of NeuroEngineering and Rehabilitation (2015)
-
Analysis of tetraplegic reaching in their 3D workspace following posterior deltoid-triceps tendon transfer
Spinal Cord (2010)
-
Sensory-motor equivalence: manual aiming in C6 tetraplegics following musculotendinous transfer surgery at the elbow
Experimental Brain Research (2010)
-
Decision for reconstructive interventions of the upper limb in individuals with tetraplegia: the effect of treatment characteristics
Spinal Cord (2008)
-
How do C6/C7 tetraplegic patients grasp balls of different sizes and weights? Impact of surgical musculo-tendinous transfers
Spinal Cord (2007)