Abstract
Study design: A case report of spontaneous resolution of a lumbar postdiscectomy pseudomeningocoele.
Objectives: To suggest the role of nonoperative treatment even in symptomatic pseudomeningocoeles.
Setting: Withybush General Hospital, Haverfordwest, Pembrokeshire, South Wales, UK.
Case report: A 65-year-old lady underwent L4/L5 discectomy for lumbar disc prolapse in 1998. As the patient did not have relief of symptoms, an MRI was taken at 1 month following the operation, which showed a residual disc at L4/L5 and a pseudomeningocoele communicating with the subarachnoid space. The patient could not undergo further treatment because of the untimely demise of the surgeon. Over the next 3 months, the symptoms began to improve and the patient was totally asymptomatic and remained so for 3 years. In 2001, she was seen for a recurring leg pain and back pain and an MRI was done, which showed complete disappearance of the pseudomeningocoele but with recurrent disc lesion.
Conclusion: Although the current medical literature favours re-exploration and repair of the dural defect in symptomatic pseudomeningocoele, the authors are of the opinion that conservative treatment may have a role in the treatment of the above condition as illustrated by the above example.
Similar content being viewed by others
Introduction
Pseudomeningocoele is a complication of lumbar discectomy. It was first reported in the literature in 1946 following laminectomy for removal of neoplasm.1 The definitive treatment of a symptomatic pseudomeningocoele is surgical.2,3,4,5 We present the case report of a patient who had complete resolution of the lesion and symptomatic relief without any form of surgical intervention.
Case report
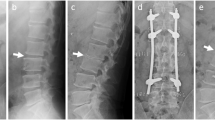
A 65-year-old lady underwent L4/L5 discectomy in 1998 for prolapsed intervertebral disc. The patient did not get symptomatic relief following the operation. An MRI was done 1 month following the operation to find out the cause of the persisting pain and it showed a pseudomeningocoele communicating with the subarachnoid space (Figure 1). Unfortunately, the surgeon treating the patient expired untimely, which prompted the patient to continue symptomatic treatment with painkillers. It was also compounded by the fact that the local hospital did not have another spine surgeon. But, the patient's symptoms improved and had total pain relief for the next 3 years. In 2001, the patient had recurrence of leg pain and the MRI showed that the pseudomeningocoele had completely disappeared (Figure 2) and the patient had recurrent disc disease.
Discussion
Pseudomeningocoeles are defined as extradural collections of cerebrospinal fluid that extravasate through a dural or arachnoid tear.6,7,8 The first three cases of pseudomeningocoeles following a lumbar discectomy were reported by Swanson and Fincher9 in 1947. The incidence of pseudomeningocoeles after lumbar discectomy varies from 0.19 to 2%.8,10
It is postulated that a smaller dural tear would be more prone to develop into an encysted pseudomeningocoele than a wider one. If the arachnoid remains intact there may be herniation of the arachnoid through the dural tear opening resulting in an arachnoid lined cyst.3,11 A narrow dural opening acts like a one-way valve leading to increase in the size of the CSF collection and formation of a pseudomembrane and occasionally it gets encapsulated by fibrous tissue.5,12 Weakness of the paraspinal muscles following surgery causes the pseudomeningocoele to expand.3 This may explain why a persistent CSF fistula after lumbar puncture does not cause pseudomeningocoele formation.4,6,8,12,13 Nerve roots may herniate into the dural opening and form a physical barrier to the healing of the dura.2
Patients with postoperative pseudomeningocoeles present with recurrence of symptoms months or years after the initial surgery.2,3,5,14 Sometimes a mild bulge under the operation scar may be the only clinical finding.3,5 Radicular pain may be because of herniation of nerve roots into the pseudomeningocoele or adhesions of nerve roots to the edges of the sac.13,15 Focal neurological deficits also can occur although uncommon.15 In patients with large pseudomeningocoele, headache may be a symptom.6
Intrathecal contrast-enhanced CT scan has the ability to identify the neck of the pseudomeningocoele.8,10,15 The MRI is more effective for demonstrating the presence of a communication between the pseudomeningocoele and the subarachnoid space without intrathecal contrast material.14
Very rarely the pseudomeningocoele may undergo ossification and give rise to a mass compressing the exposed dura.16 The resolution of pseudomeningocoele has been reported after repeated aspirations or with the use of fibrin patches.6 However, most of the authors are of the opinion that symptomatic pseudomeningocoeles should be treated by surgical repair.2,3,5,6,14,15
Conclusion
Pseudomeningocoeles are an uncommon complication of lumbar disc surgery. Recurrence of back and leg symptoms following operation should alert the surgeon of this rare complication apart from recurrence of the disc. Nonoperative management may have a role even in the treatment of symptomatic lumbar pseudomeningocoeles as illustrated in the above example. Patients need to be kept under regular review to watch for neurological complications.
References
Hyndman OR, Gerber WF . Spinal extradural cysts, congenital and acquired. Report of cases. J Neurosurg 1946; 3: 474–486.
Stuart Lee K, Hardy IM . Postlaminectomy lumbar pseudomeningocoele, Report of 4 cases. Neurosurgery 1992; 30: 111–114.
Rinaldi I, Peach WF . Postoperative lumbar pseudomeningocoele Report of 2 cases. J Neurosurg 1969; 30: 504–506.
Miller PR, Elder Jr FW . Meningeal pseudocysts (meningocele spurious) following laminectomy. Report of ten cases. J Bone Joint Surg (Am) 1968; 50A: 268–276.
Bhatoe HS . Postoperative lumbar pseudomeningocoele. J Indian Med Assoc 1995; 93: 280–282.
Barron HS . Lumbar pseudomeningocoele. Orthopaedics 1990; 13: 603, 608–610.
Pau A . Postoperative menigocoele spurius. Report of two cases. J Neurosurg Sci 1974; 18: 150–152.
Teplick JG et al. CT identification of postlaminectomy pseudomeningocoele. Am J Roentg 1993; 140: 1203–1206.
Swanson HS, Fincher EF . Extradural arachnoidal cysts of traumatic origin. J Neurosurg 1947; 4: 530–538.
Schumacher HW, Wassman H, Podlinski C . Pseudomeningocoele of the lumbar spine. Surg Neurol 1988; 29: 77–78.
Rinaldi I, Hodges TO . Iatrogenic lumbar meningocoele. Report of three cases. J Neurol Neurosurg Psychiatry 1970; 33: 484–492.
Pagni CA, Cassinari V, Bernasconi V . Meningocoele spurious following hemilaminectomy in a case of lumbar disc hernia. J Neurosurg 1961; 18: 709–10.
Mohan Kar A, Pradhan S, Mittal P . Cerebrospinal fluid fistula after lumbar puncture. BMJ 1987 Aug 29; 295: 528.
Murayama S, Numaguchi Y, Whitecloud ST . Magnetic resonance imaging of postsurgical pseudomeningocoele. Computerised Med Imaging Graphics 1989; 13: 335–339.
Hadani M et al. Entrapped lumbar nerve root in a pseudomeningocoele after laminectomy. Report of three cases. Neurosurgery 1986; 3: 474–486.
Ishaque MA, Crockard HA, Stevens JM . Ossified pseudomeningocoele following laminectomy. Case reports and review of the literature. Eur Spine J 1997; 6: 430–432.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kumar, A., Nambiar, C. & Kanse, P. Spontaneous resolution of lumbar pseudomeningocoele. Spinal Cord 41, 470–472 (2003). https://doi.org/10.1038/sj.sc.3101462
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101462