Abstract
Study design: Retrospective study.
Objectives: To examine the value of operative fracture stabilization by means of the ring fixator in fractures of the lower extremity in the presence of chronic paralysis caused by transverse lesions of the spinal cord.
Setting: A specialist center for the treatment of spinal cord injuries in Germany.
Methods: Clinical examination of the lower extremities with side-for-side comparison, radiological investigation of the fractures, patient survey.
Patients: In 21 patients with chronic spinal cord lesions, 22 fractures of the lower extremities were treated with the ring fixator.
Results: At follow-up a mean of 41.5 months after fracture healing it could be shown that movement in the knee and ankle joints on the same side as the fracture was not restricted by more than 10° in any of our patients. No losses affecting activities of daily living were reported, and 19 of the 21 patients were satisfied with the result achieved with this technique. After four of the 22 operations there were complications. Malalignments were visible radiologically following five of the fractures.
Conclusions: In osteoporosis-induced fractures of the lower extremities in chronically paraplegic and tetraplegic patients, fracture stabilization with the ring fixator, with fewer complications and better results in terms of joint mobility, is superior to the conservative treatment so far given preference in the literature. It should be offered as an alternative to conservative treatment in the case of pathological fractures.
Similar content being viewed by others
Introduction
Once paralysis has occurred as the result of a transverse lesion of the spinal cord, the bone substance in the lower extremities begins to deteriorate, leading to a lasting reduction of the bone density in these limbs.1,2,3 It is impossible to say with any degree of certainty to what extent this is responsible for fractures in paraplegic and tetraplegic patients; the incidence given in the literature varies between 1.45% and 8.7%.4,5,6,7,8 Nor is there any consensus on the best therapy for fractures of the lower extremities in paraplegic and tetraplegic patients. For the treatment of fractures of the extremities in connection with acute spinal trauma internal fixation is preferred.9,10,11,12,13 In fractures of the lower extremities in chronic paraplegia or tetraplegia, however, conservative treatment is recommended.5,8,11,14 The complication rate attributed to surgical therapy is too high. Defective alignment of the axis and leg shortening are accepted as unavoidable.6,8,14 Even conservative treatment is not free of complications, however: complication rates of 19% and 42% have been reported.11,15 The treatment selected for fractures of the lower extremities in the presence of chronic damage to the spinal cord should achieve secure primary stability and exclude the unnecessary risks inherent in open fracture treatment when the bone is affected by osteoporosis. Ilizarov's ring fixation method embodies these advantages.16 The authors' own results are presented to allow an evaluation of the minimally invasive method of fracture treatment with a ring fixator for fractures of the lower extremities sustained after years of paralysis caused by a transverse spinal lesion.
Patients and methods
From August 1993 to June 2000, the ring fixator was used in the Spinal Cord Center of the Werner Wicker Clinic in Bad Wildungen in the treatment of 22 fractures of the lower extremities in 21 patients (7 female, 14 male) with chronic spinal cord lesions (9 tetraplegic, 12 paraplegic patients). Lesions of the motor and sensory pathways were complete in 19 patients; in one woman patient with tetraplegia and one with paraplegia the lesions were incomplete, but both were nonetheless unable to use their limbs in a functional way. Only one patient had flaccid paralysis. Various degrees of spasticity were present in 19 patients. The mean age of these patients was 47.4 (range 27–73) years. The fractures were sustained when the patients had been paralyzed for a mean of 14.7 (2–44) years. In 19 patients the paralysis had resulted from an accident, in one female patient from hypoxemic damage, and in one other female patient from instability of the cervical spine caused by chronic polyarthritis. In 20 cases the patients had sustained the fractures during transfer maneuvers, falls from their wheelchairs, or physiotherapy. It was not always possible to say precisely what had precipitated the fractures. In one case the patient's fracture was the result of an automobile accident. The fractures made themselves obvious in pathologic mobility and sounds, swellings, slightly raised body temperature, and increased spasticity. The mean latent period between roentgenological confirmation of the fracture and operation was 10.8 (1–43) days in 16 patients; only in six patients was surgery performed on the day of the event triggering the fracture. Treatment was given for three fractures of the distal femur, four of the proximal tibia, five diaphyseal fractures of the tibia, and 10 distal fractures of the tibia (Table 1). The fractures were classified according to the AO/ASIF system.17 Two distal fractures of the lower leg were present in one patient; a distal fracture of the femur and a distal fracture of the tibia in the same leg in one patient; and proximal fractures of the tibia in both legs in one patient (Table 2).
The Wiesbaden ring fixator18 was used for internal fixation. This differs from the Ilizarov fixator in that the ring systems are made of a synthetic radiolucent material and the connecting pieces between the rings are linked in by ball-and-socket joints, allowing adjustment in three dimensions. To ensure that the operation would not be disturbed by spastic movements, all the patients were operated on under a general anesthetic.
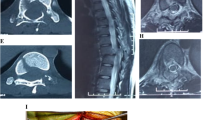
The patients were able to become mobile immediately after the operation as the system is stable on exercise and weight-bearing (Figures 1 and 2). The physiotherapy regimen included weight-bearing in a standing position and daily exercises for conservation of the adjacent joints. Positioning techniques for prevention of decubitus ulcers and the principles followed for bowel and bladder evacuation complied with the requirements imposed by the spinal paralysis as understood in a center for the treatment of spinal cord-injured patients. Special attention is paid to padding the fixator rings with pillows and foam pads while the patient is confined to bed.
Same patient as in Figure 1, 5 days after surgery, with weight-bearing on the right, fractured leg
After bony union had been confirmed by a roentgenological check the ring fixator was removed.
The clinical follow-up examinations, radiological controls, and patient surveys were carried out during outpatient examinations to check on the fractures, or during hospital stays for other treatments not connected with the fracture. In two cases the findings were ascertained in another center for spinal cord-injured patients, where the patients were not, however, being treated for problems connected with the fracture.
Results
The ring fixator needed to be left in situ for a mean of 68.3 (range 38–138) days before bony healing was confirmed (Figure 3a–c). The duration of stay in hospital was a mean of 76.4 (1–158) days. The clinical follow-up examination was a mean of 41.5 (1–91) months after removal of the ring fixator.
The mobility of the knee joints after fractures close to the knee (patients 1–7) revealed definite restrictions in the knee joints of one patient (no. 6) following proximal fractures of the tibia in both legs (Table 2). In the other cases the knee joint movement was equally good on both sides.
In two patients (patients 8 and 17) restricted mobility of the ankles was seen: comparison of both legs revealed an extension deficit of 10° following fractures of the tibial shaft and the distal tibia. One patient (no. 10) had pre-existing arthrodesis necessitated by rheumatoid arthritis.
At the last radiological check, performed on average 27.0 months (range 1–91 months) after removal of the ring fixator, all fractures were stably united. Only in five patients was malalignment observed (Table 3). Neither the shortening of the thigh by 1 cm in one patient, nor the valgus, varus or recurvation malpositioning of the tibial shaft and the distal tibia was found at the clinical follow-up examination to be causing problems with the sitting position, positioning of the foot or feet in the wheelchair or any difficulties with the footwear.
None of the patients reported any loss of function affecting activities of daily living that could be connected with the fractures. Nineteen of the 21 patients said they would consent to the procedure with the ring fixator again in the event of a new fracture.
Complications
The following complications occurred: in one patient there was still no roentgenologically demonstrable callus formation after 56 days. This patient weighed 130 kg. The ring fixator was removed and an AO fixator was substituted for it; fracture healing was then confirmed radiologically after 114 days. In one patient the fixator had to be repositioned because the system was not stable. In each of two patients a wire was repositioned because of a soft tissue defect.
There were no incidences of thrombosis or decubitus ulcers connected with stabilization of the fractures.
Discussion and conclusion
Although the study presented in this paper involved only a limited number of subjects, when the overall picture is considered a comparison with reports published on the treatment of fractures of the lower extremities hitherto does reveal that it has some special features.4,5,6,7,8,9,10,11,12,13,14 When the 22 fractures treated in the course of this study are classified according to the system of McMaster and Stauffer,11 21 are found to belong in group II (pathologic features caused by low-energy trauma). In such fractures it has hitherto been standard procedure to apply conservative methods with soft pillows and soft casts. Cochran et al. are the only authors who have published any detailed information on the extent of clinical movement.15 While the complication rate of the operations in the present study is not low, with four out of 22, it was possible to achieve a stable situation as far as the bones were concerned, with practically free movement of the joints. Only Cochran et al.15 have described restricted joint movement in the patients treated with conservative methods, 13 of their 55 patients having less than 90° knee flexion. Several authors have described decubitus ulcers as a result of treatment with casts and splints;4,6,11,15 these were not observed in our study.
In four patients in our study, defective bone positions were seen radiologically; radiological results are not mentioned in any of the other study reports. In addition, the acceptance of limb shortening and defective position following conservative treatment described by some authors6,8,14 has not so far been questioned in the sense of asking the patients affected whether they are also content to accept them. Our patients' satisfaction with the ring fixator seems to be high. The long duration of inpatient treatment, with a mean of 76 days, is comparable to the duration of treatment reported by Cochran. Other authors have not given any details on length of treatment.
The minimally invasive method of ring fixation for the operative treatment of pathologic features of the lower extremities in patients affected by chronic spinal cord lesions is characterized in the overwhelming majority of cases by reliable remodeling, practically free movement of the joints, a relatively low complication rate, and a high level of acceptance among the patients. It should therefore be mentioned as an alternative to conservative treatment of pathologic fractures of the lower extremities in the presence of chronic paralysis resulting from transverse lesions of the spinal cord. Certainty about the advantages and disadvantages of the conservative treatment, the ring fixation method, and other techniques of internal fixation can only be achieved in a prospective study with accurate classification of the fracture site, duration of paralysis before the fracture, and causation of the fracture for each patient.
References
Roberts D et al. Longitudinal study of bone turnover after acute spinal cord injury. J Clin Endocrinol Metab 1998; 83: 415–422.
Szollar S et al. Bone mineral density and indexes of bone metabolism in spinal cord injury. Am J Phys Med Rehabil 1998; 77: 28–35.
Garland D et al. Regional osteoporosis in women who have a complete spinal cord injury. J Bone Joint Surg [A] 2001; 83: 1195–1200.
Eichenholz S . Management of long-bone fractures in paraplegic patients. J Bone Joint Surg [A] 1963; 45: 299–310.
Freehafer A & Mast W . Lower extremity fractures in patients with spinal cord injury. J Bone Joint Surg [A] 1965; 47: 683–694.
Ragnarsson K . Lower extremity fractures after spinal cord injury: a retrospective study. Arch Phys Med Rehabil 1981; 62: 418–423.
Nottage W . A review of long-bone fractures in patients with spinal cord injuries. Clin Orthop 1981; 155: 65–70.
Ingram R, Suman R & Freeman P . Lower limb fractures in the chronic spinal cord injured patient. Paraplegia 1989; 27: 133–139.
Meinecke F, Rehn J & Leitz G Conservative and operative treatment of fractures of the limbs in paraplegia, Proceedings of the Annual Spinal Cord Injury Conference 1967; 17: 77–91.
Tricot A & Hallot R . Traumatic paraplegia and associated fractures. Paraplegia 1968; 5: 211–220.
McMaster W & Stauffer E . The management of long bone fractures in the spinal cord injured patient. Clin Orthop 1975; 112: 44–52.
Garland D, Saucedo T & Reiger T . The management of tibial fractures in acute spinal cord injury patients. Clin Orthop 1986; 213: 237–240.
Baird R, Kreitenberg A & Eltorai J . External fixation of femoral shaft fractures in spinal cord injury patients. Paraplegia 1986; 24: 183–190.
Freehafer A . Limb fractures in patients with spinal cord injury. Arch Phys Med Rehabil 1995; 76: 823–827.
Cochran T, Bayley J & Smith M . Lower extremity fractures in paraplegics: pattern treatment, and functional results. J Spinal Disord 1988; 3: 219–223.
Ilizarov G Transosseous Osteosynthesis: Theoretical and Clinical Aspects of the Regeneration and Growth of Tissue, Berlin, Heidelberg, New York: Springer, 1991.
Müller M, Allgöwer M, Schneider R & Willenegger H Manual of Internal Fixation, 3rd ednBerlin, Heidelberg, New York: Springer, 1991.
Fischer J, Dufek P & Stachel P . Limb lengthening with epiphyseal and callus distraction using the Wiesbaden ring fixator. Orthopäde 1992; 3: 210–220.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Meiners, T., Keil, M., Flieger, R. et al. Use of the ring fixator in the treatment of fractures of the lower extremity in long-term paraplegic and tetraplegic patients. Spinal Cord 41, 172–177 (2003). https://doi.org/10.1038/sj.sc.3101397
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101397
Keywords
This article is cited by
-
Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury
Spinal Cord (2015)
-
Soft-plastic brace for lower limb fractures in patients with spinal cord injury
Spinal Cord (2014)
-
Response to Soft-plastic brace for lower limb fractures in patients with spinal cord injury
Spinal Cord (2014)
-
Elastisch–stabile intramedulläre Nagelung einer Unterschenkelfraktur bei chronischer Querschnittslähmung
Der Orthopäde (2009)
-
Operative Therapie von Frakturen der unteren Extremit�ten bei chronischen Querschnittl�hmungen
Der Orthop�de (2005)