Abstract
Study design: A case report of self-injurious behavior in four children and adolescents with spinal cord injuries (SCI).
Objectives: To report a relatively unusual complication of pediatric-onset SCI, focusing on the potential role that dysesthesia may play in self-injurious behavior.
Setting: A Spinal Cord Injury Program in a Children's Hospital in Chicago that serves children from midwestern and south-central United States of America.
Method: Case reports and literature review.
Results: Case reports are presented of four children or adolescents with SCI who exhibited self-injurious behavior. Two of the subjects had symptoms consistent with dysesthesia. The self-injurious behavior in these two subjects and a very young child responded to treatment with anticonvulsants. The self-injurious behavior in the fourth patient was probably the result of poor technique of using his mouth to move his hands, which responded to conservative management including education, occupational therapy and gloves.
Conclusion: Self-injurious behavior is a relatively unusual complication of pediatric onset SCI, and may be a manifestation of dysesthesia and be responsive to treatment with anticonvulsants.
Similar content being viewed by others
Main
Self-injurious behavior is most commonly observed in children with severe or profound developmental delay.1 However, self-injurious behavior has been described in individuals with mild developmental delays as well as in those with normal cognition, including three adults with spinal cord injuries (SCI).2,3 Self-biting with multiple finger amputations was reported in two adult males with complete C4 SCI2 and in another adult male with a C5-6 injury.3 In addition, there are two published reports of self-injurious behavior in individuals with meningomyelocele.4,5 However, self-injurious behavior in children or adolescents with SCI has not been reported. Of the nearly 500 children and adolescents with SCI who have received care at the Chicago Shriners Hospitals for Children during the past 20 years, four patients exhibited self-injurious behaviour. These cases are presented in order to increase the awareness of this complication and the potential efficacy of medications such as carbamazepine and gabapentin.
Case Reports
Case 1 is a male who sustained a complete left C7, right T1 SCI at 2 years of age as a result of a motor vehicle crash. At 6 years of age, he was noted to be pinching and picking at both of his nipples, resulting in scarring and obliteration of the areolas and nipples bilaterally. He stated that he picked at his nipples because they irritated him. At 7 years of age, carbamazepine (10 mg/kg/day) was initiated, resulting in a carbamazepine blood level of 11 mcg/ml. Subsequently, there was a significant improvement in the self-injurious behavior. The carbamazepine was stopped when he was 10 years old, but was restarted when he was 12 years of age because of recurrent self-injurious behavior. When he was last seen at 14 years of age, he had experienced several relapses of self-mutilation whenever he stopped taking his carbamazepine.
Case 2 is a male with a complete C5 SCI, which was noted at birth. At 11 months of age he began biting the dorsum of both of his hands and both thumbnails, despite the use of gloves. From 3 to 5 years of age, this self-injurious behavior resolved when protective padding such as gauze was used. At 5 years of age, the self-injurious behavior recurred, but resolved after initiating carbamazepine (10 mg/kg/day), which resulted in a carbamazepine blood level of 4 mcg/ml. Approximately 9 months later the self-injurious behavior reappeared when the carbamazepine was discontinued, but quickly resolved when carbamazepine was restarted. During a hospitalization for pneumonia, the self-injurious behavior recurred but responded to an increase in the dosage of the carbamazepine (15 mg/kg/day). At 8 years of age, carbamazepine was discontinued and gabapentin (15 mg/kg/day, blood level=3.2 mcg/ml) was initiated with continued resolution of symptoms at last follow-up when he was 9 years of age.
Case 3 is a female who sustained a left C8, right T1 SCI as a result of transverse myelitis when she was 9 years of age. When we first saw her at 13 years of age, she was noted to have biting injuries to both arms and several fingers. The distal aspects of the right ring and little fingers and left little finger were the most involved areas with ablation of the nail beds. She attributed this behavior to anxiety and unpleasant tingling sensation in the involved areas. Counseling was initiated and the behavior improved. However, at 14 years of age, the self-injurious behavior recurred, so that counseling was resumed and carbamazepine (100 mg three times a day) was initiated. Over the ensuing 3½ years, she had relapses of the self-injurious behavior whenever she would stop taking the carbamazepine. However, on three occasions during this period of time when she claimed that she was taking her carbamazepine, carbamazepine blood levels were <2 mcg/ml. At 17½ years of age, carbamazepine was discontinued and gabapentin (300 mg three times a day) was initiated. At last follow-up 2 months later, the self-injurious behavior had resolved.
Case 4 is a male who sustained a complete C5 SCI as a result of a fall when he was 16 years old. When first seen by us at age 17 years, he had bilateral hand and terminal digit wounds from biting. He stated that he was biting his hands to help move his arms. A combination of education, occupational therapy, and use of gloves resulted in resolution of the self-injurious behavior within a year. At 20 years of age when he was last seen, the self-injurious behavior had not recurred.
Discussion
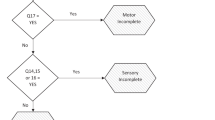
The association of self-injurious behavior with dysesthesia was based on two of our patients exhibiting symptoms consistent with dysesthesia and the location of the self-mutilation involving dermatomes immediately caudal to intact segments.6 Because Case 2 was only 11 months old and non-verbal when he initially exhibited self-injurious behavior, dysesthesia could not be excluded. Anticonvulsants and antidepressants are commonly used to manage dysesthesia.7 Therefore, carbamazepine or gabapentin was utilized in the management of self-injurious behavior in these three subjects (Cases 1, 2 and 3) with relatively good results. In all three of these individuals, self-injurious behavior recurred when the anticonvulsants were discontinued and resolved when therapy was restarted. In addition to the anticonvulsant therapy, the self-injurious behavior in two of the subjects responded temporarily to protective wrapping (Case 2) and counseling (Case 3).
The fourth case differed from the other three cases in that the self-injurious behavior appeared to be related to poor technique in positioning of the hand in the presence of insensitivity to pain. In this later case, the self-injurious behavior resolved completely after relatively straightforward non-pharmacological interventions. Similar to the two adults with SCI described by Dahlin et al2 three of our subjects (Cases 1, 3 and 4) were self-conscious of their self-mutilation, despite continued self-injurious behavior.
The majority of literature on self-injurious behavior relates to individuals with developmental delays.1 In particular, self-injurious behavior has been well described in children with Lesch-Nyhan syndrome.8,9,10,11 In addition to the reports of self-injurious behavior in the three adults with SCI and the two children with myelomeningocele, self-injurious behavior has been described in other conditions with normal cognition, such as congenital insensitivity to pain.12 In their report of two adults with SCI and self-injurious behavior, Dahlin et al2 provide a comprehensive review of this disorder, including pathogenesis and management.
The cause of self-injurious behavior has not been clearly defined in individuals with or without developmental disabilities. In their report of two subjects with tetraplegia, Dahlin et al2 ascribed the self-injurious behavior to depression, anxiety and incessant nail biting that predated the SCI. Some investigators have suggested that neurotransmitters or neuroreceptors, such as serotonin or dopamine, may be involved in the pathogenesis of this behavior.11,13
In individuals with spinal cord disorders, self-injurious behavior may represent a response to dysesthesia. In one of the reports of self-injurious behavior in a child with myelomeningocele, symptoms consistent with dysesthesia were present.5 The self-injurious behavior in this child responded to treatment with anticonvulsants and antidepressants. In one of the two adults with SCI described in the report by Dahlin et al,2 the self-injurious behavior responded to phenytoin, although there was no mention of symptoms consistent with dysesthesia. Our current report supports the potential role of dysesthesia in self-injurious behavior because of symptoms described in two of our patients and the response of the self-injurious behavior to anticonvulsants in three of the subjects.
Self-injurious behavior has been managed with physical and behavioral interventions, counseling and medications. Physical interventions have included orthotics, bandaging, gloves, or restraints that protect the body part from continued damage.2,8,9 More drastic measures such as tooth guards or extraction of teeth may be required in more resistant cases of self-injurious behavior, such as in children with Lesch–Nyhan syndrome.8,9 The application of aversive agents, such as Tabasco sauce, to the injured body part has also been successfully utilized.4 Behavioral and psychological interventions have also been utilized with variable success in children with and without developmental delays.4,5,8,14
A variety of medications have been utilized with variable success in the management of self-injurious behavior in individuals with and without developmental delays. Droperidol has been demonstrated to be effective in individuals with developmental delays; however, because of Parkinsonian side-effects, orphenadrine or benzhexol were also used.15 Subjects with Lesch–Nyhan syndrome demonstrated resolution of self-injurious behavior when treated with 5-hydroxytryptophan but became tolerant to the medication within 3 months.11 Anticonvulsants have also been beneficial in the management of self-injurious behavior in individuals with developmental delays.8 Lastly, antidepressants have demonstrated some efficacy in the management of self-injurious behavior in both patients with developmental delays11 as well as those with spinal cord disorders with normal cognition.5
The natural history of self-injurious behavior in individuals with and without developmental delays is characterized by its chronicity and tendency for recurrence.2,3,4,5 Although our first three cases all responded to anticonvulsant therapy, they experienced relapses when they discontinued their medication. It is particularly interesting that Case 2 experienced an exacerbation of his self-injurious behavior when he was hospitalized for pneumonia, despite the fact that he was on carbamazepine. All four of our patients had persistent disfiguring scars, which included nail bed ablation and obliteration of the nipples. An adult with tetraplegic SCI reported by Marmolya et al3 exhibited radiographically significant osteolysis of the terminal phalanges of both hands.
Conclusion
Although uncommon, self-injurious behavior can occur in children and adolescents with SCI. Self-mutilation of the fingertips was the most common manifestation of the self-injurious behavior in this report. However, one of our patients exhibited damage to his nipples, which has not been previously described. This report provides evidence that dysesthesia may be a common underlying cause of self-injurious behavior in individuals with SCI. Treatment with anticonvulsants, such as phenytoin, carbamazepine or gabapentin, may be beneficial for those individuals with self-injurious behavior accompanied by symptoms consistent with dysesthesia. Because antidepressants are useful in treating neuropathic pain, antidepressants may also be beneficial in those individuals with self-injurious behavior associated with dysesthesia.16
Similarly, treatment with anticonvulsants or antidepressants should be considered for patients with no identifiable cause of the self-injurious behavior. This approach may also apply to infants and younger children who may not be able to express symptoms consistent with dysesthesia. Lastly, counseling and conservative physical measures, such as soft dressings, should be considered for all patients with SCI who exhibit self-injurious behavior.
References
Hall S, Oliver C, Murphy G . Early development of self-injurious behavior: an empirical study Am J Ment Retard 2001 106: 189–199
Dahlin PA et al. Self-biting with multiple finger amputations following spinal cord injury Paraplegia 1985 23: 306–318
Marmolya G, Yagan R, Freehafer A . Acro-osteolysis of the fingers in a spinal cord injury patient. A case report Spine 1989 14: 137–139
Altman K, Haavik S, Higgins ST . Modifying the self-injurious behavior of an infant with spina bifida and diminished pain sensitivity J Behav Ther Exp Psychiatry 1983 14: 165–168
Arons MS, Lattanzi WE, Levy LL, Rifkin B . Severe self-mutilation of hands in a nonpsychotic, nonretarded patient Plast Reconstr Surg 1984 74: 282–286
Siddall PJ, Taylor DA, Cousins MJ . Classification of pain following spinal cord injury Spinal Cord 1997 35: 69–75
Bowsher D . Central pain following spinal and supraspinal lesions Spinal Cord 1999 37: 235–238
Anderson LT, Ernst M . Self-injury in Lesch-Nyhan disease J Autism Dev Disord 1994 24: 67–81
Christie R et al. Lesch-Nyhan disease: clinical experience with nineteen patients Dev Med Child Neurol 1982 24: 293–306
Hall S, Oliver C, Murphy G . Self-injurious behavior in young children with Lesch-Nyhan syndrome Dev Med Child Neurol 2001 43: 745–749
Nyhan WL, Johnson HG, Kaufman IA, Jones KL . Serotonergic approaches to the modification of behavior in the Lesch-Nyhan syndrome Appl Res Ment Retard 1980 1: 25–40
MacEwen GD, Floyd GC . Congenital insensitivity to pain and its orthopedic implications Clin Orthop 1970 68: 100–107
Goldstein M, Anderson LT, Reuben R, Dancis J . Self-mutilation in Lesch-Nyhan disease is caused by dopaminergic denervation Lancet 1985 1: 338–339
Iwata BA et al. The functions of self-injurious behavior: an experimental-epidemiological analysis J Appl Behav Anal 1994 27: 215–240
Burns ME . Droperidol in the management of hyperactivity, self-mutilation and aggression in mentally handicapped patients J Int Med Res 1980 8: 31–33
McQuay HJ et al. A systematic review of antidepressants in neuropathic pain Pain 1996 68: 217–227
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vogel, L., Anderson, C. Self-injurious behavior in children and adolescents with spinal cord injuries. Spinal Cord 40, 666–668 (2002). https://doi.org/10.1038/sj.sc.3101377
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101377