Abstract
Study design: Retrospective study.
Objective: To determine if spinal cord injuries due to gunshot wounds (GW) are associated with different bladder and sphincteric behavior compared to other trauma mechanisms.
Setting: Spinal injury center, Brazilian university hospital.
Methods: We retrospectively evaluated the records and urodynamic studies of 71 patients with spinal cord injury (SCI) referred to the Brazilian National Spinal Cord Injury Center over the year 2000, and compared the bladder-sphincteric pattern of patients with injuries caused by GW with those caused by other trauma mechanisms.
Results: The causes of SCI were (1) gunshot wounds (31 patients: 43.7%); (2) motor vehicle accidents (16 patients: 22.5%); (3) falls (16 patients: 22.5%) and (4) diving (three patients: 4.2%). In five patients (7.1%) the causes were unusual trauma mechanisms like stab wound (one patient) and direct trauma in vigorous sports (two patients) or fights (two patients). The levels of the injuries were cervical in 22 patients (31.0%), thoracic in 39 (54.9%) and lumbar in 10 (14.1%). Detrusor hyperreflexia with detrusor–sphincter dyssynergia was present in 65% of the patients overall and in 76% of the thoracic gunshot wounded. Areflexia occurred in 20% of the patients and in 16% of thoracic injured patients with gunshots. Detrusor hyperreflexia with detrusor–sphincter dyssynergia was the pattern encountered in 50% of the individuals suffering from SCI because of other mechanisms and areflexia was present in 35.8%. There was no statistical difference between GW patients and other mechanisms according to bladder and sphincter functions.
Conclusions: There was a substantial overlap of bladder and sphincteric behaviors between patients with different levels of spinal injuries, but the trauma mechanism was not important to determine the bladder and sphincteric functions.
Similar content being viewed by others
Introduction
Trauma to the spinal cord is usually associated with bladder and sphincteric dysfunction. Depending on the level of the injury, different bladder and sphincteric behaviors may be found. Many patients with spinal cord injury (SCI) suffer multiple injuries or multiple levels of spinal injury, and occasionally occult brain damage, all of which may have an adverse effect on bladder function. Moreover, spinal lesions may be complete or incomplete. As a result, the clinical neurological examination alone is not an adequate parameter to predict neurourological dysfunction and most specialists agree that urodynamic evaluation is necessary to determine the neurourologic status.1,2,3
The trauma mechanism may be important to determine the extension of the spinal cord lesion. In most series in the literature, the main causes of SCI are motor vehicle accidents and falls.4 In the last decade, however, gunshot wounds are becoming increasingly important as a cause of SCI, specially in big urban centers.5 Gunshot wounds are a high energy source of trauma. Tissue damage occurs from the concussive effect of the bullet and cavitation, which correlates with its kinetic energy.6 In addition, a bullet or a fragment of a projectile can cause damage without direct contact with the tissue, because of burning and ischemic effects.
The Brazilian National Spinal Cord Injury Center is located in São Paulo, one of the most violent cities in the world. Gunshot wounds are the main cause of spinal cord injury among our patients. As mentioned before, this population may have different clinical outcomes associated with their higher energy trauma mechanism. In this study, we analyze the bladder and sphincteric pattern in spinal cord injured patients caused by gunshot wounds and compare it with patients with SCI due to other trauma mechanisms.
Patients and methods
We retrospectively evaluated the records and urodynamic studies of 71 patients (58 males and 13 females; mean age 28, range 16 to 64 years) with SCI referred to our center from January to December 2000, and determined the trauma mechanism and level of the SCI using the Frankel system to classify the completeness of the injury. Forty-eight patients (67.6%) in the study were classified as Frankel A and 33 patients (32.4%) had incomplete injuries and were classified as Frankel non A. None of these were Frankel E.
Multichannel urodynamics consisting of cystometry and pressure/flow studies was performed after spinal shock phase in all patients. The interval between the trauma and urodynamic evaluation varied from 2 months to 2 years (mean 7 months). The urodynamic evaluation was performed in the supine or sitting position, using two 4-F catheters inserted transurethrally into the bladder. Intra-abdominal pressure was measured with a rectal balloon catheter. Saline at room temperature was instilled through one of the catheters at a constant rate of 30 ml/min. Intravesical pressure was measured through the other catheter. Detrusor pressure was calculated electronically. Pelvic floor electromyography was performed using surface electrodes. Detrusor hyperreflexia was defined as involuntary detrusor contractions of >15 cmH2O. All other definitions conform to the standardized terminology of the International Continence Society.7
Gunshot wounds (GW) and bladder behavior
According to the urodynamic studies, patients were categorized in three groups: (1) detrusor hyperreflexia with external sphincter dyssynergia; (2) detrusor hyperreflexia without external sphincter dyssynergia and (3) detrusor areflexia. To determine whether patients with SCI caused by GW have different bladder and sphincteric behaviors we compared the urodynamic findings of these patients with those of patients with other trauma mechanisms.
Statistical analysis
Data were analyzed using SISA (Simple Interactive Statistical Analysis) software. A Fisher's two by five test was used with a P value less than 0.05 for two-sided probability was considered statistically significant.
Results
The causes of SCI were (1) gunshot wounds (31 patients: 43.7%); (2) motor vehicle accidents (16 patients: 22.5%); (3) falls (16 patients: 22.5%) and (4) diving (three patients: 4.2%). In five patients (7.1%) the causes were unusual trauma mechanisms like stab wound (one patient) and direct trauma in vigorous sports (two patients) or fights (two patients).
The levels of the injuries were cervical in 22 patients (31.0%), thoracic in 39 (54.9%) and lumbar in 10 (14.1%). Table 1 shows the trauma mechanism and the level of injury in our patients.
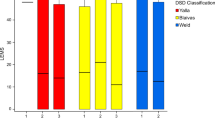
Urodynamic studies revealed detrusor hyperreflexia with detrusor–sphincter dyssynergia (DESD) in 46 patients (64.8%); detrusor hyperreflexia without dyssynergia (DH) in eight (11.2%) and detrusor areflexia (DA) in 14 (19.7%). Three patients had normal bladder and sphincteric functions (4.2%). These findings are demonstrated in Table 2.
Gunshot wounds and bladder behavior
For the comparison of the bladder behavior between patients with SCI caused by GW and other trauma mechanisms we excluded the lesions at the cervical and lumbar levels because of the reduced number of GW patients with lesions at these levels (Table 1). Patients with thoracic injuries had similar ages and gender distribution in comparison with the rest of the patients, comprising 34 men and five women with a mean age of 27, range 17–56 years. The mean ages for the GW patients and the other mechanism group was 27 and 29 years, respectively. The prevalence of complete injuries among the patients with thoracic lesions was similar in both groups, with 16 patients (64.0%) of the GW group and eight (57.1%) with other trauma mechanisms having complete spinal cord injury classified as Frankel A. Analyses of the patients with thoracic lesions demonstrated DESD in 19 patients (76.0%) with gunshot wounds and in seven patients (50%) of the other mechanisms group. DH occurred in two patients (8%) and one patient (7.1%) and DA occurred in four patients (16.0%) and five patients (35.8%), respectively, for the gunshot and other mechanisms groups. There were no statistically significant differences between the two groups in terms of bladder and sphincter patterns (P=0.18). The data are depicted in Table 3.
Discussion
Because of the complexity of SCI patients, the patterns of bladder and sphincteric behavior after injury cannot be predicted accurately based solely on the neurological examination and the level of trauma.1,2,3 Urodynamics is important to define the bladder pattern in these patients and may be instrumental in defining the prognosis and therapeutic options.
Kaplan et al analyzed the results of 489 consecutive patients with spinal cord lesions of varying causes and ascertained the relationship between bladder and sphincter functions and neurological deficits.2 They found three general urodynamic patterns after SCI, including (1) detrusor hyperreflexia with detrusor–external sphincter dyssynergia (DESD); (2) detrusor hyperreflexia without DESD (DH) and (3) detrusor areflexia (DA). Despite the predominance of DA in lumbar injuries and of DH (with or without DESD) in thoracic and cervical injuries, each bladder pattern occurred in patients with SCI at any level.
In our study, we found similar results. Detrusor hyperreflexia with DESD was present in the majority of patients with cervical and thoracic lesions but DA occurred in one (4.5%) and nine (23.1%) patients with cervical and thoracic injuries, respectively.
Although spinal cord injuries caused by GW may have distinctive clinical features, few studies have compared the differences between patients with SCI caused by gunshot and other trauma mechanisms.8,9 Even though GW are a high energy trauma mechanism, SCI caused by gunshot infrequently produces head injuries, spine instability, and vertebral fractures requiring surgical treatment, which are frequent in patients with SCI caused by other trauma mechanisms such as falls and car accidents.6 Orthopedic surgical procedures to the spine, which are frequently necessary in these patients, are usually unnecessary in patients with gunshot injuries.8 On the other hand, the kinetic energy and the cavitation effect associated with the bullet can cause great tissue damage and expand spinal injury. Furthermore, associated life-threatening injuries and blood loss are common and may lead to a delay of the rehabilitation process.
To our knowledge, there were no previous studies concerning the effects of the trauma mechanism on the bladder and sphincter functions in patients with SCI. We found no differences in the bladder and sphincter behaviors of patients with SCI caused by GW compared to patients with injuries caused by other mechanisms. In patients with thoracic lesions, detrusor hyperreflexia occurred in at least 50.0% of the patients in each group. Areflexia was present in 16.0% of the GW group and in 35.8% of the other mechanisms.
Our results are in agreement with previous reports and confirm that although the level of injury is the more important factor determining the bladder and sphincteric patterns in patients with SCI, urodynamics are necessary to accurately define their behavior. The trauma mechanism does not seem to have a significant impact on the bladder behavior, but studies involving a larger population are needed to confirm this finding.
Conclusions
Although the level of spinal injury is an important factor determining the bladder pattern in SCI patients, there was a substantial overlap of bladder and sphincteric behaviors between patients with different levels of spinal injuries, but the trauma mechanism was not an important factor to determine the bladder and sphincter behaviors.
References
Watanabe T, Rivas DA, Chancellor MB . Urodynamics of spinal cord injury. Urol Clin North Am 1996; 23: 459–473.
Kaplan SA, Chancellor MB, Blaivas JG . Bladder and sphincter behavior in patients with spinal cord lesions. J Urol 1991; 146: 113–117.
Wyndaele JJ . Correlation between clinical neurological data and urodynamic function in spinal cord injured patients. Spinal Cord 1997; 35: 213–216.
Gutierrez PA, Young RR, Vulpe M . Spinal cord injury. An overview. Urol Clin North Am 1993; 20: 373–382.
Yoshida GM, Garland D, Waters RL . Gunshot wounds to the spine. Orthop Clin North Am 1995; 26: 109–116.
Isiklar ZU, Lindsey RW . Gunshot wounds to the spine. Injury 1998; 29(Suppl 1):SA7–S12.
Abrams P, Blaivas JG, Stanton SL, Andersen JT . The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol 1988; 114: 5–19.
Waters RL, Adkins RH . Firearm versus motor vehicle related spinal cord injury: preinjury factors, injury characteristics, and initial outcome comparisons among ethnically diverse groups. Arch Phys Med Rehabil 1997; 78: 150–155.
McKinley WO, Johns JS, Musgrove JJ . Clinical presentations, medical complications, and functional outcomes of individuals with gunshot wound-induced spinal cord injury. Am J Phys Med Rehabil 1999; 78: 102–107.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sacomani, C., Trigo-Rocha, F., Gomes, C. et al. Effect of the trauma mechanism on the bladder-sphincteric behavior after spinal cord injury. Spinal Cord 41, 12–15 (2003). https://doi.org/10.1038/sj.sc.3101354
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101354